1. Introduction
Atheroma is a disease affecting blood vessels, primarily forming at the junctions of moderate to large arteries, such as the carotid artery. Plaque formation causes the inner layer of the carotid vessel to thicken. This plaque consists of various cells, including monocytes, macrophages, lymphocytes, dendritic cells, smooth muscle cells, extracellular matrix, lipids, and calcium deposits (1). These plaques can rupture suddenly, leading to distant thrombosis and ischemic attacks, such as stroke and myocardial infarction (2).
Carotid atheroma can appear in panoramic views in two forms: As a round radiopaque area or as two radiopaque vertical lines with a distance of 1.5 to 4 cm, typically located at the border of the mandible or the posterior border of the mandible and anterior to the third and fourth cervical vertebrae (3).
Radiotherapy, while targeting tumor extension, also affects surrounding normal tissues. In head and neck radiotherapy, the oral mucosa, teeth, bone, and salivary glands respond differently. Acute changes include mucosal erythema, ulcers, reduced salivary secretion, damage to taste buds, and skin erythema and desquamation. Long-term effects involve reduced blood circulation in tissues leading to fibrosis (4).
Radiotherapy of the neck increases the thickness of the inner layer of the carotid artery (5), making atherosclerosis a relatively common complication following radiotherapy (6). Radiotherapy plays a crucial role in controlling head and neck cancers, with doses regulated based on the cancer's location and type. Most patients with head and neck cancer receive doses between 50 to 70 gray. Doses higher than 45 gray have been associated with carotid atheroma in previous studies (7).
Radiation-induced coronary heart disease is the second leading cause of death among patients receiving radiotherapy for breast cancer, Hodgkin lymphoma, and other mediastinal cancers (8). It has been shown that plaque formation is dose-dependent, with carotid atheroma being more severe in patients who received radiation for lymphoma (9).
Due to the severe cerebrovascular complications associated with radiotherapy in the neck region, this study investigated the incidence of carotid atheroma in patients who received radiation and were referred to the Dental Faculty of Semnan University, using panoramic views.
2. Case Presentation
Thirty-six patients were referred to the Oral Medicine Department of the Dental Faculty at Semnan University of Medical Sciences by a hematologist-oncologist. Following an evaluation of medical and dental histories and oral examinations, a panoramic radiograph was taken for each patient to screen for dental and surrounding bone diseases and to investigate carotid atheroma (CA).
All images were analyzed by an oral and maxillofacial radiologist, and four of these images showed opacities diagnosed as carotid atheroma. The patients with CA are listed below:
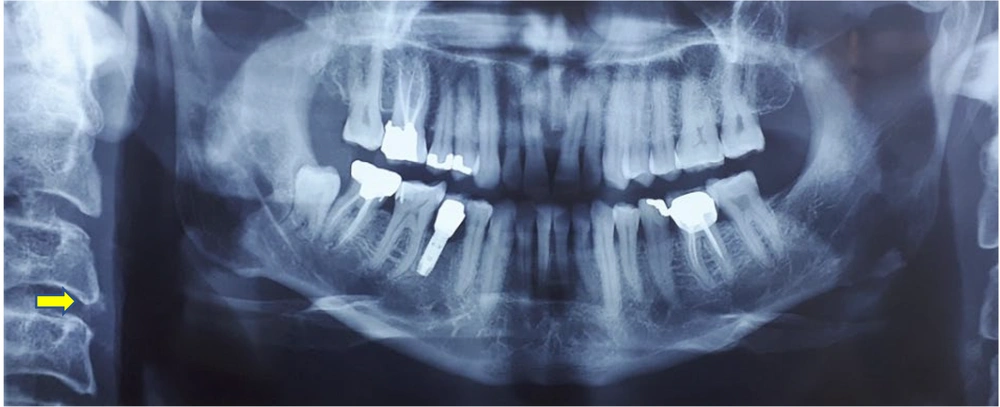
Case 1:
A 48-year-old man, weighing 78 kg and 175 cm tall, was diagnosed with nasopharyngeal cancer. He has no history of hyperlipidemia, diabetes, or hypertension. An X-ray taken 3 months after radiotherapy showed a single, almost round radiopaque area in front of the vertebral column between the third and fourth vertebrae, with a diameter of about 0.5 centimeters (Figure 1).
