1. Background
Being overweight and obese results from the interaction between environmental factors, genetic factors, and human behavior. It is estimated that the leading cause of disability-adjusted life years (DALYs) in Iran in 2019 was attributable to a high Body Mass Index (BMI) (1). Pre-pregnancy weight and gestational weight gain are considered significant perinatal complications. There is a correlation between excessive gestational weight gain and an increased incidence of maternal and neonatal complications, such as hypertensive disorders during pregnancy, fetal macrosomia (2, 3), and an elevated number of cesarean deliveries (4). Obesity is currently one of the most important health threats worldwide, and the incidence of obesity among women of childbearing age is still increasing.
Obesity and overweight in pregnant women have numerous complications, including excessive gestational weight gain, gestational diabetes mellitus, vaginal surgery-assisted delivery, cesarean section, hypertensive disorders, and preeclampsia (5-8). It is estimated that about 24% of any pregnancy complications are attributable to the overweight or obesity of pregnant women (7). Pre-pregnancy obesity can lead to spontaneous abortions and congenital fetal defects in early pregnancy. Additionally, pre-pregnancy obesity increases the risk of metabolic disorders and may impair the infant's neurocognitive development (9, 10).
Researchers have reported a significant increase in stillbirth risk with increasing BMI, particularly during early- and late-term gestation periods (11, 12). Institute of Medicine (IOM) guidelines recommend that the amount of gestational weight gain should be 12.5 - 18 kg for women with a pre-pregnancy BMI categorized as underweight (< 18.5 kg/m2), 11.5-16 kg for normal weight (18.5 - 24.9 kg/m2), 7 - 11.5 kg for overweight (25 - 29.9 kg/m2), and 5-9 kg for obese (≥ 30 kg/m2) (10).
Eating behavior changes are an effective way to control weight gain during pregnancy. Rauh et al. demonstrated the effectiveness of a lifestyle intervention, including weight monitoring, in reducing the proportion of women exceeding weight gain recommendations (13, 14). Interventions targeting psychological mechanisms, such as self-efficacy, have been suggested as a potential solution to this issue (14).
Self-efficacy theory, developed by Bandura and Adams, refers to the belief in one's ability to achieve goals and face challenges. Four strategies to improve self-efficacy include: (1) mastering tasks through step-by-step practice and experience to increase confidence in skills; (2) observing successful others to model their behavior and learn new skills; (3) receiving support and encouragement from close individuals to strengthen self-belief; and (4) training to relax, cultivate a positive mood, and reduce stress. These strategies can help strengthen self-efficacy and enhance performance in various areas of life (15). Self-efficacy, as a cognitive determinant, not only influences an individual's motivation but also their success in performance, particularly when evaluating quality of life tools (16, 17). Educational interventions that improve self-efficacy and behavior control have been associated with improvements in weight control programs (18). Research has consistently shown that self-efficacy plays a significant role in influencing healthy behaviors, including physical activity, healthy food consumption, and stress control. However, its specific impact on weight control among obese and overweight pregnant women has not been established. Studies have found that self-efficacy beliefs are strongly associated with weight control behaviors and can predict weight change during active treatment (19). In pregnant women, perceived benefits and barriers are significant predictors of weight control self-efficacy (20). Higher self-efficacy scores are associated with greater weight loss in overweight/obese postmenopausal women (21). Additionally, improvements in self-regulatory efficacy and physical self-concept are related to improvements in body satisfaction in obese women initiating exercise with cognitive-behavioral support (22). These findings suggest that self-efficacy is a key factor in weight control, and it is necessary to explore its role in obese and overweight pregnant women.
Although Iran's Ministry of Health has developed guidelines for weight gain according to pre-pregnancy BMI, there is no individualized behavioral guidance for weight control in pregnant women, especially those with pre-pregnancy obesity (23).
2. Objectives
This study aims to show the effect of improving self-efficacy in controlling excessive weight gain in pregnant obese and overweight women.
