1. Background
Forward head posture (FHP) is the most commonly recognized type of poor head posture in the sagittal plane, involving the forward excursion of the head in relation to the trunk and the plumb line (1-3). Given today's lifestyles, with the increasing use of mobile phones, computers, and technology gadgets, the prevalence of this condition is on the rise (4-6). It is more prevalent among women compared with men (7-9). In general, the prevalence of this disorder is reported to be 63 - 66% (10-13).
Since FHP leads to the forward excursion of the center of gravity, it can affect a person's balance while standing. Additionally, the presence of an impairment in proprioceptive afferents in these individuals can lead to a change in their understanding of the limits of stability (LOS) (14). The LOS is defined as the amount of movement of the center of gravity within the base of the support surface that a person can achieve only by transferring body weight without taking a step (any change in the support surface) (15). In other words, the LOS determines the maximum excursion of the center of gravity that a person can achieve in any direction without losing balance. Individuals with reduced LOS are at an increased risk for falls and injury when shifting their body weight forward, backward, or from side to side (16).
In past studies, several laboratory tools such as the force plate and the Biodex Balance System have been used to evaluate balance in people with FHP (2, 5, 17, 18). Most of these studies have reported reduced balance in people with FHP compared to otherwise normal individuals (2, 5, 18). However, there is an essential need for a reliable and accurate tool to best diagnose and classify balance impairments in these individuals. Presently, computerized dynamic posturography (CDP) represents the gold standard for the assessment of balance and postural control (19). Also, given the moderate to high test-retest reliability (intraclass correlation coefficient = 0.690 to 0.96) for the LOS measures extracted from CDP (20, 21), it appears that the CDP provides more assessment information about LOS than other tools assessing LOS.
Computerized dynamic posturography objectively quantifies people's ability to control posture by measuring the amount of excursion of their center of gravity within the LOS (4, 22, 23). The LOS test using computerized posturography is a precise method to evaluate dynamic postural control during voluntary trunk movement (weight transfer) in different directions (21). Therefore, the results can provide valuable insights into the function of the postural control system in individuals with mild and moderate-to-severe degrees of FHP.
Today's lifestyles have significantly contributed to the increase in the prevalence of FHP, which can negatively affect an individual's balance. Understanding the differences in balance impairment between two groups, mild and moderate-to-severe FHP, can help identify individuals at risk of developing balance impairments and prevent these impairments by focusing on early and appropriate treatment. In this way, individuals with moderate-to-severe FHP could receive appropriate treatment, and those with mild FHP could be prevented from developing balance disorders.
2. Objectives
Although previous studies have revealed that there is reduced LOS in individuals with FHP compared to the control group (2, 5, 18), no study has evaluated LOS between individuals with mild and moderate-to-severe grades of FHP. Therefore, this study aimed to evaluate the changes in the LOS in individuals with mild FHP compared to those with moderate-to-severe FHP.
3. Methods
3.1. Sample Size Estimation
The sample size for this study was calculated using G Power software, considering a Type I error (α = 0.05), a Type II error (β = 0.20), a power of the test = 80%, and a confidence interval = 95% to detect a group difference.
3.2. Participants
This study utilized a cross-sectional observational research design. The participants were 70 individuals with FHP disorder, aged between 17 - 45. They were selected from physiotherapy centers in Ahvaz city and from among the employees and students of Ahvaz University of Medical Sciences who had FHP (IR.AJUMS.REC.1400.707). These individuals were divided into mild and moderate-to-severe groups based on their craniovertebral angle (CVA). The two groups were similar in terms of variables such as age, sex, height, weight, and body mass index. The method and manner of conducting the test were fully explained to the participants, and they were asked to sign an informed consent form approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences. Then they entered the study.
The inclusion criteria for the study were: Age between 17 - 45 years, suffering from FHP, and no history of neck pain or neck injury in the past 6 months. Individuals who had a history of fracture or surgery in the neck area (18, 24), vision problems not corrected with glasses (25), neurological and neuromuscular disorders, inflammatory diseases, rheumatoid arthritis, congenital anomalies (26), moderate and severe scoliosis, severe thoracic kyphosis or breathing problems (1, 17, 24), headache or dizziness, vestibular system disorders (25, 27), lower limb injuries (1, 17), acute, intermittent, or radiating neck pain (25, 27), or drug or alcohol use in the previous 24 hours (27) were excluded from the study.
