1. Background
Heart failure (HF) is a chronic and complex syndrome that causes functional damage to the heart, with an estimated 64.3 million patients worldwide suffering from HF (1). Complications arising from heart dysfunction and the resulting symptoms can lead to difficulties in performing activities of daily living (ADL) (2). The prevalence of ADL impairment in HF patients is notably high, with variations likely influenced by region, country, assessment tools, and time (3).
Activities of daily living plays a crucial role in preventing readmission of HF and mortality. Furthermore, a decline in ADL in HF has been linked to a poor prognosis (4). Katano et al. found that ADL was a predictor of mortality in HF patients (5). According to Dunlay et al., difficulties with ADL were associated with a negative impact on quality of life and care needs, as well as an increased risk of hospitalization and death (6). The ability to perform ADLs is essential for patients to meet their basic needs, and it serves as a measurement tool for their health conditions. In conclusion, patients with HF often face difficulties with ADLs, and their ability to perform ADLs significantly impacts their health conditions (7). Early evaluation of ADLs is crucial for implementing proper interventions in HF patients, highlighting the need for an accurate ADL assessment questionnaire.
There are three ADL assessment questionnaires for HF patients: The Kansas City Cardiomyopathy Questionnaire (KCCQ) (8), the Performance Measure for Activities of Daily Living-8 (PMADL-8) (9), and the Daily Activity Questionnaire in Heart Failure Scale (DAQIHF) (10). The KCCQ is a 23- or 12-item questionnaire that provides a comprehensive evaluation of the patient's health status, including symptom frequency, physical limitations, social limitations, and quality of life domains (11). The PMADL-8 assesses 8 items: Rising from the floor without assistance, showering, climbing stairs without a railing, vacuuming, sliding a heavy door, getting in and out of a car, walking alongside someone of similar age, and walking uphill for 10 minutes (9). The DAQIHF is a daily activity questionnaire used to assess the daily energy expenditure of HF patients (10).
These ADL assessment questionnaires do not adequately assess the full spectrum of patients' daily activities, which may limit their ability to accurately improve patient outcomes and prevent the development of conditions that could impact daily functioning in the context of disease management and treatment plans.
However, these questionnaires did not comprehensively assess ADL, and the number of parameters they evaluated was limited. In an ADL assessment questionnaire for HF patients, it is crucial to examine parameters related to ADL, such as independence, fatigue, dyspnea, pain, and performance time, because these factors affect performance in HF (12). Additionally, cultural differences could lead to a different conceptualization of ADL (13).
Therefore, a standardized, validated measure of limitations in ADL in patients with HF is needed. Developing a questionnaire that can accurately assess and determine these parameters in all ADL activities and identify the limitations for each activity is essential.
