1. Background
Knee osteoarthritis (KOA) is a prevalent and disabling musculoskeletal condition, particularly affecting older adults. The condition is characterized by symptoms such as knee joint pain, stiffness, and functional limitations, all of which severely diminish quality of life and can lead to disability. This condition imposes a significant burden on healthcare systems globally, highlighting the need for effective symptom management and treatment strategies (1, 2).
Current treatment modalities for KOA include physiotherapy, pharmacological interventions, injectables, and surgery, with conservative therapies being particularly favored for their minimal invasiveness, especially in the non-severe stages of KOA. Physiotherapy encompasses a variety of techniques, including electrotherapy, exercise therapy, and manual therapy (3, 4). Among these, manual therapy is widely used and has been shown to reduce pain and improve joint range of motion (5, 6).
Instrument-assisted soft tissue mobilization (IASTM), a relatively new and increasingly popular manual therapy technique, utilizes specialized tools to mobilize soft tissues. Research suggests that IASTM can be effective in reducing pain, enhancing range of motion, and improving strength (7-12). The proposed mechanisms by which IASTM operates include breaking down cross-links within tissues, decreasing tissue viscosity, increasing blood flow, and positively affecting inflammation, pain receptors, and soft tissue release. All of these contribute to greater joint mobility, pain relief, and increased functional capacity (7, 8, 10, 13, 14).
When evaluating KOA treatments, it is essential to consider both localized effects and broader impacts on functional abilities and overall quality of life. Although a few studies have explored the effectiveness of IASTM in reducing pain and enhancing range of motion in individuals with knee pain (15-17), its impact on overall function and quality of life remains underexplored. Objective functional tests such as the 6-minute walking test (6MWT) and the timed up and go test (TUG) offer measurable outcomes of physical performance and mobility (18, 19). Additionally, subjective assessments of quality of life, using instruments like the 36-item short form health survey (SF-36) and the Lequesne Algofunctional Index (LAI), are critical in understanding the broader effects of KOA on daily activities, social interactions, and emotional well-being (20, 21).
2. Objectives
Despite the growing interest in IASTM, there is a significant gap in the literature regarding its specific effects on functional tests and quality of life measures in patients with KOA. This study aims to investigate the impact of a two-week IASTM intervention on these outcomes in KOA patients. By addressing this gap, we hope to contribute valuable insights into the potential benefits of IASTM as an adjunctive therapy for improving functional outcomes and enhancing quality of life in KOA patients.
3. Methods
3.1. Study Design
This study utilized a parallel, randomized, controlled, double-blind clinical trial design to evaluate the effects of IASTM compared to a sham intervention at two time points: (1) before and (2) after treatment. The dependent variables included functional measures (6MWT and TUG) and quality of life (SF-36 and LAI questionnaire) in KOA patients.
3.2. Participants
Initially, 33 participants were enrolled in the study, but three were excluded due to personal reasons, leaving 30 individuals diagnosed with unilateral KOA who completed all stages. The sample size was determined using G*Power (22) based on pilot data, with an alpha of 0.05, a beta of 0.2, and a medium effect size of 0.28. This calculation indicated a required sample size of 28 participants, and additional participants were included to account for potential dropouts.
Inclusion criteria were as follows: Age over 40 years, ability to walk unassisted, moderate KOA (Kellgren-Lawrence grades 2 and 3), and a BMI between 18.5 and 29.9. Exclusion criteria included a history of orthopedic, neurological, or rheumatologic conditions affecting the lower limb or lower back, current low back pain, a history of intra-articular injections in the past six months, severe lower-limb deformity, candidacy for total knee arthroplasty, a leg length discrepancy greater than 1.5 cm, or regular use of NSAIDs or other painkillers in the two weeks prior to treatment.
Randomization was performed using four blocks, with two assigned to the treatment group and two to the sham group. An individual not involved in the research team conducted the randomization process. Code 1 was used for the treatment group and code 0 for the sham group, with these codes placed in sealed envelopes. The study was double-blind, ensuring that both participants and the assessor were unaware of group assignments. To prevent interaction between participants, clinic visits were scheduled on different days. In the IASTM group, therapeutic direction and adequate force were applied, while in the sham group, only superficial touches were performed. The assessor also remained blinded to the participants' group assignments. All participants provided written informed consent approved by the Tarbiat Modares University Ethics Committee. Additionally, the study was registered with the Iranian Registry of Clinical Trials under the code IRCT20201128049511N3.
