1. Background
Despite the remarkable advances in their prevention, diagnosis, treatment, and rehabilitation, cardiovascular diseases are still regarded as the leading cause of mortality in many countries (1), and arrhythmia is responsible for a significant percentage of these mortalities (2). Using a pacemaker, which is an electronic device used when the heart is unable to generate an effective electrical impulse to initiate contraction and maintain cardiac output, is one of the ways to control and treat Bradyarrhythmias (3). A temporary transvenous cardiac pacemaker (TTCP) is one of the various types of pacemakers whose first successful application was reported by Tancredi et al. in 1967. A temporary transvenous cardiac pacemaker was proposed as a life-saving treatment for patients with serious arrhythmias (4). This technique is used to treat symptomatic bradycardia and different types of symptomatic cardiac blockages (5). Additionally, when a permanent pacemaker is unavailable or impossible to implant, this temporary treatment can be used to bridge the gap until a permanent pacemaker becomes available (4).
Following the insertion of a temporary pacemaker, patients are often exposed to complications caused by the procedure and other problems. The complications observed have been related to the venous lead (e.g., lead dysfunction and cardiac perforation), venous access, or the need to remain physically still so as to prevent the development of other complications, such as bleeding, infection, and thrombosis, especially in older individuals, and psychological problems, such as delirium (6-9). In addition to causing problems for the patients, these complications lead to re-intervention and prolonged hospitalization. Moreover, a second procedure is often required to insert a permanent pacemaker after the temporary one, approximately a week following the insertion of the temporary pacemaker, thereby prolonging the treatment process (8). Meanwhile, there are only general care guidelines for these patients, and the details have not been seriously examined, particularly from the patients’ point of view (10).
Various studies have argued that investigating the experiences of patients with pacemakers is the first important step toward developing effective interventions (11, 12). In their study, Timmins and Kaliszer argued that nursing care could only be effective when it is based on the patients' experiences of the disease and their perception of their own needs (13). In another qualitative study on the experiences of patients with pacemakers, Hallberg and Malm cited in Speziale et al. stated that understanding the patients’ experiences can contribute to their social and psychological rehabilitation (14). Therefore, similar to most clinical interventions, effective nursing care for patients with temporary pacemakers should be unique, based on the patients' experiences and needs, and compatible with their conditions (15). Meanwhile, studies conducted on this subject have been mostly quantitative and have investigated pacemaker insertion techniques (16), training (17), and complications and consequences (4, 18), while the challenges experienced by these patients have remained unexamined. It should be noted that the experiences of these patients can only be explored through qualitative research (13) since qualitative studies clarify participants’ knowledge of a phenomenon, enable the comprehension of the issue, and provide new insights into the subject of study (14).
The evidence about patients' experiences and challenges is limited, and a significant number of studies date back to 40 years ago. Moreover, it is unclear how these results will translate into current clinical practice (4). On the other hand, the mortality rate in patients who need TTCP is high (about 15%) (18), and due to the lack of alternative treatments, this treatment is currently unavoidable. Furthermore, about 65% of patients after TTCP need a permanent pacemaker, which increases the rate of infection in these patients up to 2.5 times (19). Therefore, it seems that conducting a qualitative study to explore experiences and challenges and to understand and identify care needs from the perspective of patients with rich experiences can be a fundamental step in reinforcing the evidence in this area.
2. Objectives
This study was performed to discover the challenges experienced by Iranian patients with TTCP.
3. Methods
3.1. Study Design
The present qualitative, interpretive phenomenology study was conducted to explore the challenges experienced by patients with temporary cardiac pacemakers based on the six steps proposed by van Manen. According to van Manen, phenomenology provides researchers with a systematic approach to studying and interpreting a phenomenon (20). This type of study is applied when the researcher needs to elucidate a lesser known or unknown phenomenon through the in-depth investigation of the lived experiences of individuals affected by that phenomenon (21).
