1. Background
Diabetes Mellitus (DM) is one of the most prevalent chronic diseases characterized by chronic hyperglycemia (1). Hyperglycemia is associated with deficiencies in insulin secretion, insulin function, or both. Chronic hyperglycemia in diabetes can lead to microvascular and macrovascular diseases that affect various organs (2-4).
Diabetes can lead to impaired swallowing function, which is the result of coordinated muscle contractions in the mouth, pharynx, larynx, and esophagus, making it a complex sensorimotor process (5). Dysphagia, a disruption in the movement of the food bolus, can occur in all phases of swallowing, including oral preparatory, oral voluntary, and pharyngeal phases (6).
Diabetes may contribute to dysphagia in several ways. Dry mouth is a common complaint and may serve as an early sign of diabetes onset. Reduced salivary flow rate and altered composition in individuals with dry mouth can lead to difficulties in speaking, swallowing, and chewing (2, 7). Additionally, metabolic and endocrine diseases can cause salivary dysfunction, potentially resulting in altered taste sensation or heightened detection thresholds (2). In addition to salivary and taste dysfunction, diabetes is associated with decreased tongue-lip motor function. Regardless of the exact mechanisms, some neuromuscular changes in diabetes impair the intricate movements of the tongue and lips, leading to decreased endurance or increased fatigability of orofacial muscles (8).
Swallowing difficulties often stem from disturbances in the motor cortices of the brain and neuronal damage (9). The Vagus nerve plays a critical role in controlling certain tongue muscles, pharyngeal constrictors, and laryngeal muscles (9). Impaired coordination between the inferior constrictor muscle and the cricopharyngeus muscle of the upper esophageal sphincter, along with cricopharyngeal muscle hyperactivity during swallowing, may contribute to oropharyngeal dysphagia in diabetic patients (6). Common signs and symptoms in diabetic patients may include coughing, choking, throat clearing, and a post-swallow wet sensation. These symptoms may arise due to inadequate pharyngeal constriction, insufficient laryngeal excursion, and reduced base of tongue movement, all contributing to swallowing disorders (6, 9). Moreover, diabetes can have adverse effects on patients' lives, potentially leading to reduced self-esteem and impacting their social life, work, and leisure activities (10).
Several studies have documented oropharyngeal dysphagia symptoms in diabetic patients. Additionally, in 2020, Witzke found that diabetic patients reported a range of symptoms. Furthermore, these symptoms were more pronounced in older patients, patients with type 2 diabetes, and patients who had been diagnosed for less than 50% of their lives. Moreover, Zakaria et al. 2017 evaluation of dysphagia among diabetic patients reported that the most common symptom was "I cough when I eat" (9, 11). However, relatively few studies have investigated the presence or absence of dysphagia symptoms in individuals with diabetes, and factors such as the type of treatment and quality of life have not been considered in the mentioned studies (9, 12-14).
On the other hand, the global prevalence of type 2 diabetes is projected to increase to 7079 individuals per 100,000 by 2030 (15). Consequently, due to the rising global prevalence of diabetes and its detrimental consequences, there is a critical need for more accurate information to identify dysphagia among diabetic patients. This will lead to the development of better screening tools and more effective treatments.
2. Objectives
This study aims to investigate the relationship between diabetes and oropharyngeal dysphagia concerning sex, age, diabetes duration, and intervention type. Furthermore, understanding the impact of dysphagia related to diabetes on the quality of life may help streamline later interventions for patients with diabetes.
3. Methods
In this recent cross-sectional study, 268 patients (169 females and 99 males) with diabetes were selected using a convenient sampling method at the diabetic clinic of Pardis Medical Center in Shiraz, Iran. The diabetic clinic at Pardis was one of the few clinics designated for diabetic patients, and the sample collection lasted for 3 months. The group comprised 99 males and 169 females. To enhance the possibility of evaluation and to avoid the impact of aging on swallowing, the subjects were aged between 18 and 65 years (16). All patients were diagnosed with type 2 diabetes, which was defined as having a recorded fasting plasma glucose level of ≥ 126 mg/dL or a recorded hemoglobin A1c level of ≥ 6.5% as one of the inclusion criteria (17). Since the study focused on dysphagia related to diabetes, patients were required to exhibit no signs of any systemic or structural conditions in the past that might have caused any form of dysphagia. Thus, one of the inclusion criteria was the absence of a medical history of thyroid disorders, tumors, previous cardiovascular accidents, head and neck traumatic injuries, neoplasms, radiation in the pharyngeal or esophageal areas, or any prior systemic neurological disorders (6). Additionally, the research plan was reviewed and approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1400.247).
