1. Background
Attention deficit hyperactivity disorder (ADHD) is a chronic neurodevelopmental disorder characterized by an ongoing pattern of inattention or hyperactivity and impulsivity (1). Attention deficit hyperactivity disorder is one of the most common childhood disorders and, despite typically being diagnosed in childhood, can persist into adolescence or even adulthood (2). According to the World Health Organization (WHO), it is estimated that ADHD affects around 5% of children and adolescents and 2.5% of adults globally (3). The Centers for Disease Control and Prevention (CDC) reports that boys are three times more likely to be diagnosed with ADHD compared to girls. However, numerous studies have suggested that ADHD in girls may be underdiagnosed due to its various manifestations (4, 5). While ADHD is considered a worldwide phenomenon, its prevalence varies by geographic region (6). In Iran, the prevalence of ADHD is 8.7%, with the highest rates in Tehran (7).
Children with ADHD may suffer from hyperactivity, impaired attention, and control of impulsive behaviors (8). These consequences of ADHD can significantly disrupt all aspects of life for both children and their parents. In other words, in addition to the physical, economic, and socioemotional impacts on parents, the effects on their psychological wellbeing are particularly significant, a fact emphasized by numerous studies (9-11). Parents of children with ADHD may feel depressed, frustrated, embarrassed, isolated, and disrespected because of their children's limitations. These unpleasant feelings can lead to various psychological disorders, especially Parenting stress (PS) (12, 13).
Parenting stress is a type of stress that emerges when parents' demands surpass their anticipated and available resources, causing challenges in their interactions with their children (14). Numerous studies have reported the presence of PS among parents of children with ADHD, as parents' understanding of their parenting role exceeds their resources and coping strategies (15-17). However, the severity and frequency of PS among parents of children with ADHD vary across different studies, potentially due to sociodemographic inequalities and differences in the severity of children’s ADHD symptoms (18, 19). One of the sociodemographic factors that can significantly influence the perception and regulation of PS is educational status (20, 21). In this regard, parents' characteristics, such as their health literacy (HL), must be considered as an underlying factor in the occurrence and intensity of PS among parents of children with ADHD (22), as HL is closely related to educational status (23, 24).
Health literacy is defined as individuals' ability to obtain, understand, and use health information and services to make informed decisions about their health, in order to maintain or even promote desirable health outcomes (25). Higher HL is associated with better mental health, as demonstrated by many studies (26, 27). In fact, individuals with a higher level of HL have a broader perspective on challenges, understand them better, and utilize more effective coping strategies to deal with them (28, 29). This is also true for parenting stress, as noted by Ağralı et al., who found that parents with a higher level of HL demonstrated a lower level of PS (30). Additionally, other studies have reported a relationship between better HL and lower PS among parents of children with different medical complexities (22, 31).
Despite the noted correlation between HL and PS in parents of children with various medical complexities, this correlation among parents of children with ADHD has not received sufficient attention in studies so far. In fact, despite the significant importance of ADHD and the considerable prevalence of its related PS among parents, studies that simultaneously evaluate the presence of PS and the level of HL, while considering the PS-HL correlation along with other correlated sociodemographic indicators, are limited. Furthermore, these limited studies have produced approximate, controversial, and ambiguous results (32-34).
Understanding how HL can influence PS among parents of children with ADHD can help researchers and healthcare professionals implement targeted interventions and support programs to improve the overall well-being of both parents and children. The findings of the present study can assist in improving the quality of care and providing support and resources to Iranian families with children suffering from ADHD, particularly within the ADHD-related rehabilitation process.
2. Objectives
Hence, based on the previously stated importance and scarcity of such studies, the current research aimed to determine the level of PS and HL among parents of children with ADHD, as well as to identify the correlation between PS and HL and other correlated sociodemographic indicators within this population.
3. Methods
This cross-sectional and descriptive-correlational study was conducted from March 2023 to December 2023 to determine the correlation between PS and HL among Iranian parents of children with ADHD.
3.1. Participants
The participants consisted of all parents of children under twelve years old with ADHD, whose disorder had been confirmed by medical diagnosis in their medical records. These participants were referred to psychiatric clinics or hospitalized in the psychiatric wards of Imam Hussein Hospital in Tehran, Iran. The sample size in the current study was determined based on two approaches. First, as Abidin declared, the appropriate sample size in correlational studies is at least 50 individuals (35). Additionally, according to Krejcie and Morgan's tables, the appropriate sample size for a population of around 80 individuals is at least 66 (36). Therefore, out of the initial 135 individuals, 83 met the inclusion criteria and provided consent after being informed of the research objectives. Ultimately, 70 individuals completed the entire questionnaire.