3.3. Procedure
First, the subjects were asked to stand in a comfortable position with their weight evenly distributed on both feet, looking straight ahead next to a rope hanging from the ceiling and passing in front of their lateral malleolus. Then, based on Kendall's definition, participants who had an ear tragus forward from the shoulder or trunk were diagnosed with FHP (28). In previous studies, the high reliability of Kendall's diagnostic method has been confirmed with a Kappa coefficient of 0.73 (1, 29).
Afterward, to determine the severity of FHP, a camera (Canon G10, Japan) was placed on a tripod at a distance of 1.5 meters from the individual at the same height as their shoulders, and the participants were photographed in a side view (30). Before taking the picture, the tragus points of the ear and the location of the spinous process of the seventh vertebra (C7) were identified and marked using markers. To identify the spinous process of the C7, the participants were asked to flex and extend their heads several times in a full range while standing, and then the spinous process of the C7 was identified (5).
After that, the CVA was measured by calculating the angle between the horizontal line that passes through the C7 and the line that connects the point of the tragus of the ear to the C7, using Kinovea software (Figure 1) (1, 6, 24, 27). A CVA of 45.5 degrees was considered the cut-off point for categorizing mild and moderate-to-severe degrees. People with a CVA less than 45.5 degrees were placed in the moderate-to-severe group, and those with a CVA greater than 45.5 degrees were allocated to the mild group (10). According to Mostafaee et al.’s study, CVA has good accuracy (AUC = 0.88) in discriminating between individuals with mild and moderate-to-severe FHP. Additionally, this angle has a sensitivity of 0.93 and a specificity of 0.62, making it valuable for correctly identifying mild FHP and screening moderate and severe grades of FHP (31).
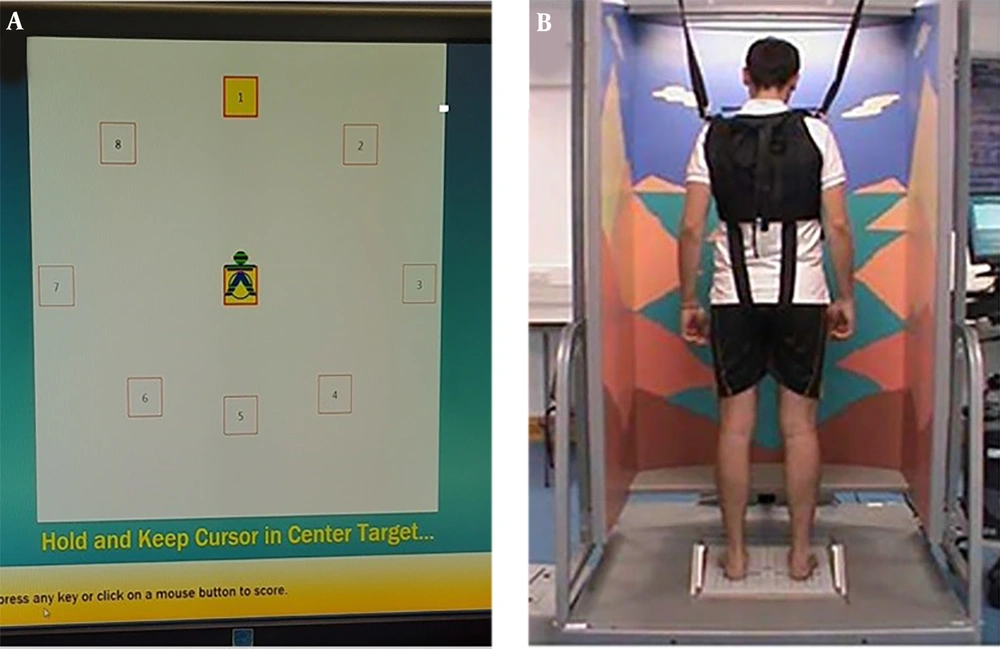
The limits of stability test was performed using a posturography device (NeuroCom, Equitest, USA). The posturography device consists of three main parts: The force plate, the screen, and the main computer body (4). This test evaluated the individuals' ability to voluntarily move their center of gravity and to assess stability in a dynamic state. Subjects were asked to stand on a force plate in front of a screen set at eye level and to voluntarily move their center of gravity toward fixed target points from different directions as far as possible without stepping or losing their balance (20). During this test, the force plate remained constant. On the screen, there was a central square target, with eight other squares in primary and secondary directions (front, back, right, left, front-right, front-left, back-right, back-left). These eight squares represented the person's limits of stability in each direction, determined by the computer at 45° intervals around the center of gravity based on the person's height (21).