3.3. Interventions
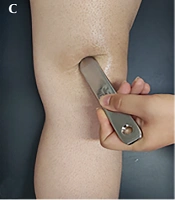
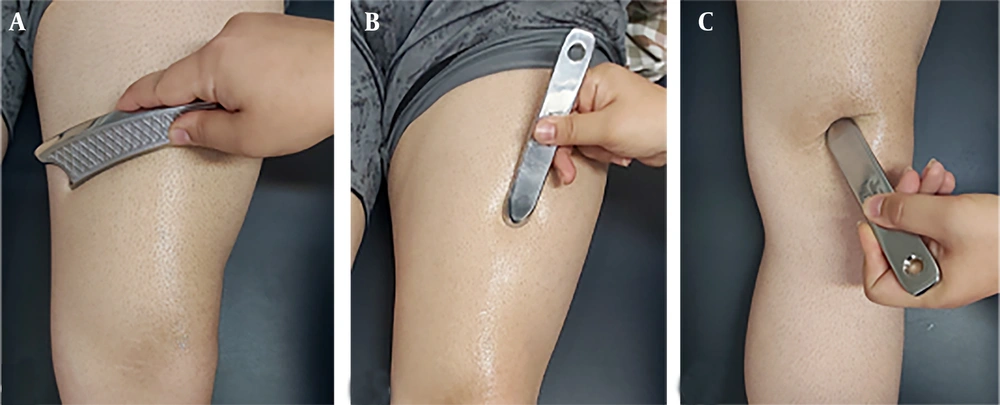
Following an initial assessment at the Research and Treatment Center for Movement Disorders at Tarbiat Modares University, participants returned the next day to receive IASTM administered by experienced physiotherapists. The treatment involved techniques such as sweeping, fanning, brushing, and framing, following the HawkGrips method using specific instruments (HGpro Multi-Tool from HawkGrips, USA, and three instruments—IS-3, IS-4, and IS-22—from MyoRelease, Iran). These techniques were applied for 60 to 90 seconds per area, targeting tissue irregularities and sensitive points in peri-articular muscles (quadriceps, hamstrings, gastrocnemius, tibialis anterior). Sweeping and fanning utilized the broader edge of the instrument, with sweeping performed in parallel and fanning executed in an arc motion (Figure 1A). Brushing involved using a smaller edge of the instrument, applied parallel to the tissue (Figure 1B). Framing focused on small strokes around the patella to enhance patellar mobility (Figure 1C) (23).
After IASTM, participants engaged in stretching and strengthening exercises, as it is recommended to combine IASTM with exercise (24). These exercises targeted the quadriceps, hamstrings, gastrocnemius, and tibialis anterior muscles (25, 26). The entire treatment was administered in four sessions over two weeks. The number of sessions was chosen based on literature demonstrating the immediate and short-term effects of IASTM (27-31). A reassessment session occurred 48 hours after the final session for the 6MWT, TUG, and LAI questionnaire. The SF-36 questionnaire was administered 2 weeks later to ensure a 4-week gap between the initial and follow-up assessments, as required by the questionnaire’s wording that refers to the previous 4 weeks. The sham group underwent a similar procedure without therapeutic IASTM movements, using instruments lightly applied to the skin.
3.4. Outcome Measures
Participants underwent comprehensive assessments before and after the intervention to evaluate the effects of IASTM on KOA patients. Functional tests included the 6MWT and TUG test. The 6MWT measures the distance walked on a flat, hard surface within six minutes, providing insights into aerobic capacity and endurance, which are crucial for assessing mobility in KOA patients. Participants walked in a 10-meter corridor with cones marking the turning points; a chair was placed in the middle of the corridor for rest if needed. However, all participants completed the 6-minute walk without needing to sit. The TUG test assesses lower extremity strength, balance, and functional mobility by timing participants as they stand up from a chair, walk three meters, turn around, walk back to the chair, and sit down again (18, 19).
In addition to functional tests, subjective quality of life questionnaires were administered. The SF-36 was used to assess various aspects of health-related quality of life, including physical functioning, role limitations due to physical problems, role limitations due to emotional problems, energy/vitality, mental health, social functioning, pain, and general health. It consists of 36 items, with each category scored out of 100, where higher scores indicate better quality of life (32). The LAI questionnaire specifically evaluated pain levels, maximum walking distance, and the impact of KOA on daily activities. The LAI consists of 24 questions, with a maximum score of 14 indicating the most severe condition of KOA (33). Both questionnaires were translated into Persian and have been shown to be reliable and valid (32, 33).