3.2. Procedures
Approval from the ethics committee of Shahid Beheshti University of Medical Sciences (SBMU) and permission from the vice-chancellor of SBMU were obtained in the initial phase. After verification by the education department of Imam Hossein Hospital, the procedure of convenience sampling from all parents of children under twelve years old with ADHD began in both the psychiatric clinics and psychiatric wards of Imam Hossein Hospital, based on the inclusion criteria of the study and adhering to ethical principles.
According to the inclusion criteria, the parents (either father or mother) in the current study must have had children under twelve years old with ADHD. The ADHD in children must have been verified by a psychiatrist (based on the medical diagnosis in their medical record). Additionally, at least one year must have elapsed since the diagnosis of ADHD in the children. Participants must not have had any acute or chronic physical, mental, or cognitive disorder that could interfere with their participation in the current study (based on the psychiatrist's opinion and their medical records). Participants were also required to be proficient in communicating in Persian. Ultimately, voluntary participation was necessary. In accordance with the exclusion criteria, participants who did not respond to more than 10% of the questionnaires were excluded from the study.
The study tools included the “Socio-Demographic Information Questionnaire (SDIQ),” “Parenting Stress Index, Fourth Edition (PSI-4),” and the “Test of Functional Health Literacy in Adults (TOFHLA).” These tools were provided to the participants along with sufficient explanations and were completed through self-reporting methods.
The "SDIQ" was the first tool used in the present study. It was designed by the authors and consisted of parents’ sociodemographic information. To appraise its validity, the method of qualitative content validity was implemented.
The next tool used in the present study was the “PSI-4.” The “PSI-4” was first designed in 1991 by Abidin to assess parenting stress in the parent-child system. The fourth edition of this questionnaire focuses on three main domains of stress: “child characteristics” (47 items), “parent characteristics” (54 items), and “situational-demographic life stress” (19 items). Altogether, the questionnaire has a total of 120 items, with 101 items using a 5-point Likert scale ranging from “strongly agree” (1) to “strongly disagree” (5). The remaining 19 items pertain to stressful events in the parents' lives over the past twelve months, each with a unique score (Table 1). A higher total score indicates a higher level of PS in participants, with a total score higher than 325 indicating a remarkably excessive level of PS (37, 38). Internal consistency was evaluated by calculating Cronbach's alpha in a group of 248 Hongkong mothers, resulting in 93%, 85%, and 91% for the child domain, parent domain, and the whole scale, respectively. The reliability of the Persian version of PSI-4 was evaluated using the test-retest method with a time interval of 10 days, resulting in 94% (39). The validated and reliable Persian version of this tool has been used by Habibpour et al. (α = 0.83) (40).
| Questions | Scores | Questions | Scores | Questions | Scores | Questions | Scores |
|---|---|---|---|---|---|---|---|
| 102 | 27 | 107 | 15 | 112 | 14 | 117 | 8 |
| 103 | 16 | 108 | 13 | 113 | 8 | 118 | 10 |
| 104 | 18 | 109 | 11 | 114 | 14 | 119 | 4 |
| 105 | 24 | 110 | 7 | 115 | 15 | 120 | 23 |
| 106 | 14 | 111 | 13 | 116 | 7 |
The “TOFHLA” was the final tool used in the current study. It was designed by Parker et al. (1995) to evaluate health literacy among adults. The “TOFHLA” consists of two sections: “reading comprehension” (50 items) and “numeracy” (17 items). The “reading comprehension” section evaluates an individual's ability to read health-related texts and has a total score of 50 (each question equals one point). The “numeracy” section pertains to the care and treatment information of individuals, with a different scoring method (Table 2), but also totaling 50 points. The overall score of the “TOFHLA” ranges from 0 to 100 and is divided into three levels: “insufficient” (below 59), “borderline” (60 - 74), and “sufficient” (75 - 100). The validity of “TOFHLA” was confirmed by the Fornell and Larcker method, with path coefficients and R-squares higher than 0.65 and 0.43, respectively. The composite reliability and Cronbach’s alpha coefficient for “TOFHLA” were higher than 0.70. Based on the test-retest method, the reliability of “TOFHLA” ranged from 78% to 90% (41). The validated and reliable Persian version of this tool has been used by Javadzade et al. (α = 0.79) (42). Furthermore, the Persian version of TOFHLA has been used in numerous Iranian studies, compiled in the study by Dadipoor et al. (α > 0.70) (43). Statistically, it is important to note that the validity of these tools has been confirmed by numerous related studies (44-47).
