1. Background
Total hip replacement involves removing the damaged hip joint and replacing it with an artificial prosthesis, consisting of both femoral and acetabular components. It is estimated that approximately 170,000 individuals in the United States and 300,000 people worldwide undergo this procedure each year (1).
Currently, posterior hip replacement is the most commonly performed procedure in the United States and possibly worldwide (2). In this method, the gluteus maximus, short external rotator muscles, and the entire capsule are divided to access the hip joint (3), and at the end of the operation, the muscles are sutured to increase joint stability and reduce the risk of dislocation (4). The posterior approach is popular due to the relative ease of the operation (5), though there is a risk of sciatic nerve injury (6) and post-operative dislocation (7). However, studies suggest there is no increased risk of dislocation when the capsule is properly sutured or when posterior soft tissue repair is enhanced (2).
In contrast, the anterior hip replacement approach allows access and implantation without cutting through the thigh muscles, using a path between the tensor fascia latae and rectus femoris (8). Recently, there has been growing interest in the anterior approach to hip replacement (9). The advantages of this method include less muscle damage, faster recovery following surgery, the possibility of early activity of the affected limb, a lower dislocation rate, and no need for precautions to prevent dislocation after surgery (3). However, its disadvantages include the possibility of femur fracture, increased blood loss during surgery (10), technical difficulty of the procedure and the need for specialized equipment, potential damage to the tensor fasciae latae and rectus femoris (9), and neuropraxia of the lateral femoral cutaneous nerve (7), which can cause numbness and discomfort at the incision site (5). As described, each of the total hip arthroplasty approaches has its own advantages and disadvantages, and it remains unclear which approach is more effective in achieving better functional outcomes (11). Surgeons continue to debate the best surgical method for total hip replacement and the superiority of one approach over the other (6, 12). While some studies suggest short-term benefits of the anterior approach over the posterior approach (13-15), others have found no significant long-term advantages (16-19). Additionally, research indicates that muscle damage can occur in both approaches, with the tensor fascia latae and rectus femoris being more affected in the anterior approach (20). Critics of minimally invasive techniques argue that reported improvements may result from unrelated factors such as aggressive physical therapy, comprehensive pain management protocols, or biased selection of healthier, more motivated patients (15).
The most affected structures in hip replacement surgery are the joint mechanoreceptors. Damage to these mechanoreceptors results in proprioceptive impairment, leading to the transmission of abnormal signals to the brain regarding joint position and movement. One of the key abilities impacted by proprioceptive abnormalities is balance, and disturbances in balance may persist after surgery, increasing the risk of falls, particularly during the first-year post-surgery (21). Additionally, while a person’s ability to perform daily activities generally improves following hip replacement, certain tasks, such as climbing stairs and rising from a chair, may remain challenging (22). Reduced independence in daily activities among individuals undergoing hip replacement can stem from diminished physical performance and a fear of engaging in these activities due to a lack of confidence in the operated limb. This hesitancy may extend to activities like stair navigation or leaving the home, ultimately increasing a patient's dependence over time (23).
Although some studies suggest better physical performance in the early postoperative period for anterior hip replacement compared to posterior hip replacement (3), this does not necessarily equate to improved overall physical activity in the anterior group (24, 25). Contrary to the hypothesis that individuals who undergo anterior hip replacement may have better balance due to reduced muscle damage during surgery compared to the posterior approach, previous research has observed better balance in the posterior group (21). This finding highlights the need for further research on this topic. To date, no studies have compared biomechanical indicators of balance between anterior and posterior hip replacements.
2. Objectives
Therefore, the aim of this study was to compare the two approaches—anterior and posterior hip replacement—in terms of biomechanical performance, functional indicators, and quality of life.
3. Methods
3.1. Participants
In this cross-sectional observational study, 22 participants who had undergone anterior hip replacement, 20 who had undergone posterior hip replacement, and 20 healthy individuals were included. The inclusion criteria for the surgery groups were: Age between 50 to 65 years, undergoing hip replacement for the first time, unilateral surgery, a minimum of 6 months and a maximum of 12 months post-surgery, ability to understand instructions and absence of cognitive impairment (Mini-mental Status Examination (MMSE) score of 24 - 30) (26), absence of neurological or orthopedic disorders, no use of balance-disrupting medications during the evaluation period, ability to walk and stand without assistive devices, and no strong dependence on a wheelchair. Exclusion criteria for the surgery groups included any damage to the operated hip joint requiring re-surgery and complications such as embolism that could interfere with the recovery process.