3. Methods
3.1. Procedure and Participants
This study was conducted as a quasi-experimental pretest-posttest design. The study population consisted of overweight and obese pregnant women attending healthcare centers in Dezful city, Iran, during the second and third trimesters of pregnancy. Pregnant women were selected using a convenience sampling method based on their medical records to receive psychological training in self-efficacy as a one-month intervention.
The inclusion criteria for the study were: (a) pregnant women whose medical records were registered in healthcare centers before pregnancy; (b) women who were in the second and third trimesters of pregnancy; and (c) women who had a pre-pregnancy BMI equal to or higher than 25 (25 - 29.9 as overweight and BMI equal to or higher than 30 as obese).
The exclusion criteria included: (a) pregnancies with twins or more; and (b) high-risk pregnancies. The safety of the intervention was approved using the guidelines of the Office of Community Nutrition Improvement of the Ministry of Health and Medical Education for weighing pregnant women. We embedded self-efficacy strategies into these materials (24). The intervention was designed and supervised by two authors, a gynecologist and a Ph.D. in Health Education and Health Promotion. An instructor with an MS in Health Education and Health Promotion implemented the intervention.
The consent form in the subjects' consent in the method section provides participants with information about the study and seeks their agreement to participate. We obtained informed consent by providing patients with detailed information about the procedures and interventions.
3.2. Sample Size
The sample size was calculated using the G* Power software package (version 3.1.9.2, Heinrich Heine University, Dusseldorf, Germany). To achieve a statistical power of at least 80% (25) for examining a medium effect size (Cohen's d = 0.6), with an α error set at 0.05 and accounting for a 20% dropout rate, we required at least 55 individuals per group. However, we selected 160 pregnant women and randomly assigned them to either the intervention or control group using random allocation software (https://random-allocation-software.software.informer.com/2.0/). This study used a per-protocol approach to deal with data loss caused by participants dropping out of the study. This type of analysis excludes participants who did not follow the protocol as intended.
Twenty participants did not receive any interventions: 12 women experienced issues with vomiting, 7 women contracted COVID-19, and one participant had to withdraw due to relocation from Dezful. As a result, the sample size was reduced to 140 participants from the initial 160. Among these participants, 69 were randomly allocated to the intervention group, and 71 were assigned to the control group.
3.3. Measurements
The demographic information, including age, gestational age, BMI, and level of education, was obtained from all pregnant women.
The Weight Efficacy Lifestyle Questionnaire: The Weight Efficacy Lifestyle Questionnaire (WEL) was developed to directly measure an individual's confidence in their ability to manage their body weight, even in the face of potential obstacles (26). The questionnaire stem is “I am confident I can manage my body weight even if/when…”. There are 20 items in the questionnaire that need to be rated on a Likert Scale of 0 to 4, with 0 representing no confidence and 4 representing high confidence. The maximum score that can be achieved is 80, while the minimum is 0. A higher score indicates better self-efficacy.
The initial analysis of the WEL revealed that self-efficacy could be best characterized by five factors related to different circumstances. These factors include negative emotions (five questions) such as “I can resist eating when I am anxious (nervous)”; availability (five questions) such as “I can resist eating even when there are different kinds of food available”; social pressure (four questions) such as “I can resist eating when I have to say ‘no’ to others”; physical discomfort (three questions) such as “I can resist eating when I am in pain”; and positive activities (three questions) such as “I can resist eating when I am watching TV”. Studies have also shown notable enhancements in WEL scores in relation to obesity treatments (14, 27).
The validity and reliability of the Persian version of the WEL were assessed and confirmed in a study conducted by Navidian with a Cronbach's alpha coefficient of 0.88 (28).
We also utilized calibrated digital scales to ensure accurate and consistent weighing of pregnant women.