3.2. Participants and Study Setting
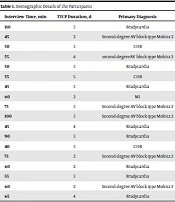
A total of 18 patients undergoing temporary cardiac pacemaker insertion entered the study by purposive sampling. Patients were interviewed during the time they had TTCP in place. The study setting consisted of two hospitals affiliated with Urmia University of Medical Sciences, Urmia, Iran, that admit these patients. Visiting the cardiac care wards in the selected hospitals enabled the acquaintance of the eligible patients, who were then selected for participation in the study. The study inclusion criteria were willingness to take part in the study, ability to establish communication and express one’s experiences, a minimum of 48 hours of TTCP use, and femoral access vein. Patients without rich experiences and those who did not provide the researcher with complete information were excluded from the study. Table 1 shows the participant’s characteristics.
| Interview Time, min | TTCP Duration, d | Primary Diagnosis | Marital Status | Education Level | Gender | Age, y | ID |
|---|---|---|---|---|---|---|---|
| 110 | 3 | Bradycardia | S | High school dropout | Male | 70 | P1 |
| 45 | 2 | Second-degree AV block type Mobitz 2 | M | High school diploma | FM | 58 | P2 |
| 50 | 3 | CHB | M | High school dropout | Male | 64 | P3 |
| 55 | 4 | second-degree AV block type Mobitz 2 | M | High school diploma | FM | 48 | P4 |
| 50 | 3 | Bradycardia | M | High school dropout | FM | 66 | P5 |
| 55 | 5 | CHB | M | High school dropout | Male | 51 | P6 |
| 45 | 3 | Bradycardia | M | High school dropout | Male | 78 | P7 |
| 60 | 2 | MI | M | High school dropout | FM | 70 | P8 |
| 75 | 3 | Second-degree AV block type Mobitz 2 | M | High school dropout | FM | 72 | P9 |
| 100 | 3 | Second-degree AV block type Mobitz 2 | S | Higher education | FM | 48 | P10 |
| 45 | 4 | Bradycardia | M | High school diploma | FM | 68 | P11 |
| 90 | 3 | Bradycardia | M | High school dropout | Male | 55 | P12 |
| 40 | 3 | CHB | S | High school dropout | Male | 69 | P13 |
| 75 | 2 | Second-degree AV block type Mobitz 2 | M | High school dropout | FM | 60 | P14 |
| 60 | 2 | Bradycardia | M | Higher education | FM | 58 | P15 |
| 55 | 3 | Bradycardia | M | High school diploma | Male | 60 | P16 |
| 60 | 2 | Second-degree AV block type Mobitz 2 | M | Higher education | FM | 51 | P17 |
| 65 | 4 | Bradycardia | M | High school dropout | Male | 62 | P18 |
Demographic Details of the Participants a
3.3. Data Collection
The data were collected using in-depth semi-structured face-to-face interviews. A total of 20 interviews were conducted with 18 participants. After obtaining the patients’ demographic details, the interviews began with open-ended questions, such as “How come you had a pacemaker inserted?” and “What happened during, before, and after the insertion of the pacemaker?” and then steered to exploratory questions, such as “What was your experience of the temporary cardiac pacemaker?”, “Describe the challenges and problems you faced during hospital admission and pacemaker insertion”, and “What is your life like with a temporary cardiac pacemaker?”. Probing questions were then asked to obtain greater richness, such as “Please elaborate on this”, “What do you mean by that?”, and “Could you give us an example?”
With their consent, the patients’ voice was recorded. Interviews with the patients who did not consent to the voice recordings (two patients) were written down manually. The interviews were conducted using Turkish and Farsi and then translated into English by an English-speaking person. Each interview was transcribed on paper at the first opportunity. The corresponding author listened to the interviews and reviewed the transcriptions several times. The views of all the research team members were implemented and confirmed. The duration of the interviews was based on each patient’s ability to cooperate, and each interview lasted 60 minutes on average (minimum of 40 and maximum of 110 minutes). The interviews were conducted at the hospital in each patient’s ward of admission and continued until the saturation of data. The non-emergence of new codes in the last two interviews was taken to indicate data saturation, and a total of 18 interviews were ultimately conducted.