For the healthy group, the inclusion criteria were: Age between 50 to 65 years, absence of neurological or orthopedic disorders affecting balance, no use of balance-disrupting medications during the study period, ability to walk and stand without aids, and no history of lower limb surgery within the past year.
All patients who underwent hip replacement surgery were treated at Akhtar Hospital. The surgery group patients were referred for the study by an orthopedic hip surgeon, and the primary researcher (first author) selected the patients based on the inclusion/exclusion criteria. Participants in the healthy control group were recruited from the School of Rehabilitation at Shahid Beheshti University of Medical Sciences. This study received ethical approval from the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1401.610), and all participants provided written informed consent for participation in the study.
3.2. Measurement Tools
3.2.1. Force Plate
To measure balance, a Bertec force plate (manufactured in the United States) was utilized, with dimensions of 40 × 60 cm and a sampling frequency of 1000 Hz, located in the biomechanics laboratory of the School of Rehabilitation at Shahid Beheshti University of Medical Sciences. The center of pressure (COP) variables, including displacement, velocity, and phase transition in the anterior-posterior and medial-lateral directions, were extracted for analysis (27).
3.2.2. Timed Up and Go Test (TUG)
The timed up and go test is used to assess functional balance and mobility. In this test, the time taken for an individual to rise from a chair with armrests, walk a distance of three meters at a self-selected speed without losing balance, turn around, and return to sit on the chair is measured. The height of the chair was adjusted to ensure a 90-degree flexion at the knee joint with the soles of the feet flat on the ground while seated. The time to complete the test was recorded in seconds using a stopwatch, and the average of three repetitions was calculated as the final TUG test score. This test has demonstrated high validity and reliability (ICC = 0.95, r = 0.77) as well as good sensitivity (28, 29).
3.2.3. Barthel Index
The Barthel Index was used to measure the functional independence of the participants. It consists of 10 items that assess a person's ability to independently perform daily activities such as bowel and bladder control, grooming, toileting, bathing, feeding, chair transfers, dressing, ambulation, and stair climbing. The scores range from 0 to 100, with higher scores indicating greater independence in daily life activities. The validity and reliability of the Barthel Index in Iran were established by Oveisgharan et al. at the Isfahan Cardiovascular Research Center (ICRC) (30). To evaluate the participants' level of independence in performing daily tasks, the Persian version of the modified Barthel Index was used. The examiner assessed self-care activities through direct observation or interviews, rating the activities based on the level of assistance required to compensate for any inability to perform them (31).
3.2.4. Canadian Occupational Performance Measure (COPM)
The Canadian Occupational Performance Measure was used to assess participants' occupational performance. The COPM is administered through a semi-structured interview and evaluates performance and satisfaction in three occupational areas: Self-care, leisure, and productivity. During the interview, participants rate their self-perceived performance and satisfaction with performance in each occupation on a scale from 1 to 10. The total scores are then divided by the number of activities, providing an average score for both performance and satisfaction. Higher scores indicate better occupational performance and higher satisfaction with performance (32). The COPM has been translated into Persian by Dehghan et al., with demonstrated validity and reliability (33).
3.2.5. Short Form-36 Health Survey (SF-36)
The SF-36 questionnaire is used to assess health status and health-related quality of life in both healthy and patient populations. The validity and reliability of its Persian version have been confirmed in Iran by Montazeri et al. (34). The SF-36 includes eight health domains: Physical functioning, role limitations due to physical health problems, bodily pain, role limitations due to emotional problems, psychological distress and well-being, social functioning, vitality (energy and fatigue), and general health perceptions. Responses are provided using various rating scales, such as a five-point Likert scale from excellent to poor, or yes/no formats, depending on the question. Scores for each domain range from 0 to 100, with higher scores reflecting better health status.