| Raw Score | Weighted Score | Raw Score | Weighted Score | Raw Score | Weighted Score |
|---|---|---|---|---|---|
| 0 | 0 | 6 | 18 | 12 | 36 |
| 1 | 3 | 7 | 21 | 13 | 39 |
| 2 | 5 | 8 | 24 | 14 | 42 |
| 3 | 9 | 9 | 27 | 15 | 45 |
| 4 | 12 | 10 | 30 | 16 | 48 |
| 5 | 15 | 11 | 33 | 17 | 50 |
3.3. Statistical Analysis
In the current research, descriptive statistics were utilized to calculate the mean, standard deviation, absolute frequency, and its percentage for demographic and clinical variables. Inferential statistics were implemented to examine the correlation between PS and HL using the t-test and Pearson correlation coefficient test. The correlations between sociodemographic characteristics with PS and HL were evaluated using Spearman's correlation coefficient. Ultimately, the obtained data were analyzed using SPSS version 26 software, with a test error rate and significance level set at less than 0.05.
3.4. Ethical Considerations
The current study was approved by the Research Ethics Committee of SBMU and received the code of ethics (IR.SBMU.RETECH.REC.1401.721). Accordingly, the ethical principles of voluntary participation, permission to withdraw, providing information, and confidentiality were upheld to the greatest extent during all stages of the study. It is necessary to note that written informed consent was obtained from all participants.
4. Results
4.1. Sociodemographic Characteristics and Descriptive Indices of Participants and Their Children
Among the 70 participants, most were in early adulthood (mean age 32.92 ± 6.79 years), female (87.1%), married (94.3%), housewives (68.6%), had secondary education (57.1%), and medium economic status (57.1%). The mean scores of the TOFHLA and PSI were 73.76 ± 14.02 and 287.51 ± 107.68, respectively. Children with ADHD were in the middle age of childhood (mean age 7.69 ± 1.93 years) (Table 3).
| Variables | Values |
|---|---|
| Gender | |
| Male | 9 (12.9) |
| Female | 61 (87.1) |
| Total | 70 (100.0) |
| Marital status | |
| Married | 66 (94.3) |
| Divorced | 4 (5.7) |
| Total | 70 (100.0) |
| Occupation status | |
| Employed | 21 (30.0) |
| Housewife | 48 (68.6) |
| Retired | 1 (1.4) |
| Total | 70 (100.0) |
| Educational status | |
| Primary | 9 (12.9) |
| Secondary | 40 (57.1) |
| Higher | 21 (30.0) |
| Total | 70 (100.0) |
| Economic status | |
| Poor | 25 (35.7) |
| Medium | 40 (57.1) |
| Desirable | 5 (7.2) |
| Total | 70 (100.0) |
| HL | 73.76 ± 14.02 (51 - 98) |
| PS | 287.51 ± 107.68 (108 - 489) |
| Age of parents | 32.92 ± 6.79 (23 - 51) |
| Age of children | 7.69 ± 1.93 (5 - 11) |
a Variables are expressed as No. (%) or mean ± SD (Min - Max).
4.2. Evaluating the Parenting Stress Among Parents of Children with Attention Deficit Hyperactivity Disorder
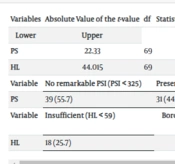
A remarkable level of PS was observed in less than half of the participants (44.3%). Moreover, based on the mean and the significance level of the PS (less than 325 and 0.05, respectively), it was concluded that although most participants did not have a remarkably excessive level of PS, the mean level of PS (287.51) among participants was still considerable and ranged from “moderate to high” according to the obtained values of lower and upper limits (261.84 and 313.19, respectively) (Table 4).
| Variables | Absolute Value of the t-value | df | Statistical Significance | Means Difference | 95% Confidence Interval of Mean Difference | |
|---|---|---|---|---|---|---|
| PS | 22.33 | 69 | 0.001 b | 287.51 | 261.84 | 313.19 |
| HL | 44.015 | 69 | 0.001 b | 73.76 | 70.41 | 77.10 |
| Variable | No remarkable PSI (PSI ˂ 325) | Presence of remarkable PSI (PSI ≥ 325) | Total | |||
| PS | 39 (55.7) | 31 (44.3) | 70 (100) | |||
| Variable | Insufficient (HL ˂ 59) | Borderline (60 - 74) | Sufficient (75 - 100) | Total | ||
| HL | 18 (25.7) | 24 (34.3) | 28 (40.0) | 70 (100) | ||
a Values are expressed as No. (%) unless otherwise indicated.
b P < 0.05.