3.1. Data Collection
Demographic and disease characteristics, including age, sex, educational status, diabetes type, treatment method (insulin injection or oral medication), any signs of dysphagia, and duration of diabetes, were recorded based on patient self-reports. The relationship between these factors and the scores of the two tests used in the study was analyzed (please refer to Appendix 1). The impact of dysphagia on the quality of life of diabetic patients was measured using the Persian version of the Dysphagia Handicap Index (P-DHI). This patient-administered questionnaire consists of 25 items divided into three subscales: 9 questions in the physical subscale, 9 questions in the functional subscale, and 7 questions in the emotional subscale. The total P-DHI score ranges from 0 to 100 and is calculated based on patients' responses to each question, which are rated as "never," "sometimes," or "always." The patient's response is assigned a value of 0, 2, or 4, respectively (18).
3.2. Procedure
Upon arrival at the Pardis diabetic clinic, patients were provided with an explanation of the research objectives and the procedures for the tests. Consent was then obtained from all participating patients. Subsequently, the inclusion criteria were checked, brief medical histories were collected, and demographic information was recorded. The Mann Assessment of Swallowing Ability (MASA) test was the first assessment administered, followed by the completion of the P-DHI questionnaire by the patients. The entire process was explained to the patients in consultation with the clinic supervisor.
3.3. Data Analysis
The data were analyzed using SPSS version 16. Descriptive statistics were reported, including means with 95% confidence intervals, standard deviations, frequencies, and percentages. To test the differences in specific variables among multiple groups, ANOVA was employed, and for evaluating correlations between variables based on their type, both Pearson and Spearman correlation coefficients were utilized.
3.4. Scoring of MASA and P-DHI
A comprehensive assessment of oropharyngeal dysphagia was conducted using the MASA. This tool comprises 24 items designed to evaluate various aspects of the subject's condition, including general status (such as alertness, cooperation, auditory comprehension, aphasia, apraxia, and dysarthria); the oral preparation phase (saliva, lip seal, tongue movement, tongue strength, tongue coordination, oral preparation, respiration, and respiratory rate for swallowing); the oral phase (gag reflex, palatal movement, bolus clearance, and oral transit time); and the pharyngeal phase (cough reflex, voluntary cough, voice, tracheostomy, pharyngeal phase, and pharyngeal response). The scoring for each item is based on the severity of impairment, with a maximum score of 5 or 10 points. The total MASA score ranges from 38 to 200, and dysphagia is diagnosed when the total score is ≤ 177. Higher scores indicate better oropharyngeal function (19, 20).
4. Results
The mean age of the 268 patients with type 2 diabetes mellitus was 57.49 (SD: 7.661). The mean duration of diabetes mellitus was 11.29 (8.215) years. Personal and medical data for the patients with diabetes are presented in Table 1. In this table, the duration of diabetes among participants is reported in two groups. This differentiation was made because most research has indicated that the effects of diabetes on the body are more likely to manifest after developing this disorder over a period of 5 years (21, 22).
| Variables | No. (%) | Mean ± SD | Range (min - max) |
|---|---|---|---|
| Sex | |||
| Female | 169 (63.1) | - | - |
| Male | 99 (36.9) | - | - |
| Mode of treatment | |||
| Insulin injection | 74 (27.6) | - | - |
| Without insulin injection | 194 (79.4) | - | - |
| Education | |||
| lower than diploma | 166 (61.9) | - | - |
| Diploma | 62 (23.1) | - | - |
| higher than diploma | 40 (14.9) | - | - |
| Age | 57.49 ± 7 .661 | (31-65) | |
| < 50 | 51 (19) | ||
| ≥ 50 | 217 (81) | ||
| Duration of diabetes (23) | 11.29 ± 8.215 | (1-47) | |
| < 5 | 51 (19) | ||
| ≥ 5 | 217 (81) |
The mean score of P-DHI was 4.73, with the highest score being 38 and the lowest reported as 0. Additionally, the mean score of MASA was 194.79 (± 5.093). According to the cutoff value, only one participant had a score below 178. This particular patient had been living with diabetes for over 10 years and was undergoing treatment with oral medication. During the assessment with the MASA test, she exhibited dysfunction of the palate, insufficient lip seal, low tongue strength, poor voluntary cough, and voice issues. It's worth noting that the MASA test was originally designed for neurogenic patients (20). However, not all neurogenic patients were selected to diagnose dysphagia in diabetic patients. Despite the MASA test's limitations in detecting many diabetic patients with dysphagia, conducting a comprehensive evaluation of all oropharyngeal stages of swallowing with MASA allowed for an examination of the relationship between age, sex, diabetes duration, treatment method, and the severity of dysphagia, as presented in Table 2.