3.3. Procedure
During the study, the researcher (first author) provided a detailed explanation of the study's purpose and methodology to all participants. Participants were screened based on the entry criteria, and those who met the criteria and were willing to participate were asked to sign a written consent form. All participants from the three groups were then instructed to visit the biomechanics laboratory at the School of Rehabilitation, Shahid Beheshti University of Medical Sciences, where their static balance was assessed using a force plate. Participants were asked to stand barefoot on the force plate in two trials: (1) standing on both legs with eyes open, and (2) standing on both legs with eyes closed, with three repetitions for each trial. The center of pressure variables were extracted using MATLAB software. Subsequently, clinical parameters, including functional balance, functional independence, participants' self-perceived performance, satisfaction with performance, and quality of life, were evaluated.
For the assessment of COP-related variables and functional balance, the presence of the healthy control group was required to compare the performance of the two surgical groups. However, other clinical tests were performed only on the two groups who had undergone anterior and posterior hip replacements. The average of three repetitions was used for analysis in both force plate and TUG test conditions.
3.4. Data Analysis
In the present study, descriptive statistics, including mean and standard deviation, were used for quantitative variables. The Kolmogorov-Smirnov test was applied to assess the normality of the data distribution. If the data were normally distributed, a one-way analysis of variance (ANOVA) was used to compare the three groups, and an independent t-test was used to compare pairs of two groups. For non-normally distributed data, the Kruskal-Wallis test was applied for comparisons among three groups, and the Mann-Whitney test was used for comparing pairs of two groups. Data analysis was conducted using SPSS-18 software, with a significance level set at 0.05.
4. Results
In this study, 62 participants were divided into three groups: Twenty-two in the anterior hip replacement group (11 women, 11 men), 20 in the posterior hip replacement group (12 women, 8 men), and 20 in the healthy control group with no history of surgery (9 women, 11 men). There were no significant differences in any demographic variables among the three groups (P ˃ 0.05) (Table 1), except for the time since surgery (P = 0.02). Tables 2 and 3 present the mean, standard deviation, and group comparisons for the measured outcomes.
| Variables | Control | Anterior Hip Replacement | Posterior Hip Replacement | P-Value |
|---|---|---|---|---|
| Age (y) | 54.95 ± 3.60 | 58.22 ± 5.38 | 56.10 ± 4.73 | 0.76 |
| Time since surgery (mo) | - | 9.63 ± 1.89 | 8.30 ± 1.71 | 0.02 |
| Height (cm) | 166.25 ± 9.68 | 166.09 ± 9/97 | 164.95 ± 8.86 | 0.89 |
| Weight (kg) | 79.40 ± 21.61 | 72.18 ± 12.20 | 71.15 ± 11.25 | 0.19 |
| Body Mass Index | 28.54 ± 7.24 | 26.07 ± 3.07 | 26.15 ± 3.65 | 0.20 |
| Lower limb length on the operated side (cm) | 83.40 ± 4.42 | 83.77 ± 5.25 | 83.30 ± 4.37 | 0.94 |
| Foot length on the operated side(cm) | 24.55 ± 1.82 | 25.00 ± 1.63 | 24.75 ± 1.74 | 0.70 |
Demographic Data of Participants in Three Groups a
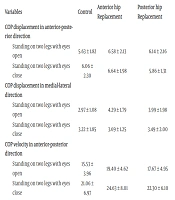
| Variables | Control | Anterior Hip Replacement | Posterior Hip Replacement | P-Value (Different Among Three Groups) |
|---|---|---|---|---|
| COP displacement in anterior-posterior direction | ||||
| Standing on two legs with eyes open | 5.63 ± 1.82 | 6.58 ± 2.13 | 6.14 ± 2.16 | 0.39 |
| Standing on two legs with eyes close | 6.06 ± 2.30 | 6.64 ± 1.98 | 5.86 ± 1.31 | 0.21 |