Before the main test began, the subject was familiarized with the test and instructed that the position of the human-like character on the screen would move according to their movements and weighting. This character represented the person's center of gravity, which had to be kept in the central square at the beginning of the test. At the start of the test, while keeping their hands at their sides with palms facing the thighs, the participants stood on the specified place on the force plate. After hearing a beep, they moved their weight toward the target with maximum possible speed and accuracy. They maintained the same posture until the target sign disappeared and they heard a second beep, which lasted for 8 seconds. The person's weight transfer during the test focused on the movement of the ankle joint, and they were instructed not to change the position of their legs or bend backward during the test (Figure 2).
Finally, the device averaged the person's performance using EquiTest software in terms of five indicators: Movement reaction time (RCT), movement velocity (MVL), endpoint excursion (EPE), maximum excursion (MXE), and directional control (DCL) in eight directions: Forward (FW), backward (BW), right (RT), left (LT), forward right (FWRT), forward left (FWLT), backward right (BWRT), and backward left (BWLT) (20, 21). The definitions of these variables are given below:
- Reaction time is defined as the time between the movement announcement signal and the start of the person's movement, measured in seconds.
- Movement velocity is the average movement speed of a person in degrees per second, calculated during 5-95% of movement (distance from the starting point). To calculate the speed more accurately, the computer removes the first and last 5% where acceleration is increasing and decreasing.
- Directional control is a comparison of the amount of movement in the desired direction (toward the target) to the amount of movement outside the range (away from the target), expressed as a percentage.
- Endpoint excursion is the distance traveled by the person's center of gravity on the first attempt to transfer weight to the target, expressed as a percentage of the person's limit of stability, indicating the person's tendency to move within their limit of stability.
- Maximum excursion is the farthest distance traveled by the center of gravity in each repetition, expressed as a percentage.
3.4. Statistical Analysis
SPSS version 26 was used for statistical analysis. A confidence interval of 95% and a significance level of P < 0.05 were considered for all analyses. To check for the normal distribution of data, the Kolmogorov-Smirnov (K-S) test was used. The results showed that the distribution of data was normal. Therefore, the t-test was used to determine the statistically significant difference between the two groups of individuals with mild and moderate-to-severe FHP in terms of the average values of age, height, weight, and body mass index. Furthermore, for each LOS variable, we performed a separate 2 × 5 mixed model analysis of variance (ANOVA). The between-group factor was group (mild FHP, moderate-to-severe FHP), and the within-group factors were direction of the LOS (Forward, Backward, Right, Left, and Overall). If there was a significant interaction of group-by-direction of the LOS variables, a comparison between groups was performed using independent-sample t-tests.
4. Results
The results of the present study showed no statistically significant difference between the two groups of people with mild and moderate-to-severe FHP in terms of demographic variables (Table 1). The results of ANOVA showed that the interaction of group by directions of the LOS variables was significant for RCT (F = 11.29, P < 0.001), MVL (F = 9.14, P < 0.001), EPE (F = 11.14, P < 0.001), MXE (F = 10.27, P < 0.001), and DCL (F = 12.95, P < 0.001). A summary of ANOVA results is shown in Table 2. The results of the LOS variables in different directions between the two groups revealed a significant difference between the mild and moderate-to-severe FHP groups in the LOS variables in the forward and backward directions (P < 0.05), while no significant difference between the two groups was observed in the LOS variables in the right, left, and overall directions (P > 0.05). In other words, the group with moderate-to-severe FHP, compared to the group with mild FHP, had longer RCT, lower MVL, shorter distance traveled in the first attempt to reach the target, shorter MXE, and less DCL in both anterior and posterior directions. The results of the LOS variables in different directions between the mild and moderate-to-severe FHP groups are reported in Table 3.
| Demographic Variables | Mild FHP (n = 31) | Moderate-Severe (n = 39) | P-Value |
|---|---|---|---|
| Age (y) | 29.94 (8.18) | 32.38 (9.84) | 0.27 |
| Height (cm) | 170.29 (8.23) | 167.31 (10.38) | 0.24 |
| Weight (kg) | 67.70 (11.06) | 65.35 (12.27) | 0.56 |
| BMI (kg/m2) | 21.31 (3.35) | 24.66 (4.30) | 0.15 |
| Sex | |||
| Female | 13 | 21 | |
| Male | 18 | 18 | 0.81 |
a Values are expressed as mean ± SD.