2. Objectives
The aim of this study is to develop an ADL assessment questionnaire that includes parameters affecting ADL.
3. Methods and Results
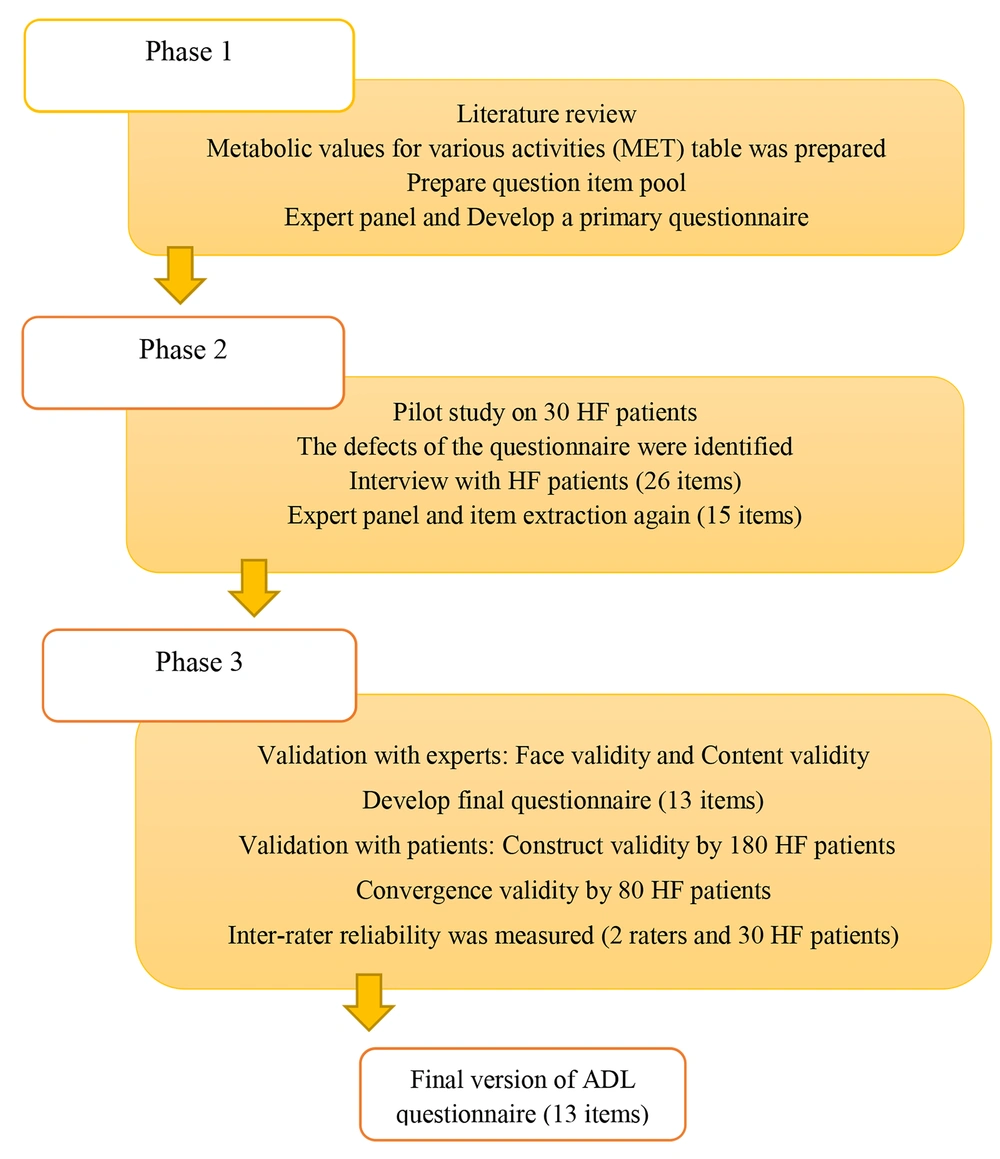
This study conducted methodological research in 2016 with the aim of developing and evaluating an ADL assessment questionnaire for the Iranian population. The development and evaluation of the scale were based on a sequential exploratory mixed-method study, with scoring based on the Likert Scale. The three stages included the definition of the concept to be measured, the development of assessment tools, and the calculation of validity and reliability (Figure 1) (14).
3.1. Questionnaire Development
The first phase involved studying literature on ADL questionnaires and models, with the occupational therapy practice framework (OTPF) being chosen as the framework. Scientific databases such as PubMed, Elsevier, Scopus, Web of Knowledge, and the Cochrane Library were searched. All ADL assessment tools were gathered, and the MET table for various activities, as well as occupational therapy models and frameworks, were examined.
The MET table defined activities with varying required oxygen consumption, encompassing both BADL and IADL activities in ADL assessment tools and activities in the OTPF. The sets of activities and parameters were inputted into the initial questionnaire. These parameters included fatigue, dyspnea, pain, value, independence, safety, difficulty, and performance time, sourced from occupational therapy and qualitative work. Following expert panel meetings and gathering opinions, the questionnaire was revised, leading to the preparation of the initial questionnaire. A team of five experts, including three with doctorates in occupational therapy, one with a doctorate in neuroscience, and one with a doctorate in physiotherapy, were involved. Individuals classified as level four of the New York Heart Association (NYHA) were excluded due to their significant limitations in physical activity. Consequently, as advised by the cardiologist, only patients categorized as levels 1 - 3 were considered for the study.
In the next phase, this form was piloted with 30 people with HF. To improve item generation, a qualitative study was carried out involving semi-structured interviews with 12 individuals at different levels of HF, using purposive sampling. The interviews were audio-recorded and transcribed directly by an occupational therapist. The focus was on HF patients' views and recommendations on questionnaire items and parameters. The first author conducted an inductive analysis and thematic evaluation of the qualitative data from the interviews. Items identified in the qualitative study were compared to the initial form. Analogical-inductive methods were used to prepare the items. Following the preparation of the form (pool of questions), the expert panel convened to gather opinions on the items in the form (15 items). Based on expert feedback, some items were combined and others were renamed. The final questionnaire (13 items) was then prepared, incorporating expert opinions, and the psychometric evaluation phase commenced.