| COP displacement in medial-lateral direction | ||||
| Standing on two legs with eyes open | 2.97 ± 1.08 | 4.29 ± 1.79 | 3.99 ± 1.98 | 0.03 b |
| Standing on two legs with eyes close | 3.22 ± 1.85 | 3.69 ± 1.25 | 3.49 ± 2.00 | 0.21 |
| COP velocity in anterior-posterior direction | ||||
| Standing on two legs with eyes open | 15.53 ± 3.96 | 19.40 ± 4.62 | 17.67 ± 4.95 | 0.02 b |
| Standing on two legs with eyes close | 21.06 ± 6.97 | 24.63 ± 8.01 | 22.30 ± 6.10 | 0.42 |
| COP velocity in medial-lateral direction | ||||
| Standing on two legs with eyes open | 9.92 ± 3.25 | 13.98 ± 3.76 | 14.06 ± 8.03 | 0.25 |
| Standing on two legs with eyes close | 10.94 ± 5.09 | 14.37 ± 4.50 | 14.18 ± 9.05 | 0.29 |
| Phase transition of COP in anterior-posterior direction | ||||
| Standing on two legs with eyes open | 11.91 ± 3.19 | 6.58 ± 2.13 | 13.68 ± 4.15 | 0.38 |
| Standing on two legs with eyes close | 15.53 ± 5.26 | 6.64 ± 1.98 | 16.84 ± 4.69 | 0.59 |
| Phase transition of COP in medial-lateral direction | ||||
| Standing on two legs with eyes open | 7.58 ± 2.52 | 12.12 ± 1.79 | 4.39 ± 6.01 | 0.29 |
| Standing on two legs with eyes close | 9.13 ± 6.80 | 11.01 ± 1.25 | 3.57 ± 6.83 | 0.20 |
The Mean, Standard Deviation and P-Value Among Groups for Center of Pressure Variables a
| Variables | Control | Anterior Hip Replacement | Posterior Hip Replacement | P-Value |
|---|---|---|---|---|
| Functional Balance | 10.59 ± 1.99 | 11.66 ± 2.35 | 11.10 ± 1.89 | 0.31 |
| Functional Independence | - | 99.09 ± 2.50 | 99.75 ± 1.11 | 0.33 |
| Client's Performance | - | 6.77 ± 3.06 | 8.10 ± 2.63 | 0.23 |
| Client's Satisfaction | - | 7.09 ± 3.00 | 8.15 ± 5.56 | 0.31 |
| Quality of Life | - | 80.50 ± 5.67 | 83.25 ± 5.96 | 0.21 |
The Mean, Standard Deviation, and P-Value Among Groups for Clinical Variables a
The normality test results indicated that most of the COP-related indicators and clinical variables—including functional balance, functional independence, performance and satisfaction of performance, and quality of life—did not follow a normal distribution in one, two, or all three groups.
There was a significant difference among the three groups for two COP variables: COP displacement in the medial-lateral direction (P = 0.03) and COP velocity in the anterior-posterior direction (P = 0.02) during two-leg standing with eyes open. Pairwise comparisons revealed a significant increase in both variables in the anterior replacement group compared to the healthy control group. No significant differences were found among the three groups for the other COP variables. Additionally, there was no significant difference between the anterior and posterior hip replacement groups or between the posterior replacement group and the control group for any COP indices.
Regarding the clinical variables, the statistical analysis showed no significant differences between the anterior and posterior replacement groups (Table 3). Furthermore, for the TUG test, there was no significant difference between the two replacement groups and the healthy control group.
5. Discussion
In the conducted studies, no clear superiority of hip joint replacement using the anterior method over the posterior one has been demonstrated. Unlike previous studies, which primarily compared the two surgical methods in terms of hospital discharge time, pain, and bleeding rate, this study focused on comparing these methods in terms of biomechanical indicators of the COP, clinical variables, and quality of life. The results of our study showed no significant differences between the anterior and posterior replacement groups concerning COP indicators and clinical variables. Therefore, the present study does not support the hypothesis that there is a significant difference between the two surgery groups in these variables.