| Variables | MASA | P-Value | P-DHI | P-Value |
|---|---|---|---|---|
| Sex | 0.008 | 0.065 | ||
| Male | 195.86 ± 4.729 | 3.29 ± 5.118 | ||
| Female | 194.16 ± 5.207 | 5.21 ± 5.699 | ||
| Modes of treatment | 0.071 | 0.001 | ||
| Insulin injection | 193.88 ± 5.216 | 6.59 ± 6.020 | ||
| Without insulin injection | 195.13 ± 5.016 | 4.02 ± 5.154 |
a Values are presented as mean ± SD.
Table 2 illustrates that females had lower mean scores for both MASA and P-DHI compared to males. While the difference in MASA scores was statistically significant, the difference in P-DHI scores was not statistically significant. There was no correlation between the mode of treatment and MASA scores. Patients who received insulin injections had a lower quality of life, as indicated by the higher P-DHI scores, while patients who took pills had a higher quality of life.
| Variables | P-Value | Pearson’s rho |
|---|---|---|
| MASA and age | 0.0001 | -0.215 |
| MASA and disease duration | 0.005 | -0.169 |
| P-DHI and age | 0.149 | 0.088 |
| P-DHI and disease duration | 0.092 | 0.103 |
Table 3 displays the results of Pearson correlation analysis, examining the relationship between MASA scores and age and disease duration, as well as P-DHI scores and age and disease duration. MASA scores were found to be correlated with both age and disease duration. However, P-DHI scores did not show a significant correlation with age or disease duration. Furthermore, the negative Pearson's coefficient indicates that higher MASA scores were associated with younger age and shorter disease duration.
| Variable | Mean ± SD | P-Value |
|---|---|---|
| Education Level | ||
| Lower than diploma | 5.31 ± 5.095 | 0.069 |
| Diploma | 3.48 ± 5.621 | |
| Higher than diploma | 4.25 ± 6.705 |
Table 4 presents the P-DHI scores for patients with varying levels of education. ANOVA was used to compare P-DHI scores, and no significant difference was observed among participants with different education levels.
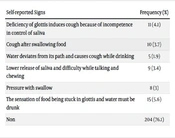
After collecting the medical history of patients, various signs of dysphagia that were not included in the MASA test were recorded. All self-reported signs were documented, and their distribution is presented in Table 5.
| Self-reported Signs | Frequency (%) |
|---|---|
| Deficiency of glottis induces cough because of incompetence in control of saliva | 11 (4.1) |
| Cough after swallowing food | 10 (3.7) |
| Water deviates from its path and causes cough while drinking | 5 (1.9) |
| Lower release of saliva and difficulty while talking and chewing | 9 (3.4) |
| Pressure with swallow | 8 (3) |
| The sensation of food being stuck in glottis and water must be drunk | 15 (5.6) |
| Non | 204 (76.1) |
Table 5 displays the signs of dysphagia reported by the participants. The most frequently reported sign was the "sensation of food being stuck in the glottis." Additionally, the signs of "Deficiency of glottis inducing cough due to incompetence in controlling saliva" and "Coughing after swallowing food" were also reported at a high frequency.
5. Discussion
This study aimed to assess the symptoms of oropharyngeal dysphagia caused by diabetes and examine the relationship of oropharyngeal dysphagia with sex, age, diabetes duration, and intervention type. The results of this study demonstrated that the duration of diabetes and age were correlated with the MASA score. Additionally, the MASA score was higher among women than men. Furthermore, the P-DHI score was higher among people who received insulin injections, and there was also a correlation between the P-DHI score and age. Moreover, by querying patients with diabetes about the signs of dysphagia, several signs, including the "sensation of food being stuck in the glottis," "deficiency of glottis inducing cough due to incompetence in controlling saliva," and "cough after swallowing food," were reported most frequently.
The results of this study revealed a correlation between the duration of diabetes and the MASA score. This finding aligns with Witzke who concluded that patients with a longer duration of diabetes are at a greater risk for swallowing problems, likely due to the increased severity of side effects, including nerve damage, in patients with longer-standing diabetes (9). In contrast, Saleh and Sulieman found no relationship between the duration of diabetes and the presence of dysphagia. However, Saleh and Sulieman used the A-EAT-10 assessment to monitor oropharyngeal dysphagia in 200 patients, which is a tool for short screening and cannot comprehensively evaluate all steps of swallowing (6). In the present study, a comprehensive assessment tool was employed to evaluate all aspects of dysphagia.