Based on the expert panel's opinions, the questionnaire has been revised. Activities such as eating, using communication devices, performing artistic works, financial management, and caring for others have been removed. The decision to exclude light activities like eating was based on low energy consumption according to the MET table, and it is only applicable in advanced stages of the disease (15, 16). Similarly, using communication devices and performing artistic works are not universally applicable due to varying levels of education and interest. The item of financial management was removed as severe cognitive involvement occurs only in level 4 NYHA of HF, which is not applicable to levels 1 to 3 (17). Caring for others was also removed due to its lack of generality for all patients and its similarity to child care duties. Additionally, based on the OTPF, mobility and movement items were divided into functional mobility and community mobility (18).
3.2. Ethical Considerations
This study was approved by the Research Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.REC.1395.95-03-32-28606) informed consent forms were signed by both the experts and HF patients.
3.3. Data Analysis
The statistical analysis was performed using SPSS, version 18. To evaluate face validity, feedback was received from 15 therapists and 30 HF patients regarding the items and questionnaire parameters. Content validity was determined by calculating the Content Validity Index (CVI) and content validity ratio (CVR). For construct validity, 180 ADL questionnaires were completed by HF patients and exploratory factor analysis (EFA) was conducted. Convergent validity was assessed by having 80 HF patients complete both the ADL questionnaire and the ADL section of the Iranian Heart Failure Quality of Life (IHF-QoL). The correlation between these two questionnaires was measured using Pearson's correlation coefficient. Reliability was checked by two raters and 30 HF patients over a 2-week period, and internal consistency was determined using Cronbach's alpha coefficient.
3.4. Face Validity
To assess face validity, 15 therapists reviewed the questionnaire items, while HF patients provided their feedback on the items and questionnaire parameters. Among the therapists, three were nurses, five were physiotherapists, and seven were occupational therapists. The item effects ranged from 2.43 to 5, leading to no items being removed and 15 items being prepared for content validity assessment. The literature recommends that a focus group of between 10 and 20 participants is ideal for assessing face validity (19).
3.5. Content Validity
The expert ratings were used to calculate content validity at the item level using the CVI and CVR. The CVI was calculated based on the ratings given by experts, with items rated as 3 or 4 being considered relevant. Items with a CVI equal to or greater than 0.79 are considered relevant (20). To assess face validity, the opinions of 15 medical personnel who work with individuals with HF were gathered. For content validity, the opinions of 8 experts with knowledge and experience in questionnaire development, occupational therapy, and working with individuals with HF were collected. Following the expert opinions, 20 medical personnel in contact with individuals with HF were asked to complete the CVI and CVR-related forms. Studies recommend using 5 to 10 experts for content validation (21).
3.6. Construct Validity
Using the convenience sampling method, 180 individuals with HF at NYHA levels 1 - 3 from an outpatient HF clinic at Shahid Rajaie Cardiovascular, Medical and Research Center participated in this study. Norman and Streiner state that factor analysis is a large-sample procedure, recommending an arbitrary sample size of 100 to 200 (22). Exploratory factor analysis is used in medical education research to develop instruments for assessing latent variables that cannot be directly measured. Researchers select instrument items based on literature review and expert input to represent a construct like professionalism and use factor loadings and other criteria to refine the measure (23). In this study, the EFA method was used to determine construct validity. To assess the data's suitability for EFA and sample size adequacy, the KMO and Bartlett's Sphericity tests were performed.
To assess convergence validity, 80 HF patients completed both the ADL questionnaire and the ADL section of the IHF-QoL questionnaire. The IHF-QoL questionnaire showed acceptable convergent validity, with a Cronbach's alpha of 0.92 and a significant ICC for all components (24). The correlation between the two questionnaires was evaluated using Pearson's correlation coefficient.