3.4. Intervention
In this study, the guidelines from the Office of Community Nutrition Improvement of the Ministry of Health and Medical Education for weighing pregnant women were utilized. Following the random allocation of pregnant women into control and intervention groups, a self-efficacy questionnaire was administered to both groups. Subsequently, pre-test demographic and experimental data were collected. All interventions were tailored based on gestational weeks and weight categories for overweight and obese individuals, following the guidelines outlined in the Ministry of Health of Iran's booklet. Interventions included six sessions, each lasting 60 - 90 minutes, over one month. Small groups of five participants were formed, and the first author conducted each group to facilitate the intervention.
The weight management interventions, which incorporated self-efficacy strategies, comprised the following: (1) implementation of step-by-step weight control behaviors to gain mastery experiences; (2) learning from individuals who achieved success in weight control as vicarious experiences; (3) employing encouragement and positive verbal reinforcement as verbal persuasion; and (4) instructing relaxation techniques to foster a positive mood and reduce stress, achieving physiological arousal. Weight control was assessed in each session. Table 1 shows the material and methods used in each session during the intervention.
| Session | Purpose | Materials | Method |
|---|---|---|---|
| 1 | Learning step-by-step implementation of weight control behaviors | Diet (avoiding fried foods, cooking in boiled form, and reducing fats like butter and cream.) | Virtual |
| 2 | Applying vicarious experiences and role modeling | Diet reducing intake of sweets and starchy foods (e.g., bread, cereals) | Virtual |
| 3 | Verbal persuasion and encouraging women following compliance with recommendations | Physical activity types recommendation for obese and overweight pregnant women | Face-to-face /virtual |
| 4 | Weight control and training the weighting | All life style training incorporated to mindfulness therapy | Virtual |
| 5 | Relaxation and stress management | Physical activity types | Face-to-face/virtual |
| 6 | Monitoring and providing feedback | Diet and Physical activity types/diet | Virtual |
In the step-by-step implementation of weight control behaviors, pregnant women played an active role in setting smaller goals to accomplish larger ones, thereby fostering a stronger sense of self-efficacy upon successful completion. Women were encouraged to share and celebrate their successes, regardless of magnitude, during subsequent sessions. Recommendations were provided for pregnant women at this stage, such as limiting fat consumption by avoiding fried foods, cooking in boiled form, and reducing fats like butter and cream. Additionally, reducing the intake of sweets and starchy foods (e.g., bread, cereals) while promoting the consumption of fiber-rich foods such as fruits and vegetables was advised. Women were also encouraged to engage in low-intensity physical activity three times a week for 10 minutes. During the vicarious experiences stage, pregnant women who maintained appropriate weight and adhered to the recommendations were requested to share their progress with others. This stage facilitated the selection of a successful role model to guide women in improving their weight control behaviors.
Women shared their experiences and communicated the actions taken to replace previous detrimental behaviors, such as avoiding fatty foods and consuming low-fat alternatives. To further enhance eating self-efficacy, pregnant women received encouraging text messages following compliance with recommendations and successful weight control. They also received a gift in face-to-face sessions for obtaining the optimal weight gain. The stage of physiological arousal/excitement centered on individuals' assessment of their physical and mental states resulting from certain behaviors. This assessment influenced individuals' beliefs in their capabilities and abilities to perform certain healthy diet and behaviors. It was observed that many individuals encountered experiences such as stress and anxiety during this stage. A brief mindfulness program was used in a WhatsApp group, and pregnant women were asked to use this program to understand situations where they experience negative or positive emotions, which lead to increased consumption of unhealthy food. The mechanism of the mindfulness program for perceiving negative or positive emotions typically involves increasing self-awareness, attention, and non-judgmental observation of one's thoughts, feelings, and bodily sensations in the present moment. Through mindfulness practices such as meditation, breathing exercises, and body scans, individuals learn to cultivate moment-to-moment awareness of their experiences. Relaxation training materials were developed and shared with pregnant women.
Upon completion of the training period, the self-efficacy questionnaire and data related to women's BMI were collected both before and after the intervention. The control group received standard prenatal care, which included nutritional recommendations.