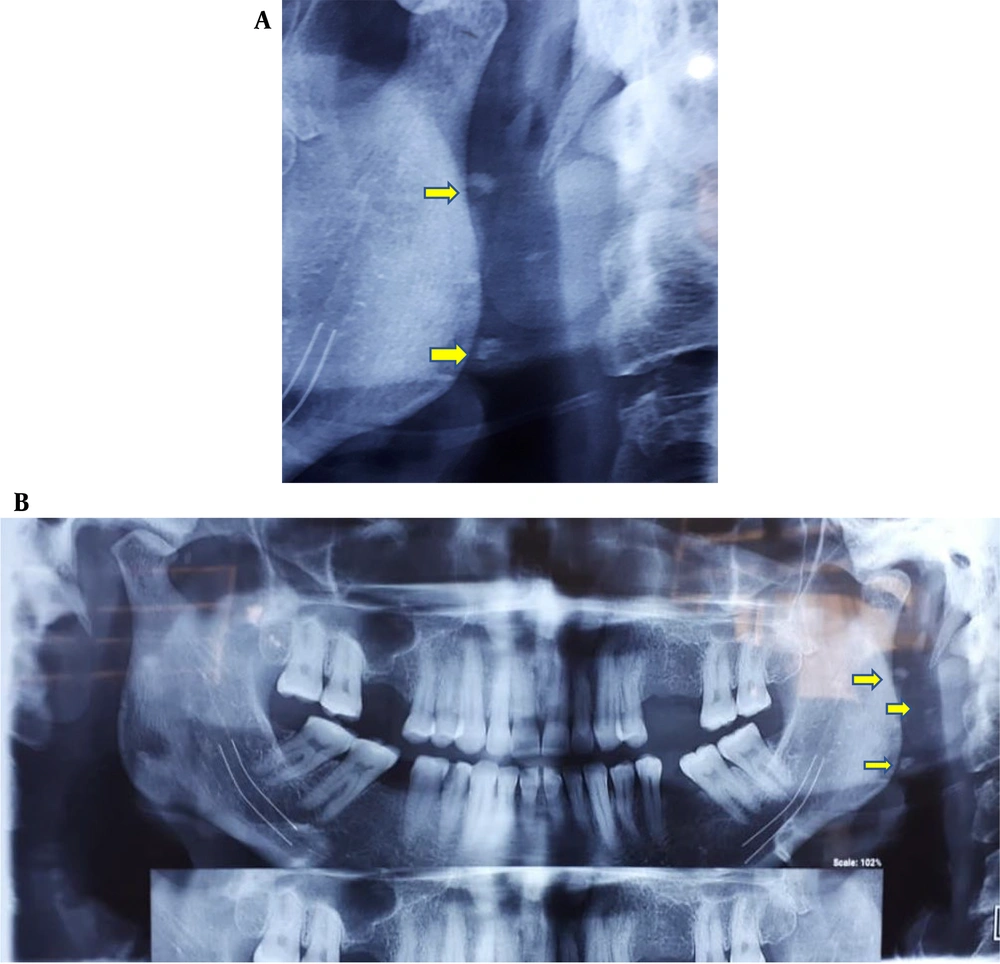
Case 2:
A 62-year-old woman, weighing 70 kg and 165 cm tall, with a history of hyperlipidemia, was diagnosed with breast cancer. She has no history of diabetes or hypertension. An X-ray taken 4 months after radiotherapy showed a radiopaque area (Figure 2).
Case 3:
A 39-year-old woman, weighing 65 kg and 159 cm tall, with a history of breast cancer and hyperlipidemia, was referred. She has no history of diabetes or hypertension. An X-ray taken 5 months after radiotherapy revealed a radiopaque area (Figure 3).