3.7. Reliability
Reliability was evaluated by two raters and 30 HF patients on two occasions, two weeks apart, and internal consistency was determined using Cronbach's alpha coefficient. Inter-rater reliability was assessed using the intraclass correlation coefficient (ICC). The ICC results were categorized as poor (0.5), moderate (0.5 - 0.75), good (0.75 - 0.9), and excellent (> 0.9) (25). Pearson correlations and ICC are influenced by the score range. Calculating the proportion of agreement of test-retest differences with a referent value of ±1 could offer more insight into the questionnaire's stability (26).
The initial questionnaire was completed by 30 individuals with HF, with 53% (16 people) being male and 46% female. Participants' ages ranged from 22 to 65 years old, with a mean (SD) age of 50.57 (11.3). Among the participants, 8 people (25%) were at level I, 14 people (43%) were at level II, and 8 people (25%) were at level III of the NYHA functional class. Additionally, 8 (25%) individuals were admitted to the hospital, while 22 (75%) were not. The average duration of HF among the participants was 5.6 (4.4) years.
To perform face validity, the HF patients provided their opinions and suggestions regarding the items and parameters of the questionnaire. Interviews with HF patients at different levels of NYHA were conducted, and 26 items from the initial questionnaire and results of the interviews were extracted. To review the content of the questionnaire, three sessions were held with eight experts, including five individuals with doctorates in occupational therapy, one with a doctorate in neuroscience, one with a doctorate in physiology, and one with a doctorate in physiotherapy. After applying the suggested changes, 15 items remained. These items include: Excretion of urine and feces, dressing, bathing, functional mobility, social mobility, sexual activities, using public transportation, driving, taking care of one's health, performing individual religious duties, carrying out duties related to child care, traveling, duties at home, caring for animals and plants, and self-grooming.
To check face validity, 15 therapists commented on the items of the questionnaire. Three were nurses (experts in the HF department), five were physiotherapists (master's degree), and seven were occupational therapists (master's degree). The effect of items ranged between 2.43 and 5. In this way, no items were deleted, and 15 items were prepared for content validity.
To check the content validity of the questionnaire, a meeting was held with eight experts and research team members. The panel included three cardiologists specializing in HF (5 to 13 years of professional experience), eight masters in occupational therapy (2 to 8 years of professional experience), six masters in physical therapy (2 to 12 years of professional experience), and three bachelor-level nurses (10 to 15 years of professional experience). The questionnaire, with the remaining 15 items and the given changes, was prepared to check the quantitative content validity (CVI and CVR).
Twenty experts (eight occupational therapists, six physiotherapists, three cardiologists, and three cardiac nurses) completed the questionnaire at this stage to determine the CVI and CVR (Tables 1 and 2). According to the critical value suggested by the Lawshe table, items with a content validity index of less than 0.42 should be removed from the questionnaire. The total content validity of the questionnaire (CVI-s) was calculated as 0.91. Two items were deleted: The self-grooming item with an I-CVI of 0.65, and the animal and plant care item with an I-CVI of 0.7 and a CVR of -0.2.
| Numbers | Items | Essential | Useful But Not Essential | Unessential | CVR | Interpretation |
|---|---|---|---|---|---|---|
| 1 | Excretion of urine and feces (sitting and standing up, maintaining the situation in the toilet, transfer to the toilet) | 15 | 4 | 1 | 0.5 | Remained |
| 2 | Self-grooming (correction of body hair, nail care) | 12 | 7 | 1 | 0.2 | Eliminated |
| 3 | Self-dressing (flexion and extension for wearing clothes and closing shoelace) | 19 | 1 | - | 0.9 | Remained |
| 4 | Take a bath (change the position in the bathroom and during washing, entering, and exiting the bathroom) | 20 | - | 1 | 1 | Remained |
| 5 | Functional mobility Easy: Sitting and standing, bending and straightening moderate: Fast walking, transfer to car difficulty: Climbing ramps, going up and down stair | 20 | - | - | 1 | Remained |