4.3. Evaluating the Health Literacy Among Parents of Children with Attention Deficit Hyperactivity Disorder
Most of the participants demonstrated a "borderline to sufficient" level of HL (74.3%). Moreover, based on the mean score (73.76 ± 14.02) and the significance level of the TOFHLA (less than 0.05), along with the positive values of both lower and upper limits, it can be concluded that HL in parents of children with ADHD was relatively sufficient (Table 4).
4.4. The Correlation Between the Parenting Stress and the Health Literacy in Parents of Children with Attention Deficit Hyperactivity Disorder
Based on the statistical values from the Pearson correlation coefficient test (r = - 0.268, P = 0.02), the alternative hypothesis (H1) is accepted over the null hypothesis (H0). Accordingly, it can be concluded that although the correlation between PS and HL among participants was not very strong, it was still statistically significant (Table 5).
4.5. The Correlation Between Sociodemographic Characteristics and Descriptive Indicators with the PS and the HL
According to the statistical values from the Spearman's correlation coefficient test, different correlations were observed between the variables. Specifically, only the correlations between marital status and PS (r = - 0.24, P = 0.04), educational status and HL (r = 0.34, P = 0.01), and economic status and HL (r = 0.35, P = 0.01) were significant (Table 6).
| Spearman's rho | PS | HL |
|---|---|---|
| Age of parents | ||
| Correlation coefficient | 0.04 | - 0.01 |
| Sig. (2-tailed) | 0.71 | 0.94 |
| N | 70 | 70 |
| Gender | ||
| Correlation coefficient | 0.22 | - 0.09 |
| Sig. (2-tailed) | 0.06 | 0.45 |
| N | 70 | 70 |
| Marital status | ||
| Correlation coefficient | - 0.24 | 0.04 |
| Sig. (2-tailed) | 0.04 a | 0.74 |
| N | 70 | 70 |
| Educational status | ||
| Correlation coefficient | - 0.13 | 0.34 |
| Sig. (2-tailed) | 0.27 | 0.01 a |
| N | 70 | 70 |
| Occupation status | ||
| Correlation coefficient | - 0.02 | 0.01 |
| Sig. (2-tailed) | 0.86 | 0.95 |
| N | 70 | 70 |
| Economic status | ||
| Correlation coefficient | - 0.21 | 0.35 |
| Sig. (2-tailed) | 0.08 | 0.01 a |
| N | 70 | 70 |
a P < 0.05.
5. Discussion
The aim of the present study was to determine the correlation between HL and PS among Iranian parents of children with ADHD.
Regarding the first aim of the study—determining the level of PS among participants—the results indicated that, although there were no remarkably excessive levels of PS in most participants, the level was still considerable. This suggests that the complications and limitations associated with having children with ADHD have significantly affected the psychological well-being of their parents, leading to substantial psychological disorders such as PS. This finding is supported by Leitch et al., who noted that PS in parents of children with ADHD was clinically significant due to their children's individual and social limitations. They reported that parents attributed their high levels of PS to their children’s unusual behavior, unmet supportive needs, and irritating social stigma (32). Furthermore, these findings align with those of similar studies. However, differences in the frequency and severity of PS among parents of children with ADHD have been observed, which may be due to demographic and methodological variations (12, 17).
This is true for the current research as well. Most participants were female, and given that stress levels are generally higher in females compared to males (44-46), the observed severity of PS is understandable. Additionally, many participants had secondary education, poor to medium economic status, and were housewives. Thus, the considerable level of PS observed can be partly attributed to higher stress linked with lower educational status (47), higher stress associated with lower economic status (48), and higher stress correlated with unemployment (49). Finally, as most participants were in early adulthood (around 33 years old), the reported PS levels are consistent with the fact that individuals aged 18 - 34 often experience the highest levels of stress (50).