3.4. Data Analysis
The data were analyzed using van Manen’s six-step method (20). His two holistic and selective approaches were used to separate thematic sentences and extract themes. According to this method, the text of the interviews was transcribed and reviewed several times by the corresponding author to confirm its accuracy and to gain a general understanding of it. Then, the general understanding gained from the text was written down in two or three paragraphs, which helped the researcher to immerse himself in the data. Then, the text of each interview was read several times, and sentences and phrases that seemed to describe the nature of the phenomenon or reveal it were selected, and themes were extracted. In the analysis process, the research team went over these steps several times and exchanged views on extracting topics and themes. In order to resolve any discrepancies and inconsistencies in the interpretations, the process of returning to the texts continued regularly and repeatedly until the resulting themes were connected in the best possible way. Finally, the main themes emerged through these frequent forward and backward reviews, and 13 subthemes and 3 themes were obtained.
3.5. Rigor
To confirm the trustworthiness of the data, Lincoln and Guba's cited in Speziale et al. evaluative criteria, including credibility, reliability, confirmability, and transferability, were employed (14). Credibility was achieved through an appropriate rapport and close interaction with the participants. The interview texts were given to the participants, and their views were implemented. Through prolonged engagement with the data, all the stages of the study were reviewed by the research team, and their views were also implemented. Moreover, the participants were selected with the maximum diversity possible. For reliability, all the stages of the study were reviewed by the research team and externally checked (by someone familiar with qualitative research and clinical settings) through discussion. These views were implemented for all the stages, and the results were confirmed. To ensure confirmability, the study stages were documented for availability to and use by others in the future. All the study stages were accurately described so as to enable the application of the research findings in other societies with similar characteristics and to achieve transferability.
4. Results
A total of 18 patients with TTCP hospitalized in the hospitals of Urmia, Iran, who had the greatest information about the research phenomenon, took part in this study. They comprised 10 females and 8 males, with 15 married and 3 single, and their mean age was 61.55 years (mean ± SD = 61.55 ± 9.2). The analysis of the data obtained from the interviews with the patients produced 13 subthemes and three themes, as shown in Table 2.
4.1. Theme 1: Disregard for Patient’s Dignity
Respecting the patients’ dignity is one of the crucial ethical concepts in nursing and a basic patient right. In the present study, the patients had experienced disregarding of their rights, privacy, and values in various ways. This theme included three subthemes: Disregard for patients' rights, lack of privacy, and disregard for patients' values.
4.1.1. Disregard for Patient’s Rights
Occasionally, some measures intended to help the patients would threaten their personal independence. The patients had experienced this threat in different ways, such as not having the right to choose and not having permission to go to the bathroom without other individuals’ help. One of the patients said:
“I was taken to the operating room as soon as I went into the hospital. I had no idea what they were going to do at all. No one explained things fully to me as if I had no right to make comments or choice treatments.” (P2, female, 58 y)
4.1.2. Lack of Privacy
Most patients considered physical contact without permission, not receiving care by same-sex personnel, and disregard for their preferred clothing as a violation of their personal identity. One of the male patients explained:
“A female physician came to my bedside, pushed my clothes aside, and placed her stethoscope on my thigh at the site of the lead insertion without asking for my permission. It was very disturbing because I was not ready to be touched at all.” (P3, male, 64 y)
Additionally, most patients stated that their privacy had not been respected in the hospital, their anxiety had elevated, and their security needs had not been met. They considered the disrespect for their personal space and their exposure to other individuals as a violation of their personal security. One of the patients described:
“My room was not like a private room. There were curtains, but the nurses would not allow them to be closed either. I could be seen by everyone, and it was disturbing since I did not have proper clothing, so I felt insecure.” (P10, female, 48 y)
4.1.3. Disregard for Patient’s Values
While undergoing treatment with a temporary cardiac pacemaker, the patients were faced with conflicts that were not within the framework of their previous values and experiences, which annoyed them. Religious matters were among the patients’ foremost priorities, and performing religious duties, such as saying prayers, was one of its components. One of the patients explained:
“My body was in blood, and it was not right to say prayers like that. Moreover, they would not allow me to sit down, saying it would disconnect the lead. I had to say my prayers, but no one cared or helped. They kept telling me to be careful with the lead.” (P6, male, 51 y)
Additionally, cultural diversity among the patients was another issue. The patients cared a lot about their own culture; however, the values ruling the ward were sometimes in conflict with the patients' cultural priorities. A patient explained:
“I am a Kurd, and in our culture, the entire family comes to visit when someone falls ill. But they do not allow my family to come visit me here. When I protested, they said they could not allow so many visitors for each patient.” (P7, male, 78 y)
Another patient said:
“I have to wash up each time after going to the bathroom, but they do not let me do it here; they say that I must get used to it, which is very difficult for me.” (P15, female, 58 y)
4.2. Theme 2: Dependent Life
One of the experiences discussed by the patients was the sense of dependence, which was not pleasant for them; in brief, they felt they were not themselves. This theme consisted of two subthemes, including depending on others and depending on the pacemaker.