| 6 | Social mobility (shopping, going to do banking, walking with carrying things) | 20 | - | - | 1 | Remained |
| 7 | Sexual activities (participating in an activity that results in sexual satisfaction or pregnancy) | 19 | 1 | - | 0.9 | Remained |
| 8 | Use of public transportation (standing on a bus for a long time, using a plane, using the subway to travel) | 17 | 3 | - | 0.7 | Remained |
| 9 | Caring for animals and plants (flowering, taking care of animals and flowers) | 8 | 9 | 3 | -0.2 | Eliminated |
| 10 | Driving (independent transfer in society with their own car) | 17 | 2 | 1 | 0.7 | Remained |
| 11 | Taking care of your health (using a proper diet, exercising, managing your medication ) | 17 | 3 | - | 0.7 | Remained |
| 12 | Carrying out individual religious duties (how to pray (sitting or standing), bending, straightening, doing meditation) | 16 | 4 | - | 0.6 | Remained |
| 13 | Tasks related to taking care of the child (spending time for issues related to the child, spending time with the child) | 11 | 9 | - | 0.1 | Remained |
| 14 | Traveling (the ability to sit for a long time in a vehicle) | 12 | 7 | 1 | 0.2 | Remained |
| 15 | Housekeeping tasks (sweeping, making the bed, washing dishes, ironing, cooking, interior repairs, dusting and house cleaning) | 18 | 2 | - | 0.8 | Remained |
Calculating content validity ratio (CVR) for the Heart Failure Activities of Daily Living (ADL) Questionnaire
| Numbers | Items | Not Relevant | Somewhat Relevant | Acceptable Relevant | Very Relevant | CVI | Interpretation |
|---|---|---|---|---|---|---|---|
| 1 | Excretion of urine and feces (sitting and standing up, maintaining the situation in the toilet,transfer to the toilet) | 1 | - | 3 | 16 | 0.95 | Remained |
| 2 | Self-grooming (correction of body hair, nail care) | 3 | 4 | 8 | 5 | 0.65 | Remained |
| 3 | Self-dressing (flexion and extension for wearing clothes and closing shoelace) | - | 1 | 3 | 16 | 0.95 | Remained |
| 4 | Take a bath (change the position in the bathroom and during washing, entering, and exiting the bathroom) | - | - | - | 20 | 1 | Remained |
| 5 | Functional mobility Easy: Sitting and standing, bending and straightening moderate: Fast walking, transfer to car difficulty: Climbing ramps, going up and down stair | - | - | 1 | 19 | 1 | Remained |
| 6 | Social mobility (shopping, going to do banking, walking with carrying things) | - | - | 1 | 19 | 1 | Remained |
| 7 | Sexual activities (Participating in an activity that results in sexual satisfaction or pregnancy) | - | 1 | 3 | 16 | 0.95 | Remained |
| 8 | Use of public transportation (standing on a bus for a long time, using a plane, using the subway to travel) | - | - | 2 | 18 | 1 | Remained |
| 9 | Caring for animals and plants (flowering, taking care of animals and flowers) | 3 | 3 | 9 | 5 | 0.7 | Eliminated |
| 10 | Driving (independent transfer in society with their own car) | - | 2 | 5 | 13 | 0.9 | Remained |
| 11 | Taking care of your health (using a proper diet, exercising, managing your medication ) | 1 | 1 | - | 18 | 0.9 | Remained |
| 12 | Carrying out individual religious duties (how to pray (sitting or standing), bending, straightening, doing meditation) | - | - | 4 | 16 | 1 | Remained |
| 13 | Tasks related to taking care of the child (spending time for issues related to the child, spending time with the child) | 1 | 2 | 9 | 8 | 0.85 | Remained |
| 14 | Traveling (the ability to sit for a long time in a vehicle) | 1 | 1 | 6 | 12 | 0.9 | Remained |
| 15 | Housekeeping tasks (sweeping, making the bed, washing dishes, ironing, cooking, interior repairs, dusting and house cleaning) | - | 2 | 2 | 16 | 0.9 | Remained |
| S-CVI average | 0.91 | ||||||
Calculating Content Validity Ratio (CVI) for the Heart Failure Activity of Daily Living (ADL) Questionnaire
After collecting the opinions of experts, 13 items (urinating and defecating, dressing, bathing, functional mobility, social mobility, sexual activities, using public transportation, driving, taking care of one's health, performing personal religious duties, performing child care duties, traveling, and tasks at home) remained in the questionnaire. The questionnaire was completed by 180 people with HF at NYHA levels 1 - 3. Among the participants, 65% (117 people) were male and 35% were female. The participants' ages ranged from 18 to 65 years old, with a mean (SD) age of 50.12 (12.49). A total of 83 people (46.1%) were at level I, 58 people (32.2%) were at level II, and 39 people (21.7%) were at level III of the NYHA functional class.