3.5. Statistical Analysis
The results were summarized using descriptive statistics. Means, standard deviations, and frequencies (percentages) were used to report continuous and qualitative variables. The Shapiro-Wilk test was used to assess the normal distribution of the study variables. Demographic variables and BMI were compared between the two groups using the chi-square test for categorical variables and the independent t-test for normally distributed continuous variables. Independent t-tests were used to compare the control and intervention groups, while paired t-tests were used for within-group comparisons.
The participants of this study were categorized into two groups: Overweight and obese. Weight gain during the intervention was compared for each category between the intervention and control groups. All statistically significant levels were set at α = 0.05. The primary outcome was considered to be the weight gain each week, and the secondary outcome was specified as self-efficacy dimensions, including availability, social pressure, negative emotion, positive emotion, physical discomfort, as well as the total self-efficacy score among pregnant women.
4. Results
A total of 141 pregnant women participated in this study. The average participant age was 29.7 years with a standard deviation of 5.9. In the intervention group, the mean age was 30.49 with a standard deviation of 5.3, and in the control group, it was 29.03 with a standard deviation of 6.4. Of the participants, 48.94% were aged 28 - 38, 46.10% were aged 18 - 28, 4.26% were aged 38 - 48, and 0.71% were aged 48 - 58. The mean and standard deviation of the women's gestational age were 19.96 ± 4.31 weeks in the intervention group compared to 18.98 ± 4.43 weeks in the control group, with 90% of pregnant women participating during the 13th to 26th week of pregnancy. Among all participants, 44.90% had a diploma/sub-diploma, 14.29% had a postgraduate degree, and 40.82% had a bachelor's degree or higher (P-value = 0.061). In a self-report survey, 66.33% of the participants exhibited a moderate socio-economic status, while one-third displayed a favorable socio-economic status. At baseline, no statistically significant differences were found between the intervention and control groups in sub-scales of the self-efficacy questionnaire (P-values > 0.05) (Table 2).
| Variables | Intervention | Control | P-Value b |
|---|---|---|---|
| Age | 30.67 ± 5.34 | 29.18 ± 6.30 | 0.12 |
| Gestational age (week) | 19.96 ± 4.31 | 18.98 ± 4.43 | 0.17 |
| BMI | 29.54 ± 3.40 | 30.68 ± 19.54 | 0.62 |
| Educational level | |||
| Primary school and diploma | 31 | 29 | 0.13 |
| Associate degree | 12 | 10 | 0.14 |
| Bachelor's degree | 20 | 26 | 0.26 |
| Master of degree | 6 | 4 | 0.09 |
| Ph.D. | 0 | 2 | 0.18 |
| Eating self-efficacy dimensions | |||
| Availability | 11.04 ± 3.58 | 11.96 ± 3.52 | 0.21 |
| Social pressure | 9.62 ± 3.51 | 9.46 ± 3.30 | 0.76 |
| Negative emotion | 15.95 ± 3.75 | 16.78 ± 3.17 | 0.14 |
| Positive emotion | 7.64 ± 2.47 | 8.58 ± 2.05 | 0.15 |
| Physical discomfort | 10.12 ± 1.91 | 10.18 ± 1.95 | 0.83 |
| Total self-efficacy score | 54.43 ± 11.28 | 56.37 ± 10.13 | 0.09 |
Abbreviation: BMI, Body Mass Index.
a Values are expressed as mean ± SD or No. (%).
bT-test for quantitative variables; chi-Square test for qualitative categories.
