1. Background
Cerebral palsy is a complex neurological disorder characterized by impaired muscle coordination and body movement (1). Its impact extends beyond the affected individual to profoundly affect their families, particularly mothers who often assume the primary caregiving role (2). The daily challenges associated with caring for a child with cerebral palsy can have substantial emotional, physical, and financial repercussions for mothers (3).
Mothers of children with cerebral palsy frequently experience heightened levels of stress, anxiety, and depression in comparison to mothers of typically developing children (2). The relentless demands of caregiving, frequent medical appointments, and the emotional strain of witnessing their child's struggles can lead to chronic stress and caregiver burnout (4). Moreover, the financial strain of raising a child with cerebral palsy can exacerbate the stress experienced by mothers, particularly if they are compelled to forgo work opportunities to provide full-time care. This amalgamation of emotional and financial strain can result in feelings of isolation and helplessness (5, 6). Since mothers usually have the main role of caring for a child with cerebral palsy, it is necessary to monitor the quality of life of parents. Healthcare professionals should be aware of this issue, have tools to assess the impact of factors affecting parents' quality of life, and make concerted efforts to plan and implement interventions that directly target mothers' psychological stress, empower them, and improve their overall well-being and quality of life (7). Improving the quality of life of mothers is an indirect way to intervene in children because they are responsible for supporting, caring for, and stimulating the growth and development of children (8).
The psychological symptoms and reduced quality of life that mothers of disabled children experience due to their conditions have a direct and significant impact on the growth and well-being of their children (4). The literature also shows that how parents cope with the situation, and how the family functions in general, has a major impact on how children deal with problems. Family functioning strongly affects children's treatment outcomes, as children rely heavily on their parents' support (6, 9-11).
Recent evidence has shown that psychosocial and behavioral interventions may be more effective in reducing emotional and psychological problems in mothers of children with cerebral palsy, while also increasing quality of life and promoting appropriate management strategies in the family, which also positively impacts the child and their family's functioning (12, 13).
Psychoeducation is defined as a specific treatment program with a focus on educational communication of information and providing coping skills to patients and families. It may be patient, parent, or school-focused (14). Family psychoeducation is a systematic approach that empowers patients and their families by focusing on developing emotional and cognitive skills to effectively manage the disease and any problems it may cause. The goal of this intervention is to foster relationship-building and shared responsibility between the patient and family for treatment adherence and outcomes (15).
While research on the effects of psychoeducation interventions for the caregivers of children with cerebral palsy is limited, some studies have explored similar programs for families dealing with other developmental disorders such as autism spectrum disorders (ASD), attention-deficit/hyperactivity disorder (ADHD), and intellectual disabilities (14, 16, 17). These studies found the benefits of psychoeducation for improving caregiver quality of life and reducing negative symptoms. Considering the diverse challenges faced by caregivers of children with cerebral palsy, as well as their pivotal role in treatment, the present study aimed to examine the impact of group psychoeducation on caregiver anxiety, depression, and quality of life.
While research on psychoeducational interventions for mothers of children with developmental disorders in Iran is still limited, some international studies have explored this area. A few existing investigations examined the impact of psychoeducation on caregivers and mothers of children with chronic conditions (18, 19). Additionally, several investigations evaluated the effectiveness of educational programs for caregivers of children with developmental disorders and cerebral palsy. These studies highlighted the significance of educating caregivers in mitigating care-related issues for children and enhancing the quality of life for both children and their families (20-22).
The studies highlighted that psychoeducational interventions for caregivers have the potential to resolve issues arising from childcare responsibilities, while also enhancing the well-being of children and their families. Overall, the findings emphasized empowering caregivers with knowledge and skills can lead to positive outcomes for both the children and their families.
As cerebral palsy can influence various physical and psychological dimensions of both affected children and their families, it is posited that the results of this study may help to enhance functioning and well-being within this population. The overarching aim of this study is to examine the impact of a psychoeducation program on anxiety, depression, and quality of life in mothers of children with cerebral palsy. Specifically, the study aims to: (1) Evaluate whether participation in a psychoeducation program reduces symptoms of anxiety and depression in mothers of children with cerebral palsy, compared to a control group not receiving the intervention; (2) Assess whether participation in a psychoeducation program improves quality of life domains for mothers of children with cerebral palsy, such as physical health, psychological health, social relationships, and perceptions of environmental support systems.