The KMO and Bartlett’s sphericity test results are shown in Table 3. The KMO sampling adequacy index was 0.86, and Bartlett’s test of sphericity was statistically significant (χ2 = 557.52, P < 0.001). The KMO exceeding the recommended value of 0.6 indicates sampling adequacy (27).
| Variables | Values |
|---|---|
| KMO | o.86 |
| Bartlett's test of Sphericity | 557.52 |
| Df | 28 |
| P | < 0.01 |
Results of Sampling Adequacy Test for EFA
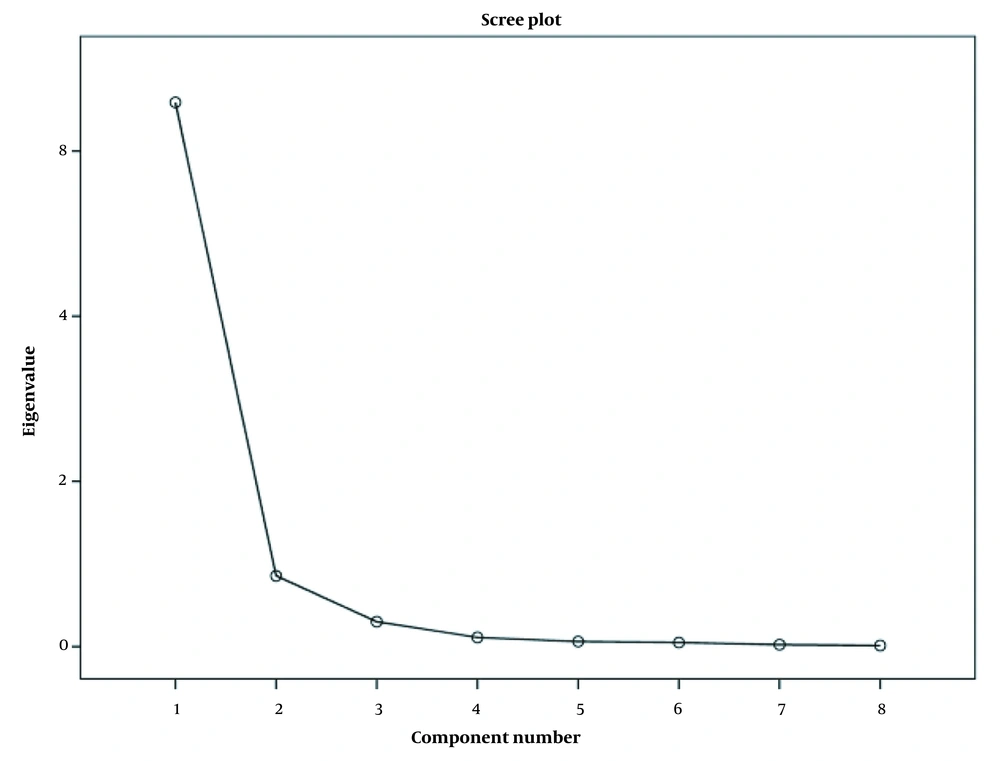
The scree plot (Figure 2) suggested that two factors must be retained, but varimax rotation indicated that three factors were necessary. Table 4 depicts that the EFA proposed a three-factor model. Considering the conceptual commonalities between the variables, we labeled factor one as value, safe independence, and signs and symptoms. The first factor, signs and symptoms, encompassed dyspnea, pain, duration of activity, and difficulty. Safe independence constituted the second factor, involving safety and independence, while the third factor, value, consisted of just one item.
Figure 2. Scree plot of the exploratory factor analysis (EFA) of activities of daily living (ADL) Questionnaire
| Variables | Components | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Dyspnea | 0.9 | ||
| Fatigue | 0.87 | ||
| Pain | 0.82 | ||
| Duration of activity | 0.79 | ||
| Difficulty | 0.75 | ||
| Safety | 0.84 | ||
| Independence | 0.78 | ||
| Value | 0.98 | ||
Final Rotated Component Matrix
The questionnaire's construct validity was assessed through Pearson correlation. All parameters of the ADL questionnaire had correlations exceeding 0.9 (P < 0.05), except for the value parameter, which ranged from 0.3 to 0.44 (P > 0.05) due to the different nature of this parameter. The convergence validity of the questionnaire with the ADL part of the IHF-QoL in 80 patients with HF, based on Pearson correlation, was 0.74 (P < 0.05).