In relation to the second aim of the present study—determining the level of HL among Iranian parents of children with ADHD—the results indicated relatively sufficient levels of HL among most participants. Although most participants had "sufficient" levels of HL, there was also a considerable number with "borderline" levels of HL. This finding contrasts with the study by de Moura et al., which reported that ADHD-related symptoms in a family member are associated with lower HL levels in that family (51). However, Davidson et al. reported results somewhat consistent with the present study, noting that the level of HL was above the medium range among most parents of children with ADHD (34).
The variability in results is not limited to these studies; other similar research has also reported various levels of HL among parents of children with ADHD (52-54). This suggests that the contradictory findings regarding HL levels among parents of ADHD children may be related to differences in demographic and methodological characteristics of the studies. Given the well-established fact that "higher educational status is associated with higher HL" (23, 55), the relatively sufficient HL levels observed in this study might be attributed to the significant proportion of participants with secondary or higher education. Additionally, since "HL tends to be higher among younger individuals," the relatively sufficient HL in this study may also be due to the early-adulthood age range of most participants (56-58).
Regarding the third aim of the study, there was a meaningful but not very strong inverse correlation between participants' PS and HL. This implies that as participants' HL increased, their PS decreased, and vice versa. This finding is supported by Michou et al., who reported that "low levels of HL are significantly correlated with high levels of stress" (59). Additionally, Dekkers et al. found a meaningful association between parents' knowledge and HL and their experienced PS due to their children's ADHD-related complications, stating that "higher knowledge and HL correlate with lower experienced PS" (60). While other studies have emphasized the existence of an inverse correlation between HL and PS among parents of children with other chronic disorders, the results are consistent with those of the current study (61-64).
Consistent with the last aim of the study, there were positive, though not very strong, correlations between PS and the age and gender of parents. Specifically, female and older individuals demonstrated higher levels of PS. Generally, physiological and psychological differences between genders are associated with higher stress levels among women (65). Regarding age, findings vary: Some studies suggest that younger individuals are more vulnerable to stress due to psychosocial issues (50, 66), while others report that the physiological vulnerabilities of old age lead to higher stress levels (67, 68). Nevertheless, the results of the studies by Narkunam et al. and Lee and Kim align with the findings of the present study (69, 70).
Conversely, weak but inverse correlations were found between PS and marital status, educational level, occupation, and economic status. Individuals who were married, had higher educational levels, better economic status, and employment experienced lower levels of PS. These conditions contribute to a more favorable lifestyle, which is associated with reduced stress levels (71-74). The results were consistent with numerous similar studies (32, 75, 76).
Regarding HL, various but weak correlations were observed. Younger parents, males, married individuals, those with higher educational levels, better economic status, and those who were employed reported higher levels of HL. Most of these conditions are contextual factors that enhance knowledge and awareness, leading to higher HL levels (77-79). These findings are consistent with the results of several other studies (34, 51).
5.1. Limitations
The generalizability of the findings may be limited due to several factors: The small sample size, the exclusive focus on participants from Tehran, potential diversity among parent-child dyads (such as varying sociodemographic and diagnostic characteristics), and the restriction to government medical centers, which may limit the sample to participants from middle to low socioeconomic backgrounds. Additionally, the study's methodology presents limitations, including the use of convenience sampling and self-report tools, which may introduce bias. These limitations should be considered when interpreting the findings and applying them to other populations or settings.
5.2. Implications
Assessing levels of HL and PS among Iranian parents of children with ADHD can help identify those who may need additional comprehensive support. Healthcare professionals can evaluate HL and PS during routine visits and provide appropriate resources based on the identified needs in both clinical and community settings. Addressing factors that influence HL and PS levels can improve parent-child relationships and overall quality of life. Interventions designed to enhance HL and reduce PS can lead to better outcomes for both Iranian parents and their children with ADHD. Educational programs focused on PS management and HL improvement can benefit these parents. Providing tools to enhance coping strategies and resilience can also help reduce PS and improve overall well-being. Collaborative care models involving healthcare providers, mental health professionals, and community resources can address the complex needs of parents of children with ADHD. Therefore, implementing such models within the Iranian sociocultural context, with a focus on providing comprehensive services, can lead to better outcomes for the entire family system.
5.3. Conclusions
According to the results of the current study, the level of HL among Iranian parents of children with ADHD was "relatively sufficient," while their PS was "considerable." Additionally, the correlation between PS and HL among participants was significant but not strongly inverse. It is important to note that the "frequency," "severity," and "correlation" of these variables were influenced by various demographic factors among participants. Therefore, further studies are needed to investigate the factors affecting HL and PS levels in this group of parents to enhance their parent-child relationships and improve their overall quality of life.