2. Objectives
This study seeks to contribute new knowledge on supportive interventions for families affected by cerebral palsy that have the potential to enhance their well-being and coping abilities while caring for a child with special needs. The results may help identify best practices for psychoeducation programming to support this important population.
3. Methods
3.1. Study Design
This randomized controlled trial evaluated the efficacy of a psychoeducation intervention for mothers of children with cerebral palsy. The study was conducted between May 2018 and September 2019.
3.2. Participants
A total of 52 mothers of children diagnosed with cerebral palsy were invited to participate through voluntary sampling from rehabilitation clinics in Semnan, Iran, and assigned to experimental and control groups. Based on a preliminary study with 14 participants, a power analysis using the formula for sample size calculation for a single population proportion (23) determined a final sample size of 24 per group was needed to detect a difference with 95% power and an alpha of 0.05:
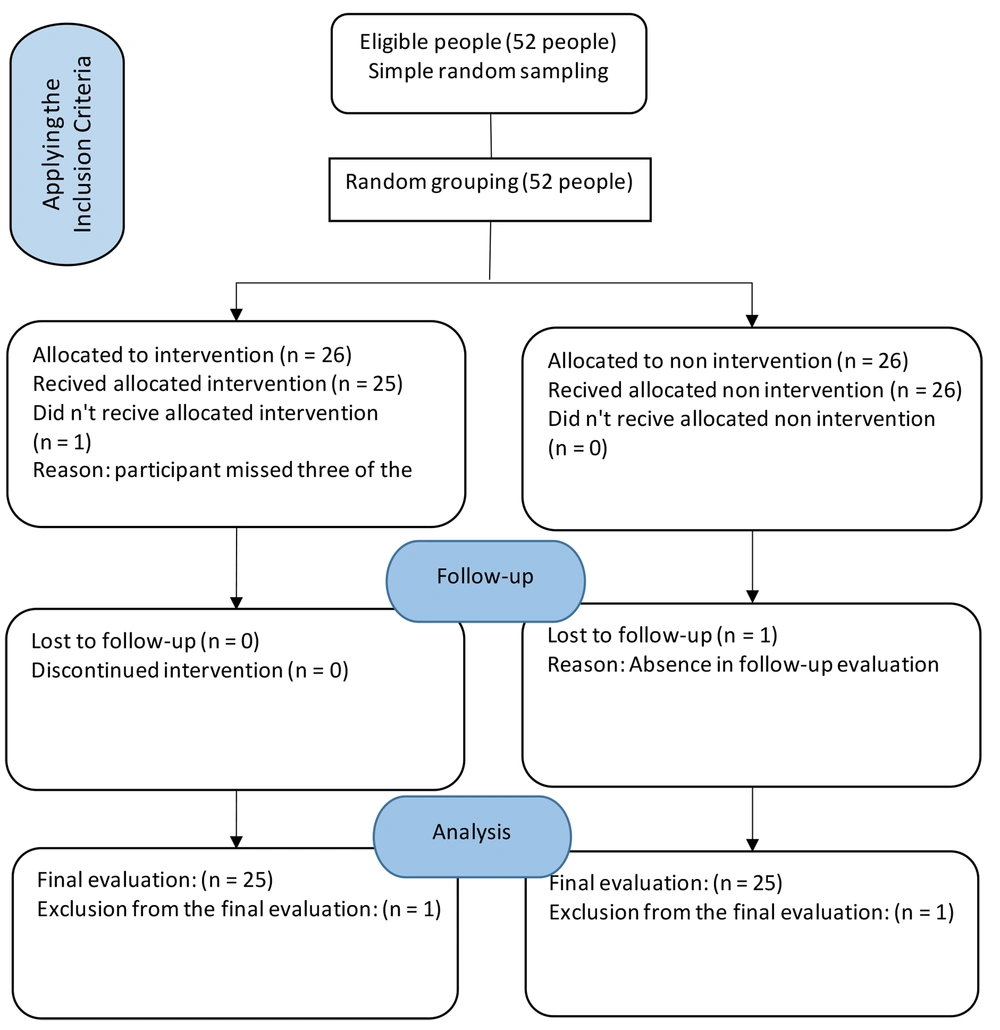
To account for possible dropouts or exclusions, the final sample size recruited for each group in the main study was set at 26 participants. Participants were randomly divided into experimental and control groups using simple randomization. In this method, first natural numbers from 1 to 52 were written in equal numbers on pieces of paper. Then the cards were randomly distributed among the participants. Even numbers were assigned to the experimental group and odd numbers to the control group.