There was no significant difference between the anterior and posterior hip replacement groups in clinical variables, including functional balance, functional independence, self-perception of performance and satisfaction, and quality of life. Martusiewicz et al., comparing the performance of the two hip replacement groups during the first six weeks after surgery, reported that the anterior replacement group discarded assistive devices 8 days earlier, left their homes 3 days earlier, and resumed driving 5 days earlier than the posterior group (7). Maldonado et al. suggested that after a 2-year follow-up, the anterior replacement group showed a higher quality of life compared to the posterior group (35), which contrasts with the findings of the present study. The discrepancy may be attributed to the fact that the evaluation in the Maldonado et al. study was conducted less than six months post-surgery, whereas the evaluation in our study was conducted at least six months post-surgery. Additionally, the follow-up period for the posterior group was significantly longer than for the anterior group in Maldonado et al.'s study (35).
On the other hand, the findings of Barrett et al. (36) and Yuasa et al. (37) are consistent with the present study. They compared the performance and quality of life of the anterior and posterior hip replacement groups five years post-surgery and observed favorable outcomes in both groups, with no significant differences. It seems that any initial differences between the anterior and posterior replacements may diminish six months after surgery, as rehabilitation and muscle strength improve, which directly impacts performance and quality of life, and both approaches ultimately achieve good results (24, 38).
According to the results, there was no significant difference between the anterior and posterior replacement groups in all variables related to COP. In a study by Pan et al., which aimed to investigate differences in postoperative gait, limb balance, and hip motor capacity one month after surgery between two hip replacement groups, it was reported that the anterior replacement group performed significantly better than the posterior group in terms of stride length, stride frequency, single-leg support time, and plantar pressure difference. By the third month after surgery, the anterior group continued to outperform the posterior group in stride frequency, single-leg support time, and plantar pressure difference. However, six months post-surgery, the anterior group only performed better than the posterior group in plantar pressure difference, with no significant differences in other parameters. Additionally, the anterior group showed better performance in the 2-minute walking and standing-walking timing tests during the first and third months post-surgery (39).
In a review by Labanca et al., they found no difference between the anterior and posterior replacement approaches in single-limb standing balance two months after surgery (21), which is consistent with the findings of the present study. It appears that six months after hip replacement surgery, due to routine rehabilitation and the individual's engagement in daily life activities, the strength and proprioception of the muscles damaged during surgery (24) have improved, leading to a closer balance and performance level between the two groups.
When compared to the healthy control group, the anterior replacement group exhibited significantly higher COP displacement in the medial-lateral direction and COP velocity in the anterior-posterior direction during two-leg standing with eyes open. This indicates that the anterior group expended more energy to maintain static balance compared to the control group. However, none of the COP variables were significantly different in the posterior replacement group compared to the control group.
In the anterior approach, the use of surgical tools may cause excessive stretching of hip muscles, particularly the tensor fasciae latae and sartorius, likely contributing to the greater difference observed between the anterior group and the control group. These muscles contain more neuromuscular spindles than the external rotators that are split during the posterior approach, and they play a significant role in movement control (40). A previous study reported that individuals with anterior hip replacements exhibited higher average COP displacement and velocity compared to healthy controls, while those with posterior hip replacements showed no significant differences from the controls (40).
We need to acknowledge several limitations in this study. First, the multiple inclusion criteria limited the sample size, restricting the number of participants we could examine. Second, all patients in the study were operated on by the same surgical team in the same hospital, which may reduce the generalizability of the results to other surgeons or clinical environments. Third, individuals with lower functional levels, those whose surgeries did not result in favorable outcomes, or those who experienced multiple complications during surgery were not included in the study. This omission could influence the significance of the results and findings.
It is recommended that future research follow up with patients at two different time periods—less than six months and more than six months after surgery—to determine whether performance differences between the two groups persist. Additionally, since the Barthel index does not capture subtle differences in daily activity performance, it would be beneficial to use a scale capable of detecting these minor performance variations in future studies. Lastly, future research should include cases of hip replacement surgery accompanied by complications such as nerve damage, as well as cases requiring additional surgeries. This will allow for a comparison of individuals with a broader range of functional levels.
5.1. Conclusions
The results of the present study did not reveal significant differences between the two groups undergoing hip joint replacement using the anterior and posterior methods in terms of biomechanical and clinical indicators and quality of life six months after surgery. Therefore, the choice of surgical method can be based on the patient's specific condition and the surgeon’s expertise in the particular approach.