| Independent Variables | RCT | MVL | EPE | MXE | DCL | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| F-Ratio | P-Value | F-Ratio | P-Value | F-Ratio | P-Value | F-Ratio | P-Value | F-Ratio | P-Value | |
| Main effect of group | 5.36 | 0.02 | 4.83 | 0.03 | 4.97 | 0.02 | 6.07 | 0.01 | 7.54 | 0.00 |
| Main effect of directions of LOS | 19.10 | <0.001 | 11.09 | <0.001 | 18.84 | <0.001 | 26.78 | <0.001 | 30.45 | <0.001 |
| Interaction group × direction of LOS | 11.29 | <0.001 | 9.14 | 0.02 | 11.14 | <0.001 | 10.27 | <0.001 | 12.95 | <0.001 |
Abbreviations: LOS, limit of stability; RCT, reaction time movement; MVL, movement velocity; EPE, endpoint excursion; MXE, maximum excursion; DCL, directional control.
| Variables of LOS | Mild FHP (n = 31) 95% CI | Moderate-Severe FHP (n = 39) 95% CI | P-Value |
|---|---|---|---|
| RCT (s) | |||
| Forward | 0.90 (0.32) (0.78 - 1.03) | 1.09 (0.36) (0.98 - 1.20) | 0.03 |
| Backward | 0.77 (0.28) (0.64 - 0.91) | 1.15 (0.44) (1.03 - 1.27) | 0.00 |
| Right | 0.87 (0.32) (0.77 - 0.97) | 0.90 (0.25) (0.81 - 0.99) | 0.65 |
| Left | 0.80 (0.29) (0.70 - 0.90) | 0.83 (0.26) (0.75 - 0.92) | 0.62 |
| Overall | 0.84 (0.25) (0.76 - 0.92) | 0.86 (0.20) (0.79 - 0.93) | 0.67 |
| MVL (deg/s) | |||
| Forward | 4.21 (1.23) (3.76 - 4.67) | 3.50 (1.20) (3.10 - 3.90) | 0.02 |
| Backward | 3.45 (0.94) (3.12 - 3.79) | 2.98 (0.94) (2.68 - 3.29) | 0.04 |
| Right | 4.54 (2.10) (3.92 - 5.17) | 3.96 (1.37) (3.40 - 4.51) | 0.16 |
| Left | 4.54 (1.90) (4.02 - 5.07) | 4.27 (0.99) (3.80 - 4.74) | 0.44 |
| Overall | 4.16 (1.35) (3.68 - 4.64) | 4.08 (1.34) (3.65 - 4.51) | 0.88 |
| EPE | |||
| Forward | 86.38 (15.21) (80.83 - 91.93) | 78.64 (15.69) (73.69 - 83.58) | 0.04 |
| Backward | 71.93 (12.17) (66.67 - 77.19) | 63.15 (16.38) (58.46 - 67.84) | 0.01 |
| Right | 84.87 (18.03) (77.73 - 92.00) | 77.46 (21.46) (71.10 - 83.82) | 0.12 |
| Left | 87.00 (18.63) (79.87 - 94.12) | 86.30 (20.79) (79.95 - 92.65) | 0.88 |
| Overall | 79.06 (12.97) (74.46 - 83.66) | 76.41 (12.74) (72.30 - 80.51) | 0.39 |
| MXE | |||
| Forward | 98.61 (9.85) (94.39 - 102.83) | 91.89 (13.10) (88.13 - 95.66) | 0.02 |
| Backward | 83.64 (10.56) (78.49 - 88.79) | 76.07 (16.78) (71.48 - 80.67) | 0.03 |
| Right | 96.25 (14.87) (89.97 - 102.54) | 93.41 (19.39) (87.80 - 99.01) | 0.50 |
| Left | 97.06 (14.17) (91.27 - 102.85) | 95.12 (17.56) (89.96 - 100.29) | 0.62 |
| Overall | 91.64 (10.06) (87.69 - 95.59) | 90.02 (11.71) (86.50 - 93.54) | 0.54 |
| DCL | |||
| Forward | 89.51 (3.19) (87.80 - 91.22) | 85.46 (5.71) (83.93 - 86.98) | 0.00 |
| Backward | 79.54 (7.52) (75.71 - 83.37) | 72.46 (12.63) (69.04 - 75.87) | 0.00 |
| Right | 81.80 (7.80) (78.05 - 85.55) | 78.53 (12.16) (75.19 - 81.88) | 0.19 |
| Left | 82.83 (5.17) (80.68 - 84.99) | 81.35 (6.58) (78.44 - 82.27) | 0.09 |
| Overall | 82.77 (5.29) (80.83 - 84.71) | 81.12 (5.48) (79.40 - 82.85) | 0.21 |
Abbreviations: SD, standard deviation; RCT, reaction time movement; MVL, movement velocity; EPE, endpoint excursion; MXE, maximum excursion; DCL, directional control.
a Values are expressed as mean ± SD or No. (%).