Regarding the effect of aging on swallowing, a significant correlation was observed between age and the MASA score. This finding is consistent with the findings of Saleh and Sulieman and Witzke, who reported that older individuals exhibited more symptoms of dysphagia, likely due to age-related changes in the physiology of swallowing (6, 9). Although no correlation was found between the P-DHI score and the duration of diabetes, several items of the P-DHI were accurately indicated by patients with diabetes. These symptoms of dysphagia were also directly described by patients in their medical histories as self-reported signs. This suggests that the duration of diabetes may not directly affect the quality of life, but specific items of the P-DHI should be considered.
Females were found to have higher MASA scores than males, although there was no statistical difference between males and females in P-DHI scores. This outcome may be attributed to the higher prevalence of neurological disorders and neuropathy among women compared to men (24). Thus, the main side effect of diabetes that causes swallowing problems appears to be more common among women. This finding is consistent with Saleh and Sulieman, who found higher scores on the A-EAT-10 for women than men (6).
The choice of treatment mode may influence the severity of dysphagia, as insulin use is often considered an accurate indicator of the severity of diabetes (25, 26). Consequently, more severe diabetes may lead to more pronounced dysphagia and a lower quality of life among individuals with diabetes. Although lower P-DHI scores were observed in insulin users compared to non-insulin users, no significant difference in the severity of dysphagia was found between the two groups of insulin users and non-insulin users.
Apart from the MASA test, which detects signs of dysphagia, patients reported nine signs of dysphagia in their medical history. The most common sign was the "sensation of food being stuck in the glottis, requiring the consumption of water," which may be attributed to delayed pharyngeal emptying. Moreover, this sign was also the most common in the studies conducted by Witzke and the second most common in Saleh and Sulieman's work. The second most frequently reported complaint was the "cough induced by glottal insufficiency due to poor saliva control." This sign was also reported in Witzke's study, albeit with lower frequency. The difference in frequency may be attributed to variations in sample size, as Witzke examined 10 individuals, while the current study involved 268 patients (6, 9).
In summary, the evaluation conducted on a group of 268 individuals with diabetes using MASA and P-DHI tests yielded significant findings related to the presence of nine symptoms suggestive of oropharyngeal dysphagia, such as the "sensation of food being stuck in the glottis," "cough induced by glottal insufficiency due to poor saliva control," "cough after swallowing food," and more. Additionally, insulin injection was identified as a factor leading to a lower quality of life.
The presence of diabetes implies a greater risk of swallowing problems due to the frequent occurrence of autonomic neuropathy as a diabetic complication. This study focused on individuals with type 2 diabetes, and future research could explore individuals with type 1 diabetes. To assess the quality of life and the level of dysphagia, two tests were employed. P-DHI is a self-administered questionnaire used to describe the impact of dysphagia on the lives of diabetic patients. Additionally, a comprehensive test was required to evaluate all stages of swallowing, leading to the selection of the MASA test as one of the most comprehensive options. However, despite the useful features of the MASA test, it was unable to detect all patients with dysphagia. This limitation may arise from the fact that the MASA test was initially designed for stroke patients, although all patients with neurological disorders were excluded from the study.
Lack of an appropriate test specifically designed to evaluate the impact of diabetes on swallowing function was a major challenge in this study. Therefore, it is suggested that a comprehensive test be developed based on the specific signs exhibited by patients with diabetes. Additionally, given that data collection occurred during the COVID-19 pandemic, convenience sampling was employed. Furthermore, the study was conducted in a single city, but ethnicity varies across different cities, potentially affecting diabetes susceptibility. Thus, future studies could investigate dysphagia signs and the prevalence of dysphagia among diabetic patients in different cities. Further research and testing are needed to enhance our understanding of oropharyngeal dysphagia in people with diabetes.
5.1. Conclusions
The results have shown that patients with diabetes may exhibit various symptoms of oropharyngeal dysphagia. Therefore, detecting these diverse signs of dysphagia associated with diabetes can aid researchers in developing a new screening tool for dysphagia in these patients. Additionally, the recent study has uncovered several relationships between variables, providing valuable insights for therapists in predicting certain signs. For example, a significant relationship was observed between the duration of diabetes and the occurrence of dysphagia, which can assist therapists in predicting dysphagia in patients with a long history of diabetes.