The inclusion criteria for children were: Having a confirmed diagnosis of cerebral palsy according to a pediatric neurologist, age between 2 - 11 years, and being at levels 3 to 5 on the Gross Motor Function Classification System (GMFCS) scale. The inclusion criteria for mothers were: Being married, aged 18 - 45 years, having a primary education level of literacy, and having sufficient cognitive skills to participate in the group sessions.
The exclusion criteria for children included: Having comorbid conditions such as uncontrolled seizures and severe intellectual disability. The exclusion criteria for mothers included: Having a history of any psychiatric or disabling medical conditions such as neurological or orthopedic disorders, caring for other children with developmental disorders or chronic illnesses, or failing to attend more than one intervention session.
3.3. Measures
This study employed three standardized questionnaires to measure key variables: The Beck Anxiety Inventory (BAI), the Beck Depression Inventory-II (BDI-II), and the 36-item Short Form Health Survey (SF-36). Additionally, a demographic questionnaire collected descriptive data such as the mothers' age, marital status, number of children, and the age of the child with cerebral palsy, providing context for the research findings.
The Beck Anxiety Inventory (BAI) measures anxiety with 21 items rated on a 4-point severity scale from 0 to 3, yielding total scores from 0 - 63, with higher scores indicating increased anxiety. The BAI is known for its strong internal reliability (α = 0.92) and test-retest consistency (r = 0.75) and has shown reliability and validity within Persian-speaking populations (24).
Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II), a 21-item self-report measure of depression where respondents rate each item from 0 to 3 based on symptom severity over the past two weeks, resulting in scores ranging from 0 to 63. The BDI-II is noted for its strong internal consistency (α ≥ 0.86) and adequate test-retest reliability (r ≥ 0.73). It includes established cut-off scores to indicate minimal, mild, moderate, and severe levels of depression (25).
Health-related quality of life was measured using the Medical Outcomes Study 36-item Short Form Health Survey (SF-36), a validated instrument that produces eight subscale scores and two composite scores for physical and mental health. The Persian version of the SF-36 has been validated and is reliable for measuring quality of life. These standardized, validated questionnaires allowed for reliable and valid assessment of the key study variables in the sample population, with previous research supporting their psychometric properties in Persian samples (26).
3.4. Process of Implementation
The present study employed a multi-step methodology. First, participants were voluntarily recruited from patients at rehabilitation clinics in Semnan. A comprehensive list of all active clinics in the city was obtained, identifying six facilities. Advertisements inviting patient collaboration were then distributed to each clinic. Recruitment continued until the target sample size was reached. Subsequently, recruited participants were provided with information about the study and asked to provide informed consent. Baseline information was gathered using a demographic questionnaire, and assessments of anxiety, depression, and quality of life were conducted using the Beck Anxiety Inventory (BAI), the Beck Depression Inventory-II (BDI-II), and the 36-item Short Form Health Survey (SF-36), respectively.
Participants were then randomly allocated to either the intervention (n = 26) or control (n = 26) group. The intervention group received a 5-session psychoeducation program consisting of group-based educational and supportive therapy interventions, with each session lasting approximately 90 minutes. This program was conducted by an expert psychotherapist. The control group did not receive any intervention during this period. Post-intervention assessments using the same questionnaires were administered immediately following the completion of the 5 sessions. Follow-up assessments were also conducted 2 months later to examine longer-term effects.
To maintain objectivity, all assessments—including those conducted at pre-intervention baseline, post-intervention, and during follow-up periods—were administered by a trained examiner, a fourth-year occupational therapy student, who was blinded to group assignment and uninvolved in delivering the psychoeducation program or other aspects of the intervention. This approach helped reduce potential biases from lack of blinding during outcome evaluation. This randomized controlled trial follows the CONSORT 2010 guidelines for reporting (27).