The reliability was evaluated by two raters and 30 HF patients on two occasions, with a 2-week interval between assessments, to minimize the chance of rater recall bias. Internal consistency was calculated using Cronbach's alpha coefficient, which yielded a value of 0.98, indicating high reliability. Inter-rater reliability was measured using the intraclass correlation coefficient (ICC), with the ICC for all items being > 0.9 (Table 5). These results indicate that the questionnaire's stability over time is considered adequate.
| Parameters | ICC | CI (0.95) | SEM | Mean | SD |
|---|---|---|---|---|---|
| Value | 0.97 | 0.81 - 0.99 | 2.17 | 75.08 | 12.55 |
| Safety | 0.97 | 0.85 - 0.99 | 3.26 | 74.41 | 18.84 |
| Independence | 0.97 | 0.84 - 0.99 | 3.27 | 73.75 | 18.9 |
| Difficulty | 0.93 | 0.41 - 0.99 | 5.06 | 70.08 | 19.15 |
| Pain | 0.96 | 0.73 - 0.99 | 3.81 | 71.58 | 19.08 |
| Fatigue | 0.95 | 0.75 - 0.99 | 4.03 | 67.91 | 18.04 |
| Dyspnea | 0.96 | 0.76 - 0.99 | 3.69 | 68.75 | 18.48 |
| Duration of activity | 0.94 | 0.66 - 0.99 | 4.86 | 70.66 | 19.86 |
| Total | 0.96 | 0.78 - 0.99 | 28.77 | 576.41 | 143.86 |
Inter-Rater Reliability by ICC
4. Discussion
Heart failure is a chronic condition that significantly limits individuals' daily activities and requires them to tolerate various hindrances to their performance. Understanding their needs and limitations is crucial for implementing effective interventions to maintain their ability to perform ADL activities and live independently. This study developed an ADL questionnaire for HF patients with NYHA levels 1 - 3. A decline in ADL functions for HF patients may affect their independence. Hence, a scale to identify disruptions in ADL performance is crucial.
To develop the ADL questionnaire, an item pool was prepared using a review of ADL assessment tools, the OTPF framework, the MET table, therapeutic models, and OTPF frameworks. Based on the literature, expert panel feedback, and qualitative study, the ADL parameters were categorized into treatment models and frameworks. These parameters included value, independence, safety, difficulty, dyspnea, pain, fatigue, and duration of activity. Item extraction was performed accordingly.
Exploratory Factor Analysis suggested three factors: Value, safe independence (independence and safety), and signs and symptoms (difficulty, dyspnea, pain, fatigue, and duration of activity). The final 13 items of the questionnaire demonstrated good face and content validity. The scale showed a construct validity of 0.98 and a convergent validity of 0.73. It was also found to be reliable (Cronbach's alpha: 0.97; ICC: 0.9). The final ADL questionnaire proved to be a valid and reliable scale for assessing ADL in HF patients at NYHA levels 1-3, indicating its potential for evaluating ADL challenges.
According to the ADL questionnaire, engaging in valuable activities, safety, and independence can significantly impact the daily life of individuals with HF. Common signs and symptoms of HF include difficulty with activities, dyspnea, pain, fatigue, and the duration of activities, all of which affect an HF patient's ability to perform ADL activities.
Daily Activity Questionnaire in Heart Failure Scale is a questionnaire designed to assess the ADL of HF patients. It consists of 7 dimensions: Problems in sleep and resting periods; washing; meals; toilet use; household and related activities (chores, repairs, child care, etc.); sports and non-sport leisure time activities; occupation in training; social activities; usual forms of travel, including non-sport walking or cycling; and any other uninvestigated activities. The DAQIHF questionnaire has been proven valid and reliable, with test-retest reliability ranging from 0.82 to 0.98 and high interrater reliability. Its sensitivity to changes in peak VO2 concurrent with changes in daily energy expenditure (DEE) was high (r = 0.88, P < 0.000) (10).