4.2.1. Depending on Others
After treatment with the pacemaker, the patients felt the burden of dependence on others and disclosed their experiences. Dependence on the wife, children, and nurses was not pleasant for them. One of the patients said:
“After this illness, I can no longer get my medications myself, and my children and wife have to help me. My wife has grown old, and the children have to help, but poor things, they are busy themselves” (P1, male, 70 y)
Another patient said:
"From now on, I became dependent on my children, and I could not do my work without their help. This bothers me. I do not want to be a burden on them."(P9, female, 72 y)
4.2.2. Depending on the Pacemaker
The patients regarded the pacemaker as a donated heart that had saved their lives for now, and therefore, their lives depended on the pacemaker’s functioning. They had, therefore, become very sensitive about its proper functioning. A patient told us:
“I kept watching the nursing station to see if the nurses were paying any attention to my pacemaker or not because I would die if it did not function well. My life is now dependent on the proper functioning of this device.” (P4, female, 48 y)
4.3. Theme 3: Physical and Psychological Problems
Despite saving their life, the patients also experienced many problems with TTCP. With regard to physical and psychological problems, they pointed out issues that made up the following subthemes: Back pain, problems related to the legs, constipation caused by immobility, fear, anxiety, life in prison, wishing to return to normal life, and a disturbed outlook.
Back pain: This subtheme describes how the patients experienced pain in the course of the treatment. Most patients complained about their backache. One of them described his experience of pain as follows:
“My back ached all the time for lying on my back, and the pain was very severe. If there was a kind nurse in the shift, she would give me a painkiller to relieve the pain a bit; otherwise, the back pain would kill me.” (P13, male, 69 y)
Problems related to the legs: Other physical complications experienced by the patients were problems related to the legs. A patient described his experience:
“They bandaged my legs every morning as I woke up; as if they were bandaging a corpse. It made me feel bad, but they said they had to bandage my legs.” (P8, female, 80 y)
In addition, the immobility of the lower extremities due to restrictions caused numbness in the patient's legs. A patient described:
"Both my legs had become numb since I was told not to move them. I thought I had no limbs waist down, but they ached when I moved them.” (P11, female, 68 y)
Constipation due to immobility: The majority of the patients complained about constipation and recalled it as a bad and annoying experience. One patient explained:
“The thing that annoyed me most was constipation. I had not been to the bathroom for three days, and my stomach ached, and the medicine they gave did not work.” (P7, male, 78 y)
Fear: Patients, especially those with no previous experience of heart disease, had a sense of fear following their experience with the temporary pacemaker and gave various reasons for their fear, including fear of dying, fear of returning to the operating room, and fear of lead dislodgement. One of the participants said:
“When I went to the operating room and came back, I thought I would die. They had inserted a lead through my leg into my heart; how could I live after that? I was so afraid. I did not sleep that night until the morning.” (P5, female, 66 y)
Anxiety: Most participants had experienced pre-operative anxiety, which had been caused by their unfamiliarity with the procedure and delayed treatment. One of the participants said:
“When their work was finished in the emergency ward, they took me to the operating room, where I lied down on the bed for half an hour, and they said that the doctor had not arrived yet. The doctor’s late arrival had gotten me very anxious.” (P11, female, 68 y)
Another patient described:
“It was my first time seeing these, and I was very anxious. I had no idea what they were going to do.” (P10, female, 48 y)
Living in prison: The physical limitations caused by the temporary pacemaker lead inserted into their groin and the loss of freedom in personal affairs resembled life in prison for most patients. One patient explained:
“I was on my back the whole time, and they would not even let me sit up. I felt I was imprisoned. As soon as I wanted to turn to one side, they told me to lie on my back. It was very unpleasant.” (P4, female, 48 y)
Wishing to return to life quickly: The participants had accepted the insertion of the temporary cardiac pacemaker as a way of being saved from death and wished to recover as soon as possible to be able to return to their normal life. One participant said:
“I had no choice. I wished to be released from this situation, so I could get out of the bed, eat like I always did, and do my things as usual.” (P12, male, 55 y)
Disturbed outlook: A wide range of ambiguities and concerns about the future had mentally preoccupied the patients. A farmer patient explained:
“I kept thinking what would happen to my plots, and who would attend to them; the children would not. It is highly unlikely for me to be able to work again; that is, if I survive at all.” (P3, male, 64 y)
Another participant described:
"I am deeply worried. I do not know what the future will be like. I do not know if I will get well or if I will be involved in this disease. I have no hope for a good future."(P12, male, 55 y)
| Themes | Subthemes | Codes | Frequency |
|---|---|---|---|
| Disregard for the patient's dignity | Disregard for patient’s rights | Not being allowed to use the bathroom alone | 16 |
| Having no right to choose | 12 | ||
| Lack of privacy | Physical touch without permission | 25 | |
| Disregard for the patient’s preferred clothing | 21 | ||
| Not receiving patient care by same-sex personnel | 14 | ||
| Being in other individuals’ sight during the procedures | 16 | ||
| No respect for their private space | 14 | ||
| Disregard for patient’s values | Not being able to perform their religious duties | 31 | |
| Previous personal habits | 17 | ||
| Personal hygiene culture | 18 | ||
| Cultural diversity | 10 | ||
| Dependent life | Depending on others | Feeling dependent on the nurses | 19 |
| Dependent on the children | 18 | ||
| Dependent on the spouse | 18 | ||
| Depending on the pacemaker | Pacemaker as the pulse of life | 16 | |
| Sensitivity to the pacemaker’s functioning | 22 | ||
| Understanding the need for a pacemaker through Simulation | 9 | ||
| Physical and psychological problems | Back pain | Constant backache | 35 |
| Great back pain | 31 | ||
| Constantly being in the supine position and back pain | 35 | ||
| Severe back pain and receiving no treatment for it by nurses | 18 | ||
| Problems related to the legs | Feeling tightness in the groin at the site of lead insertion | 12 | |
| Pain in the operated leg after removing the lead | 14 | ||
| Pain in the groin during lead insertion | 18 | ||
| Numbness in the legs | 15 | ||
| Inflammation and having no sense in the legs | 13 | ||
| Numbness in the legs, especially in the operated leg | 11 | ||
| Having no sense in the lower limbs | 10 | ||
| Unpleasant feeling in the legs during the day caused by bandages | 23 | ||
| Assimilating their bandages to the way a corpse is wrapped | 17 | ||
| Leg bandaging as an imitation of death | 14 | ||
| The leg bandages are painful | 11 | ||
| Constipation caused by immobility | Having a tight stomach due to lack of bowel movement | 32 | |
| No bowel movement for 3 days | 27 | ||
| Stomachache due to lack of bowel movement | 25 | ||
| Stomachache caused by the inability to defecate on the bed | 22 | ||
| Fear | Fear of dying | 29 | |
| Fear of going back to the operating room | 18 | ||
| Fear of lead dislodgement | 22 | ||
| Anxiety | Anxiety caused by unfamiliarity with the procedure | 26 | |
| Anxiety due to delayed treatment | 13 | ||
| Living in prison | Imprisonment | 24 | |
| Annoying physical limitations | 26 | ||
| Wishing for a quick return to life | Wishing for recovery | 19 | |
| Hoping to recover with a pacemaker | 16 | ||
| Treatment acceptance | 15 | ||
| Disturbed outlook | Concern about the future | 17 | |
| Ambiguities about the future | 14 |
Themes and Subthemes
5. Discussion