Details of the psychoeducation program administered to the experimental group are provided in Table 1. Each session had specific educational and therapeutic aims and involved various activities and discussions. The control group did not participate in any such intervention during the study period.
| Session | Topic | Time (min) | Resources |
|---|---|---|---|
| 1 | Introduction to training session objectives, introduction to cerebral palsy, prevalence and etiology, symptoms and signs, types and prognosis. | 70 | Children with cerebral palsy: A manual for therapists, parents and community workers (28) |
| 2 | Introduction to problems in children with cerebral palsy, associated disorders, and also secondary problems in these children such as social problems. | 90 | |
| 3 | Introduction to common treatments including medical treatments and physiotherapy interventions, introduction to new treatments, and review of treatment characteristics. | 90 | Cerebral Palsy: A Multidisciplinary Approach (29) |
| 4 | Review of parents' problems such as lack of acceptance, shame and isolation, anxiety and depression, and coping strategies. | 90 | Finnie's Handling the Young Child with Cerebral Palsy at Home (30) |
| 5 | Teaching coping strategies, special care of these children, and handling | 120 | Learning supportive psychotherapy: An illustrated guide (31) |
Training Sessions Schedule for Intervention Group
3.5. Statistical Analysis
The results of the study were statistically analyzed using chi-square tests, paired sample t-tests, independent t-tests, and one-way repeated measures ANOVA. Statistical analyses were conducted using SPSS Version 22. The Shapiro-Wilk test was utilized to evaluate the normal distribution of the data before conducting the parametric tests, ensuring the assumptions for using paired t-tests and repeated measures ANOVA were met.
3.6. Ethical Considerations
This study received ethical approval from the Semnan University of Medical Sciences Research Ethics Board (IRB approval number IR.SEMUMS.REC.1397.259) before commencement. All relevant ethical guidelines were adhered to, including maintaining patient anonymity, obtaining voluntary informed consent, and ensuring patient safety. The study was prospectively registered in the Iranian Registry of Clinical Trials (registration number IRCT20181130041807N1).
4. Results
A total of 52 mothers of children with CP participated in this study. Two were excluded due to rejection (Figure 1). All participants were married, lived in urban areas, and had elementary to secondary levels of education. The mean age was 32.04 years in the experimental group and 31.16 years in the control group, with ages ranging from 23 to 45 years. The data were normally distributed.
Statistical analysis of demographic and baseline data revealed no significant differences between the intervention and control groups in terms of age, gender, and initial evaluation scores. This homogeneity was confirmed using standard statistical tests (Table 2).
| Variables | Group | |
|---|---|---|
| Intervention | Control | |
| Mothers age | 32.04 (4.42) | 31.16 (2.98) |
| Child sex | ||
| boy | 14 (28.0) | 13 (26.0) |
| girl | 11 (22.0) | 12 (24.0) |
| CP Diagnosis | ||
| Spastic | 19 (38) | 17 (34) |
| Dyskinetic | 1 (2) | 4 (68) |
| Ataxic | 4 (8) | 4 (8) |
| non | 1 (2) | 0 (0) |
Demographic Characteristics of Participants a