4.1. Primary Outcome
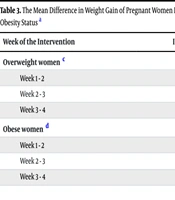
After categorizing participants into overweight and obese groups, the recommended weight gain after week 13 is 0.3 kg per week for overweight participants and 0.2 kg per week for obese participants. Although there was no significant difference in the mean weight gain between the two groups (P > 0.05), participants in the obese group had a higher weight gain than the recommended range during the weeks of intervention (Table 3). Among obese women in the intervention group, the weight gain ranged from 0.16 to 0.30 kg per week, which is within the recommended range. In contrast, the control group had a weight gain range of 0.29 to 0.41 kg per week, which exceeded the recommended range of 0.3 kg per week. The weight gain differences between the control and intervention groups were significant during the one-month intervention (P < 0.05) (Table 3).
| Week of the Intervention | Intervention (kg/w); (n = 69) | Control (kg/w); (n = 71) | P-Value b |
|---|---|---|---|
| Overweight women c | |||
| Week 1 - 2 | 0.18 ± 0.11 | 0.71 ± 0.7.5 | 0.42 |
| Week 2 - 3 | 0.17 ± 0.12 | 1.31 ± 7.40 | 0.26 |
| Week 3 - 4 | 0.23 ± 0.17 | 0.31 ± 0.39 | 0.19 |
| Obese women d | |||
| Week 1 - 2 | 0.16 ± 0.1 | 0.41 ± 0.4 | 0.02 |
| Week 2 - 3 | 0.3 ± 0.3 | 0.29 ± .23 | 0.96 |
| Week 3 - 4 | 0.25 ± 0.12 | 0.51 ± 0.5 | 0.01 |
a Values are expressed as mean ± SD.
b Independent sample t-test.
c Recommended weight gain is 0.3 kg/w for overweight women.
d Recommended weight gain is 0.2 kg/w for obese women.
4.2. Secondary Outcome
According to the results obtained from Table 4, the mean score of the "Availability" self-efficacy sub-scale before the intervention was 11.04 ± 3.58 in the intervention group and 13.83 ± 2.46 in the control group. However, after the intervention, the mean score of the "Availability" self-efficacy sub-scale was 11.96 ± 3.52 in the intervention group and 12.32 ± 3.23 in the control group. This indicates an improvement in the "Availability" sub-scale in the intervention group (P < 0.001). Before the intervention, the mean score of the "Social Pressure" sub-scale showed no statistically significant difference between the intervention and control groups (P = 0.76). After the intervention, the mean score in the intervention group (11.22 ± 2.63) was higher than in the control group (9.44 ± 3.13), suggesting an improvement in the "Social Pressure" sub-scale in the intervention group (P < 0.001) (Table 4).
| Self-Efficacy; Dimensions | Before Intervention | After Intervention | P-Value b | Values |
|---|---|---|---|---|
| Availability | ||||
| Intervention | 11.04 ± 3.58 | 13.83 ± 2.64 | < 0.001 | 2.82 ± 2.23 |
| Control | 11.96 ± 3.52 | 12.32 ± 3.23 | 0.885 | -0.03 ± 1.61 |
| P-value c | 0.021 | < 0.001 | < 0.001 | |
| Socialpressure | ||||
| Intervention | 9.63 ± 3.51 | 11.22 ± 2.63 | < 0.001 | 1.62 ± 2.03 |
| Control | 9.46 ± 3.30 | 9.44 ± 3.13 | 0.811 | -0.04 ± 1.47 |
| P-value c | 0.76 | < 0.001 | < 0.001 | |
| Negativeemotion | ||||
| Intervention | 15.95 ± 3.75 | 17.49 ± 2.30 | < 0.001 | 1.55 ± 2.25 |
| Control | 16.78 ± 3.17 | 16.90 ± 2.57 | 0.432 | 0.15 ± 1.63 |
| P-value c | 0.14 | 0.15 | < 0.001 | |
| Positiveemotion | ||||
| Intervention | 7.64 ± 2.47 | 8.97 ± 1.74 | < 0.001 | 1.27 ± 1.49 |
| Control | 8.58 ± 2.05 | 8.38 ± 1.87 | 0.075 | -0.19 ± 0.91 |
| P-Value c | 0.15 | 0.04 | < 0.001 | |
| Physicaldiscomfort | ||||
| Intervention | 10.12 ± 1.91 | 11.03 ± 1.12 | < 0.001 | 0.89 ± 1.48 |
| Control | 10.18 ± 1.95 | 10.33 ± 1.68 | 0.810 | 0.16 ± 1.12 |
| P-value c | 0.83 | 0.004 | 0.001 | |
| Self-efficacytotal score | ||||
| Intervention | 54.43 ± 11.28 | 62.54 ± 7.49 | < 0.001 | 8.13 ± 5.18 |
| Control | 56.37 ± 10.13 | 57.37 ± 8.93 | 0.905 | 0.06 ± 3.93 |
| P-Value c | 0.09 | < 0.001 | 0.001 |
a Values are expressed as mean ± SD.