The present study was conducted to explore the experiences of patients with temporary cardiac pacemakers using van Manen’s theme analysis approach. Three main themes emerged from the analysis of the data, as follows: disregard for the patient's dignity, dependent life, and physical and psychological problems. Although TTCP is only inserted for a few days, the patients encounter many problems during this time that require examination and attention. One of the problems disclosed by the patients was disregarding their dignity and lack of privacy in a variety of ways. The threat to their personal independence, other individuals touching them without their permission, their body’s exposure to other individuals, the lack of appropriate private space, the disregard for their preferred clothing, and receiving care by nurses of the opposite sex were some of the instances of the violation of the patient’s rights and privacy. Although previous studies conducted on patients’ privacy in clinical settings have yielded similar results and emphasized the importance of nurses’ own role in their ethical performance and in maintaining the patients’ privacy and independence (22-24), this issue has not been investigated with regard to patients with TTCP, demonstrating the disregard for these patients’ experiences.
Disregarding the patient's values was another important problem experienced by the participants that emerged during their treatment with TTCP. Due to certain conditions imposed by the disease and the inevitable restrictions, the patients were required to observe matters that were not within their value system and which mentally preoccupied them, leading to a clash between their value system and the clinical setting’s value system and making them annoyed and resentful. The patients gave priority to their own personal values, including religious values, personal hygiene, and previous habits; nevertheless, the hospital, especially the nurses, prioritized health values in giving care so that the patient's life would not be at risk. These conflicts can be largely resolved and the patients’ understanding of the circumstances can be improved by incorporating the patients’ needs into the process of care, ensuring that the patients’ problems are well understood, and reaching a common mentality. The outcome will then be improved patient cooperation, participation, and satisfaction.
Meanwhile, the patients’ resistance to complying with the nurses’ recommendations can be reduced by ensuring proper nurse training. There is an abundance of literature on the conflict between nurses and patients (25-28); however, none of these studies has dealt with the complexities and theoretical perspectives of conflict in relation to patients with TTCP inserted. Moreover, the literature review did not show any studies on the importance of patients’ preferences in this area, which shows the need for further research on the subject.
Feeling dependent on others was another unpleasant experience for the patients. They saw their life as dependent on the pacemaker and other individuals’ help. They understood that they had lost the normal functioning of their heart and viewed their life as dependent on others from then on. They carefully followed the pacemaker’s functioning and saw their continued survival dependent on the proper functioning of the pacemaker. They also envisioned a life of dependence on others, including their spouse and children, after their discharge. This finding indicates that therapeutic goals in these patients are not met by the implantation of a TTCP alone. To be successful in this field, there must always be patient control and regular patient education during care to accelerate the patient's return to normal life. There was a tangible need for supportive measures and interventions to improve their adaptation.
Che et al. (29) argued that adapting to the pacemaker is a challenging matter. The maladaptation of patients with a temporary pacemaker was evident since the failure to understand the patients’ experiences could be one of the causes of their maladaptation (30). The patients also had the worst ideas about life after discharge. In their study, Deaton et al. (31) argued that coming to terms with reality and accepting losses are inevitable. Therefore, patients should be directed toward greater adaptation to these circumstances through effective care programs. Various studies have also reported dependence on permanent pacemakers (15, 32).