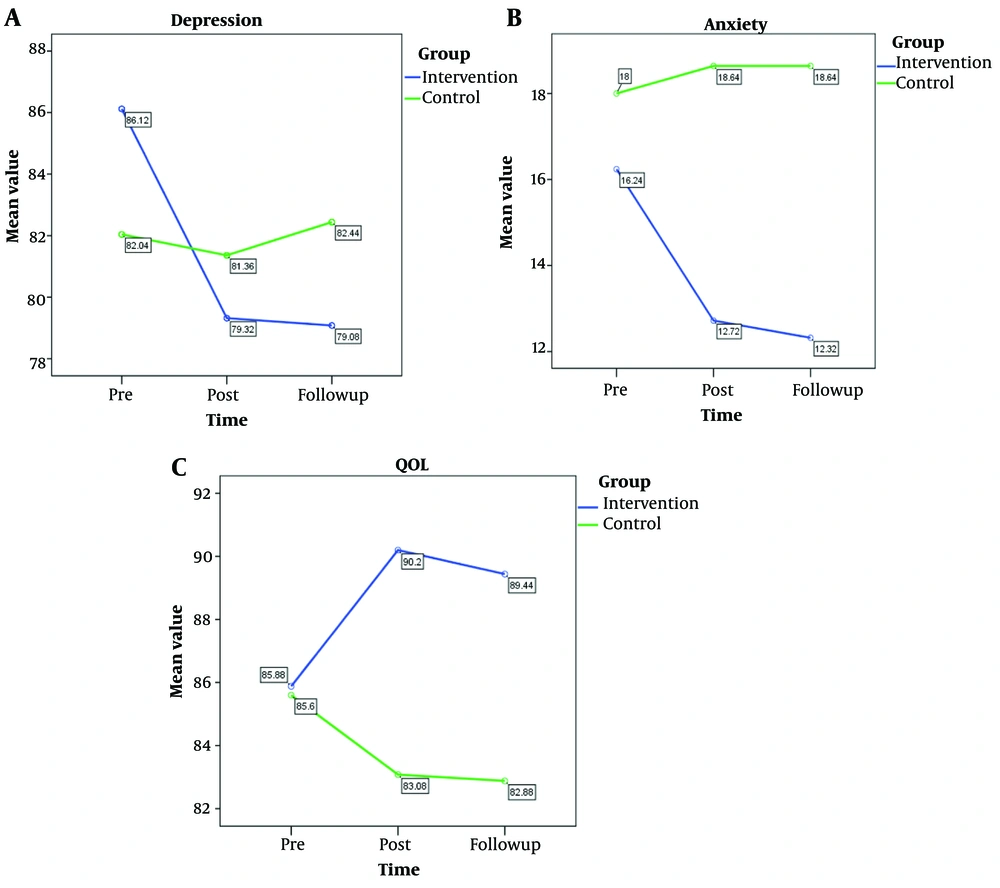
As shown in Table 3, the mean and standard deviation of outcome measures were calculated for both groups at various assessment points. Statistical analysis revealed no baseline differences between the arms on any of the factors prior to the start of the study intervention (P > 0.05). Following completion of the intervention period however, scores on two key measures - Beck Anxiety Inventory (BAI) and short form 36 (SF36) - were significantly varied between the groups at later follow-up assessments, with p-values below typical thresholds (P < 0.05).
The results uncovered significant differences within the subjects in the BDI, BAI, and SF36 (P < 0.001). Moreover, the within-subject results showed that all variables significantly changed over time (P < 0.001).
| Variables | Intervention (N = 53) | Control (N = 53) | P-Value |
|---|---|---|---|
| BDI | |||
| Pre | 86.12 ± 14.47 | 8204 ± 14.45 | 0.332 |
| Post | 79.32 ± 11.13 | 81.36± 14.87 | 0.586 |
| F | 79.08 ± 11.06 | 82.44 ± 14.50 | 0.362 |
| P-value | 0.014 | 0.178 | - |
| BAI | |||
| Pre | 16.24± 13.25 | 18.0 ± 10.67 | 0.607 |
| Post | 12.72± 9.74 | 18.64 ± 10.26 | 0.042 |
| F | 12.32 ± 10.97 | 18.64 ± 9.99 | 0.017 |
| P-value | 0.018 | 0.903 | - |
| SF36 | |||
| Pre | 88.85 ± 7.16 | 85.60 ± 6.42 | 0.885 |
| Post | 90.20 ± 7.17 | 83.08 ± 6.70 | 0.001 |
| F | 89.44 ± 6.60 | 82.88± 6.54 | 0.001 |
| P-value | 0.036 | 0.067 | - |
Mean and Standard Deviation Values of the Studied Variables Between the Two Groups at Different Times a
Figure 2 displays the fluctuations in average values of analyzed variables over different time intervals, including BDI, BAI, and SF36 measures, indicating significant group × time interaction effects (P < 0.001). The Cohen's d-effect size analysis confirmed a notable impact of the intervention, with scores decreasing significantly (d > 0.5) across all variables.
5. Discussion
This study investigated the impact of a group psychoeducational intervention on anxiety, depression, and quality of life among mothers of children with cerebral palsy. The results confirmed that the intervention significantly alleviated anxiety and depression, and enhanced quality of life.
Research underscores that parents, particularly mothers, of children with cerebral palsy often endure significant emotional strain, contributing to a decline in their overall well-being and quality of life due to persistent stress, depression, and chronic sorrow (6, 32). Although psychoeducational therapy is recognized as an effective treatment for anxiety and depression, relatively few studies have specifically focused on parents of children with developmental disorders like cerebral palsy (33).
Recent studies suggest that psychoeducation can mitigate anxiety by encouraging patients not to suppress emotions but instead to strive for balanced relationships and attend to personal needs. Recognizing feelings of loneliness and inadequacy plays a crucial role in this process (34-36). Moreover, skills such as overcoming submissiveness, adjusting locus of control, and enhancing social support have been shown to effectively reduce anxiety levels (37). For mothers of children with cerebral palsy, the unpredictability of the disorder and a lack of understanding about their child’s condition are significant sources of anxiety, which psychoeducation can help alleviate by improving knowledge and awareness (38).