5. Discussion
Based on the LOS test, the results of our study showed a significant difference between the two groups of individuals with mild and moderate-to-severe FHP in terms of RCT, MVL, EPE, MXE, and DCL in both anterior and posterior directions. Several reasons could explain this significant difference:
The myofascial network is continuous, and according to Myers' theory, among the 11 paths of myofascial lines, the dorsal superficial line extends from the gastrocnemius to the hamstring tendon, the ischial tuberosity, the sacrotuberous ligament, the thoracolumbar fascia, the erector spinae, the iliocostalis, and the frontal muscles. Therefore, it can transfer tension from the head or gastrocnemius to other connected parts (32-34). Thus, in conditions of structural imbalance, such as the head facing forward, where the center of gravity of the body is shifted from its normal position and moved forward, more muscle activity is needed to achieve balance. As a result, there will be a decrease in a person's ability to respond to external stimuli and properly regulate changes (35). In other words, FHP results in eccentric contraction of the posterior cervical muscles, which influence balance control by delivering tension to the plantarflexion of the ankle through integration with the effect of the fascia (33).
On the other hand, due to the anterior excursion of the center of gravity in individuals with FHP, there is a fear of losing balance and falling while moving forward. Given that in people with moderate-to-severe FHP, the amount of excursion of the center of gravity is greater and that the ankle has a lower level of support on the posterior side due to its biomechanics, the fear of falling and losing balance in these people is more pronounced in anterior and posterior directions. This reduces the movement velocity and increases the reaction time in the moderate-to-severe FHP group (4, 23).
Also, since the superficial back line transmits tension from the back or gastrocnemius to other parts, the anterior shift of the center of gravity in people with FHP, compared to those with normal posture, causes more tension in the extension muscles toward the head, resulting in a reduction of ankle plantarflexion range of motion (4, 23). In general, individuals with FHP have limited movement capacity in the joints of the lower limbs (4, 23). Therefore, considering the negative relationship between the severity of FHP and the ankle’s range of motion (33, 34), it can be concluded that individuals with moderate-to-severe FHP have more movement restrictions in lower limb joints than individuals with mild FHP. For this reason, the distance traveled and the maximum excursion in the first attempt to reach the target point is reduced in individuals with moderate-to-severe FHP compared to those with mild FHP.
Furthermore, our study results did not show a significant difference in these variables of the LOS test in other directions between the two groups of mild and moderate-to-severe FHP. Despite the exaggerated anterior location of the COG with FHP, the absence of body asymmetry on the right and left sides contributes to maintaining the ability to control direction and movement in the other directions (23).
The results of our study are in agreement with those of previous studies (4, 23, 35) that examined the LOS in individuals with FHP. The results of those studies showed that individuals with FHP have decreased balancing ability compared to the normal head posture group (4, 23, 35). Of course, in previous studies, comparisons were made between individuals with FHP and normal individuals. In our study, however, the comparison was made between individuals with different severities of FHP, namely moderate-to-severe versus mild. Future studies are needed to confirm the results obtained in this preliminary study.
5.1. Limitation
The main limitation of this study is that we did not use precise tests such as an MRI to exclude cervical disorders that may affect balancing ability. We only conducted physical and radiological examinations for this purpose. Therefore, the possible presence of musculoskeletal disorders cannot be definitively ruled out. Other limitations of our study were the lack of a group with non-FHP people and the small sample size. Therefore, we recommend conducting further studies with an increased sample size to evaluate the LOS between individuals with different severity of FHP compared to non-FHP individuals.
On the other hand, a systematic review conducted by Lin et al. showed that current evidence supports an association between FHP and a detrimental alteration in the LOS (36). However, no study has determined the relationship between FHP severity and postural stability. Therefore, it is recommended that future research be designed to assess the relationship between FHP severity and balance measures.
5.2. Conclusions
The moderate-to-severe FHP group had longer RCT and MVL and a lower percentage of movement in performing the LOS test compared with the group with mild FHP. In other words, the individuals with moderate-to-severe grades of FHP showed decreased balancing ability compared to individuals with mild grades. A restricted LOS significantly influences the ability to react to perturbations in the balance control system. Therefore, it is necessary to design appropriate targeted interventions to prevent falls in individuals with FHP. Specifically, these individuals should receive balance exercises in dynamic situations.