The DAQIHF questionnaire is used to assess the daily energy expenditure of HF patients (10) and not only focuses on ADL activities but also includes other occupations. However, it contains many items related to physical activity and does not cover all IADL and BADL parameters (12). The large number of questions makes it difficult to thoroughly assess ADL.
Performance Measure for Activities of Daily Living-8 is a self-reported questionnaire assessing functional limitations in HF patients. It was developed using the International Classification of Functioning, Disability, and Health model and a review of other functional limitation questionnaires. The items include: Getting up and down from the floor without tools; washing the body and hair; going up a flight of stairs without a handrail; vacuuming the room; pulling and closing a heavy sliding door; getting into and out of a car; walking at the same speed as someone of the same age; and walking up a slight slope for 10 minutes. The psychometric characteristics were confirmed by 130 HF patients in Japan. Validity was investigated by comparing 37 elderly CHF patients with 37 matched controls from the general population (28). The PMADL-8 focuses on mobility and physical movements but does not cover all ADL activities. Its Cronbach’s α was 0.94 and ICC was 0.96. The validity of the hierarchical scale, as assessed by a Rasch scaling analysis in elderly Japanese CHF patients, demonstrated significant (p < 0.01) and good correlations with dyspnea (r = 0.77) and fatigue scores of the Marianna Heart Failure Questionnaire (r = 0.69), and the NYHA classification (F = 26.7), indicating convergent validity.
In PMADL-8, only specific aspects related to advanced ADL activities were explored, with hardness being the sole parameter considered. Time was not documented in this questionnaire.
The KCCQ is a valid, reliable, and responsive measure of health status and functional capacity for patients with chronic HF. It is a disease-specific measurement tool consisting of a 23-item self-administered questionnaire (15 questions). The items cover physical limitation, quality of life, total symptom (including symptom frequency and symptom burden), social limitation, symptom stability, and self-efficacy. The clinical score includes the physical limitation and total symptom domains, while the overall score encompasses the clinical score as well as the quality of life and social limitation domains. Cronbach’s alpha for the KCCQ and its subscales were 0.92, with specific values of 0.80 for independent care (2 items), 0.84 for physical limitation (4 items), 0.90 for social interference (7 items), 0.86 for symptoms (8 items), and 0.63 for self-efficacy (2 items) (8). Although the KCCQ evaluates functional capacity, it is not specifically designed for assessing ADL. The KCCQ is valid and reliable for assessing the health status of HF patients, with a primary focus on quality of life. It addresses fatigue and shortness of breath but covers only a limited range of physical activities, particularly regarding the severity of limitations.
In developing this scale using the OTPF occupational therapy reference framework, all aspects of ADL and IADL have been thoroughly addressed. The current questionnaire evaluates eight parameters (value, safety, independence, difficulty, pain, fatigue, shortness of breath, and time taken) for each item, providing a more comprehensive assessment compared to other ADL questionnaires.
4.1. Study Limitations
We have not yet examined the meaningful change in ADL Questionnaire scores, and further follow-up studies should address this aspect. While the study's sample size meets statistical standards, a larger multicenter sample should be considered to improve sample representativeness, as participants in this study may not fully represent the overall HF patient population. Additionally, patients classified as class IV in the NYHA HF category were excluded due to their substantial physical limitations.
4.2. Conclusions
Regarding the prognosis and clinical outcomes of HF patients, having a dedicated ADL measurement tool is crucial for clinicians and researchers. This ADL questionnaire can accurately assess parameters in all ADL activities and identify which parameters create limitations in each activity, enabling precise clinical evaluations in occupational therapy interventions. The ADL questionnaire for HF patients with NYHA levels 1 - 3 has demonstrated good face, content, construct, and convergence validity, making it a reliable assessment tool. This questionnaire allows researchers and clinicians to evaluate patient independence in ADL and compare HF patients before and after interventions. Future studies should focus on assessing significant changes and exploring the questionnaire's validation in different societies, including cultural adaptation and predictive validity for clinical outcomes. Additionally, future research could verify the questionnaire's validity across various patient groups. It is recommended to conduct studies using the ADL activities measurement scale as a screening and outcome measure to assess and explore the therapeutic effects of interventions and improve the validity and reliability of measuring ADL activities in individuals with HF. Further examination of the generalizability of the measures for different populations and all levels of NYHA is needed to support the evaluation of interventions and screening uses of the measures.