Picard et al. highlighted that group psychoeducational therapy facilitates better parent-therapist interactions and fosters social support by providing crucial information, thus enhancing service reception and reducing stress (39).
Mothers of children with cerebral palsy often struggle with the complexity and demands of their children's treatment, which can lead to depression and diminish their quality of life. The multifaceted nature of cerebral palsy requires a multidisciplinary approach to foster improvements and facilitate positive changes. Managing a chronic condition involves a complex set of behaviors that incorporate information, skills, attitudes, values, and environmental supports. One crucial goal of psychoeducation is to familiarize caregivers with the disease, its side effects, treatment options, and the recovery process (40).
The intervention in this study provided substantial information and education to parents, which appeared to be beneficial. Jahagirdar demonstrated that psychoeducation effectively increased parents' knowledge and awareness about cerebral palsy (33). Similarly, Khanjani et al. conducted a study that taught caregivers proper care techniques for children with cerebral palsy using an educational guide. After training caregivers according to recommended care practices, the study found that the psychoeducation intervention significantly improved the caregivers' quality of life across various domains (41).
In this study, the psychoeducation intervention was delivered in a group setting, leveraging the inherent benefits of group dynamics. Sharing concerns and solutions within the group can enhance problem-solving strategies and foster a sense of community among participants (42). This aspect is especially valuable for mothers who, as primary caregivers, often have limited time for other activities due to the intensive care requirements of their children. Additionally, the dynamic changes within the family system necessitate that all members adapt to new roles and responsibilities (43).
Psychoeducation in psychotherapy can significantly benefit individuals by increasing their understanding of psychological issues, thereby improving their problem-solving abilities and developing more effective coping strategies. This enhancement of mental health capabilities empowers individuals to better manage challenges to their well-being, ultimately elevating their quality of life by providing insights and skills that promote healthy psychological functioning (44). However, not all studies have found psychoeducation to be effective. For instance, Ferrin et al. reported no significant changes in depression or stress levels following a psychoeducation program for parents of children with ADHD. This intervention was delivered individually rather than in a group setting, which may have lacked the social support component that has been shown to be important. Additionally, their sample size was smaller (45).
A systematic review by Dahl et al. indicated that a small number of studies were unable to demonstrate the effect of psychoeducation on the stress and depression of caregivers of children with developmental disorders, noting that most of these studies had limitations such as small sample sizes, which may have hindered their ability to detect significant effects (14). Future research with more robust study designs is necessary to fully evaluate the potential benefits of psychoeducation interventions for caregivers of children with developmental disorders.
5.1. Limitations and Recommendations
This study had certain limitations that should be acknowledged. One limitation was the lengthy duration of sessions, which could lead to fatigue and reduce participants' willingness to continue attending. Another limitation was the lack of cooperation and inactivity of some participants during therapy sessions. Although the results of this study were reasonably consistent with our findings, it is suggested that future studies compare the impacts of this intervention with other educational and psychological interventions. Additionally, the effect of psychoeducation on other individual and social components of parents of children with cerebral palsy and other developmental disorders should be examined.
5.2. Conclusions
This study demonstrated the significant effectiveness of group psychoeducation in improving the mental health and quality of life of mothers caring for children with cerebral palsy. The findings underscore the valuable role of psychoeducational programs in alleviating symptoms of anxiety and depression, enhancing caregiver well-being, and addressing the unique challenges faced by those caring for individuals with chronic conditions. The results also have implications for rehabilitation and occupational therapy services working with children with cerebral palsy. Psychoeducation programs can empower caregivers to better support their child's rehabilitation needs at home, potentially improving treatment adherence, engagement in therapy, and functional outcomes for children. Moreover, the sustained benefits observed over time indicate the lasting positive impact of psychoeducation. Rehabilitation professionals could consider incorporating brief psychoeducational modules into routine care to continuously support caregivers. Occupational therapists, in particular, are well-positioned to provide psychoeducation on managing daily living activities and promoting independence. Further research should explore the scalable implementation of psychoeducational programs across contexts, compare interventions to optimize caregiver support, and investigate long-term effects. Overall, the findings advocate for integrating psychoeducation as a fundamental component of holistic care for not only caregivers but also the individuals they support, enhancing rehabilitation and occupational therapy services.