b Paired t-test.
c Independent sample t-test.
The sub-scale for "Negative Emotion" did not display a significant difference in mean scores after the intervention (P = 0.15). However, the independent sample t-test results revealed a significant difference between the mean differences before and after the intervention for the two groups (1.55 ± 2.25 vs. 0.15 ± 1.63) (P < 0.001) (Table 4). The intervention led to an increase in the "Positive Emotion" sub-scale items related to eating self-efficacy, resulting in a significant difference between the two groups after the intervention (P = 0.04). The mean differences for the intervention group were 1.27 ± 1.49 compared to -0.19 ± 0.91 for the control group (P < 0.001) (Table 4). This pattern also applied to the "Physical Discomfort" sub-scale, with a statistically significant difference between the mean scores before and after the intervention in the two groups (P = 0.001).
The total score of self-efficacy of pregnant women increased by 8 points after the implementation of the intervention, whereas in the control group, there was only a 0.06-point increase (P < 0.001) (Table 4).
5. Discussion
This study aimed to investigate the impact of psychological training based on self-efficacy theory on weight control in obese and overweight pregnant women. The intervention group showed significant improvement in weight gain control compared to the control group. The self-efficacy of women in the intervention group increased from 54.43 ± 11.28 to 62.54 ± 7.49. Additionally, pregnant women in the intervention group successfully controlled their weight gain within the recommended range, while the control group did not meet the recommended guidelines for weight gain. Overall, the study highlights the importance of self-efficacy and behavioral interventions in managing weight gain during pregnancy and suggests the potential benefits of mindfulness-based eating awareness training for pregnant women.
Studies have shown that using self-efficacy theory can promote the empowerment of pregnant women and improve their performance in self-care behaviors during pregnancy (29). Weight maintenance is associated with internal motivation for weight loss, social support, effective coping strategies, resilience in handling life stress, self-belief in one's abilities, autonomy, taking responsibility in life, and overall psychological resilience and stability (30). Pregnant women were asked to follow the diet instructions step by step and note the challenges of consuming healthy foods. In this way, they benefited from the Mastery Experience strategy. Bandura and Adams identified mastery experiences as the most powerful driver of self-efficacy. Mastery experiences benefit self-efficacy by providing direct, personal experience and linking effort to successful performance, enhancing expectancy judgments (15).
Wrieden and Symon and Ferrari et al. both highlight the difficulties in achieving dietary compliance, with the latter emphasizing the need for clear and individualized guidance (31, 32). Studies have reported that the implementation of self-efficacy strategies, along with a theory-based multi-component intervention, significantly improved diet quality and physical activity, ultimately contributing to enhanced weight management (33).
This study aimed to investigate the impact of psychological training based on self-efficacy theory on weight control in obese and overweight pregnant women. The intervention group showed significant improvement in weight gain control compared to the control group. The self-efficacy of women in the intervention group increased from 54.43 ± 11.28 to 62.54 ± 7.49. Additionally, pregnant women in the intervention group successfully controlled their weight gain within the recommended range, while the control group did not meet the recommended guidelines for weight gain. Overall, the study highlights the importance of self-efficacy and behavioral interventions in managing weight gain during pregnancy and suggests the potential benefits of mindfulness-based eating awareness training for pregnant women.