Case 4:
A 61-year-old woman, weighing 65 kg and 157 cm tall, with a history of breast cancer, was referred. She has no history of hyperlipidemia or diabetes. After 7 sessions of radiotherapy, an X-ray was prepared (Figure 4).
3. Discussion
Atherosclerosis is one of the most common vascular diseases worldwide, affecting many individuals in older age. The most well-known complications of this disease include an increased risk of cardiovascular disorders, while less common but significant complications such as stroke and infarction also warrant attention.
Recent research has indicated that radiotherapy is associated with the formation of a stroke-stimulating factor known as atheroma in the cervical region of the carotid artery, which can be detected on panoramic radiographs (10).
Currently, head and neck cancers are treated with surgery, chemotherapy, and radiotherapy. The complications of radiotherapy are dose-dependent and significantly influenced by the radiation field.
One notable complication of radiotherapy is atherosclerosis in vessels such as the carotid artery, particularly when the radiation field includes regions affected by lymphoma, breast cancer, and other mediastinal cancers. Radiation doses of 45 Gy and higher are associated with this complication. The dose of radiation linked to the development of carotid atherosclerosis ranges from 40 Gy for the treatment of Hodgkin's and non-Hodgkin's lymphoma to 50-80 Gy for the treatment of squamous cell carcinoma and salivary malignancies of the head and neck (11).
Some studies, utilizing Doppler ultrasound and angiography (12), have shown that the damage caused by radiotherapy is extensive and typically involves the distal part of the common carotid artery, the bifurcation area of the artery, as well as the proximal and distal parts of the internal carotid artery. In contrast, spontaneous atherosclerosis is usually limited to the bifurcation area of the common carotid artery and the proximal internal carotid artery (12, 13).
In a study, the carotid arteries of 40 patients were examined 10 years post-radiotherapy, and 40% showed stenosis in their arteries (14). In a similar study, among 23 patients, 22% had carotid stenosis 4.9 years after completing radiotherapy (13). A recent cohort study indicated that radiotherapy either initiates new atherosclerosis or accelerates existing conditions, underscoring the importance of early diagnosis to prevent the potentially fatal outcomes of carotid atheroma (15).
Another study demonstrated that the prevalence of severe stenosis following radiotherapy in head and neck cancer patients is low. It suggests that common cardiovascular risk factors are more influential in causing these lesions. Consequently, regular and continuous examinations are essential for patients receiving radiotherapy who have underlying cardiovascular risk factors (3, 16). These lesions typically appear 1.5 to 2.5 cm below and posterior to the angle of the mandible (17). Dentists play a crucial role in early diagnosis, as patients are often referred to them before, during, or after radiotherapy for routine dental check-ups. Dentists should also consider the possibility of new or recurring diseases in radiotherapy patients and manage dry mouth while preventing osteoradionecrosis (18).
Identifying patients with carotid atheroma through panoramic radiography is vital, as radiotherapy-related atherosclerosis may be the first sign of acute ischemic stroke (19, 20). Timely diagnosis and follow-up of these lesions can significantly reduce the risk of death.
Therefore, guidelines should be developed for dentists treating patients undergoing head and neck radiotherapy. These guidelines should include educating dentists to screen for critical lesions, such as radiopaque lesions in the paravertebral area suspected of being carotid atheroma, and referring patients to appropriate physicians for further treatment if such lesions are detected. Specialist physicians must evaluate patients for high blood pressure, high cholesterol, high blood sugar, and smoking, as arteries exposed to radiation are particularly sensitive to these atherogenic factors (21). It is also recommended that doctors use ultrasound and other imaging methods to assess the extent of stenosis (22).
3.1. Conclusions
Radiotherapy, a common treatment for head and neck malignancies, can lead to carotid atheroma. Dentists should monitor panoramic views of patients receiving radiotherapy for any suspicious lesions and refer patients with detected atheroma to a cardiovascular specialist for timely treatment, thereby helping to prevent cerebral attacks and sudden death.