Physical and psychological problems were another theme that emerged from data analysis, which included eight subthemes for these patients: Back pain, problems related to legs, constipation due to immobility, fear, anxiety, life in prison, wishing to return to normal life, and a disturbed outlook. The majority of the patients complained about their back pain and described it as occasionally very severe, in which case the palliative interventions provided by the nurses did not relieve the pain either. The patients’ other unpleasant experiences during the course of treatment included problems arising from immobility, such as numbness in the legs and constipation.
The physical complications and problems experienced by patients with TTCP have been addressed in various studies, and similar results have been obtained (6-9). Given the patients' statements in this study, despite its importance in saving their lives, TTCP also entailed psychological problems for the patients and sometimes made them unhappy and uncomfortable. Fear of death, fear of being sent back to the operating room, and fear of lead dislodgment in their leg were disturbing notions for them. Anxiety due to delayed treatment and unfamiliarity with the procedure were other problems faced by these patients.
Psychological symptoms can be the result of a lack of education and attention to patient’s needs and TTCP care. The results of the present study showed that patients have uncertainty and do not provide useful information that can indicate the importance of patient education. Although the psychological problems faced by patients with permanent pacemakers have already been investigated in the literature, it should be noted that the nature and origin of these issues differ for patients with TTCP (33, 34). Moreover, the limitations caused by the pacemaker insertion induced a sense of isolation and a perception of life in prison in these patients. Concern about the future was another issue that disturbed the patients’ outlook. Tagney et al. examined patients with implanted defibrillators and obtained similar results regarding these patients’ concerns about the future (15). In the present study, the patients revealed that they wished to return to normal life and get rid of the present state as soon as possible.
5.1. Limitations
The present study had some limitations. One limitation pertained to the selection of participants, as the coronavirus disease 2019 (COVID-19) outbreak had limited patient referrals and dispatch to medical centers. It is better to know that the identification and treatment of a large number of patients with COVID-19 has caused the health systems of many countries, including Iran, to be under unprecedented pressure and to go beyond their existing capacities to deal with this pandemic. Therefore, COVID-19 can affect the present study in factors, such as the duration of patient visits by their families, the concern of the medical staff about the infection, the reduction of the hospital's medical capacity to care for non-coronavirus patients, and the selection of participants. Moreover, the high prevalence of consciousness disorders and delirium in these patients meant that some of the patients had to be excluded from the study, especially those who had experienced physical restraints. Another limitation of this study was that only patients implanted with a femoral venous approach were included. This issue might be explained by the fact that the femoral venous approach method for pacemaker implantation is the most frequently used access site for TTCP in selected centers.
5.2. Conclusions
The present study reveals the important aspects of challenges experienced by Iranian patients with TTCP. This group of patients is facing challenges related to the care and hospitalization matter, as well as facing their fears and uncertain future. Therefore, there is a need to pay more attention to patients' needs during hospitalization, such as informing patients about the procedure and the probabilities in the future and respecting patients’ rights, values, and dignities. The patients found TTCP placement difficult due to physical problems, such as pain, that should be considered. Additionally, given that the patients' psychological strength is usually reduced during this procedure, it should be accepted that the dimension of the problem is not limited to the procedure as such but to other problems that emerge or the deeper needs of the patients. Future studies are also recommended to address the experiences of nurses providing care to these patients so that the results can be used to design comprehensive care plans.
5.3. Implications for Clinical Practice
(1) Nurses in clinical practices can improve the experience of patients with TTCP by treating all of them with equal kindness and concern when ill, respecting their dignity, rights, and values.
(2) Providing ongoing TTCP advice and access to nursing support and informing patients might facilitate patients to cope with the feeling of dependence.
(3) Many patients with TTCP described physical problems, such as back pain, problems related to legs, and constipation caused by immobility, and nurses can minimize these problems by providing appropriate care.
(4) The physical limitations and psychological challenges (i.e., fear and anxiety) caused by TTCP, in addition to threatening the patient's personal independence, instill a sense of isolation and imprisonment, which should be taken seriously in clinical settings and nursing care interventions.
(5) Most patients in this study found themselves suffering from a heart disease that they cannot easily get rid of and facing their fears and uncertainty, which necessitates more supportive measures and paying more attention.