Studies have shown that using self-efficacy theory can promote the empowerment of pregnant women and improve their performance in self-care behaviors during pregnancy (29). Weight maintenance is associated with internal motivation for weight loss, social support, effective coping strategies, resilience in handling life stress, self-belief in one's abilities, autonomy, taking responsibility in life, and overall psychological resilience and stability (30). Pregnant women were asked to follow the diet instructions step by step and note the challenges of consuming healthy foods. In this way, they benefited from the Mastery Experience strategy. Bandura and Adams identified mastery experiences as the most powerful driver of self-efficacy. Mastery experiences benefit self-efficacy by providing direct, personal experience and linking effort to successful performance, enhancing expectancy judgments(15) . Wrieden and Symon and Ferrari et al. both highlight the difficulties in achieving dietary compliance, with the latter emphasizing the need for clear and individualized guidance (31, 32). Studies have reported that the implementation of self-efficacy strategies, along with a theory-based multi-component intervention, significantly improved diet quality and physical activity, ultimately contributing to enhanced weight management (33).
In the current study, self-efficacy improved in the sub-scale of availability, indicating that interventions related to relaxation and physiological arousal in pregnant women reduced the stress and tension associated with adopting healthy eating behaviors. Pregnant women were able to limit their consumption of unhealthy food even when it was available to them in order to control their weight gain. Research consistently shows that relaxation interventions, such as mindfulness, emotional brain training, and relaxation therapy, can significantly reduce stress and improve eating behaviors in pregnant women (34, 35). However, some argue that physiological arousal is considered to be the least influential factor in determining quality of life, as it is typically only indirectly related to our capacity to perform (36).
In this study, the utilization of role models and vicarious experiences, along with the presentation of examples of individuals who have effectively managed excessive weight gain during pregnancy, resulted in a notable improvement in the sub-scale of eating self-efficacy. Bandura and Adams suggested that by observing others succeed or fail at activities, we can gauge our own chances of success or failure in similar activities based on the perceived similarity or difference between ourselves and the person we are observig (15). In our study, individuals concluded through analysis and discussion in virtual spaces that they can refrain from consuming unhealthy food like their successful role models.
The use of role models and vicarious experiences, along with examples of effective weight management during pregnancy, has been shown to improve eating self-efficacy and other healthy behaviors (37, 38). This is consistent with the findings of Terry, who emphasized the role of self-efficacy in promoting gestational weight management (39).
Providing verbal persuasion to pregnant women who have managed their weight gain according to recommended guidelines resulted in an increase in their self-efficacy in eating. Vining highlighted the role of personalized nutritional counseling in helping women achieve recommended weight gain (40). Additionally, delivering mindfulness training aimed at helping individuals understand positive and negative emotional situations they may encounter and control those situations through compensatory eating led individuals towards better insight into eating in positive and negative emotional situations and provided good social support (41). Pregnant women likely engaged in mindfulness practices to develop an understanding of their emotions related to consuming unhealthy food.
By mindfully attending to their thoughts, cravings, physical sensations, and emotional states, they could have gained insight into how these factors contributed to their eating behavior and made more conscious choices. Studies suggest that pregnant women can benefit from mindfulness practices in understanding their emotions related to unhealthy food consumption (42). Mindfulness interventions have been found to reduce stress and overeating during pregnancy (38). This program offers guidance, techniques, and exercises that specifically help pregnant women apply mindfulness to food and make healthier decisions. Studies have shown that mindfulness-based eating awareness training was effective in impacting biological, psychological, and behavioral indicators among overweight and obese women (43).
5.1. Limitation
This study had some limitations, including: (a) the digital literacy and access to technology among pregnant women may vary, potentially limiting the reach and effectiveness of the virtual WhatsApp-based program; (b) sustaining participant engagement over time in a virtual program may be challenging, leading to decreased adherence and potential bias in the results; (c) a short follow-up period may not capture the long-term effects of the intervention on weight gain during pregnancy, potentially underestimating its impact; (d) pregnant women who volunteer for a virtual intervention may differ systematically from those who do not, introducing bias into the study results.