3.5. Data Analysis
The Shapiro-Wilk test was conducted to check the normal distribution of the data. Since all data followed a normal distribution, an independent t-test was performed at baseline to identify any initial differences between the two groups. A mixed ANOVA, with one within-subject factor (before and after treatment) and one between-subject factor (treatment and sham group), was used to assess the effect of the treatment. The alpha level was set at 0.05, and partial eta squared values of 0.01, 0.06, and 0.138 were used to indicate small, medium, and large effect sizes, respectively (34).
4. Results
All 30 participants completed the entire procedure. Demographic data and descriptive results of all variables are presented in Tables 1, and 2, respectively.
| Variables | IASTM Group (N = 15) | Placebo Group (N = 15) | P-Value |
|---|---|---|---|
| Sex | - | ||
| Female | 13 | 12 | |
| Male | 2 | 3 | |
| Age, (y) | 57.73 ± 8.54 | 58.27 ± 7.36 | 0.277 |
| Body Mass Index, kg/m2 | 27.46 ± 2.95 | 27.59 ± 2.82 | 0.856 |
Abbreviation: IASTM, instrument-assisted soft tissue mobilization.
| Variables | IASTM Group | Sham Group | ||
|---|---|---|---|---|
| Before | After | Before | After | |
| 6 MWT, (m) | 357.27 ± 52.22 (328.34 - 386.19) | 400.53 ± 54.85 (370.15 - 430.91) | 353.40 ± 68.58 (315.42 - 391.38) | 371.80 ± 60.36 (338.37 - 405.23) |
| TUG, (s) | 8.66 ± 1.01 (8.06 - 9.22) | 7.97 ± 1.06 (7.38 - 8.56) | 8.71 ± 1.25 (8.01 - 9.40) | 8.51 ± 0.95 (7.98 - 9.04) |
| Total LAI score | 9.00 ± 2.54 (7.58 - 10.41) | 5.86 ± 1.89 (4.81 - 6.91) | 7.66 ± 3.55 (5.69 - 9.63) | 6.10 ± 3.21 (4.31 - 7.88) |
| Physical functioning | 46.66 ± 18.28 (36.53 - 56.79) | 49.66 ± 17.87 (39.76 - 59.56) | 51.00 ± 19.83 (40.01 - 61.98) | 53.66 ± 19.03 (43.12 - 64.20) |
| Role limitations (physical) | 55.00 ± 25.24 (41.02 - 68.97) | 62.08 ± 17.43 (52.42 - 71.73) | 54.16 ± 17.62 (44.40 - 63.92) | 62.08 ± 16.10 (53.16 - 71.00) |
| Role limitations (emotional) | 59.44 ± 20.86 (47.89 - 70.99) | 68.33 ± 19.21 (57.69 - 78.97) | 72.77 ± 14.24 (64.88 - 80.66) | 68.88 ± 15.89 (60.08 - 77.69) |
| Energy/vitality | 40.13 ± 17.26 (30.58 - 49.69) | 47.08 ± 17.17 (37.57 - 56.59) | 47.91 ± 19.14 (37.31 - 58.51) | 51.66 ± 16.78 (42.37 - 60.96) |
| Mental health | 54.33 ± 19.16 (43.71 - 64.94) | 57.33 ± 15.90 (48.52 - 66.14) | 60.08 ± 17.93 (50.15 - 70.01) | 62.33 ± 13.21 (55.01 - 69.64) |
| Social functioning | 74.16 ± 12.90 (67.01 - 81.31) | 76.00 ± 9.99 (70.46 - 81.53) | 68.33 ± 16.94 (58.94 - 77.71) | 69.16 ± 15.57 (60.54 - 77.79) |
| Pain | 45.33 ± 19.95 (34.28 - 56.38) | 58.66 ± 15.75 (49.94 - 67.38) | 53.33 ± 16.08 (44.42 - 62.23) | 64.33 ± 17.12 (54.84 - 73.81) |
| General health | 54.16 ± 17.78 (44.31 - 64.01) | 55.83 ± 22.09 (43.59 - 68.06) | 53.33 ± 19.46 (42.55 - 64.11) | 58.33 ± 25.29 (44.32 - 72.34) |
| Total SF - 36 score | 53.64 ± 16.09 (44.72 - 62.55) | 58.93 ± 12.87 (51.80 - 66.06) | 57.95 ± 14.56 (49.88 - 66.02) | 61.04 ± 13.00 (54.20 - 68.60) |
Abbreviations: 6MWT, 6-minute walking test; TUG, timed up and go test; SF-36, 36-item short form survey; LAI, Lequesne Algofunctional Index.
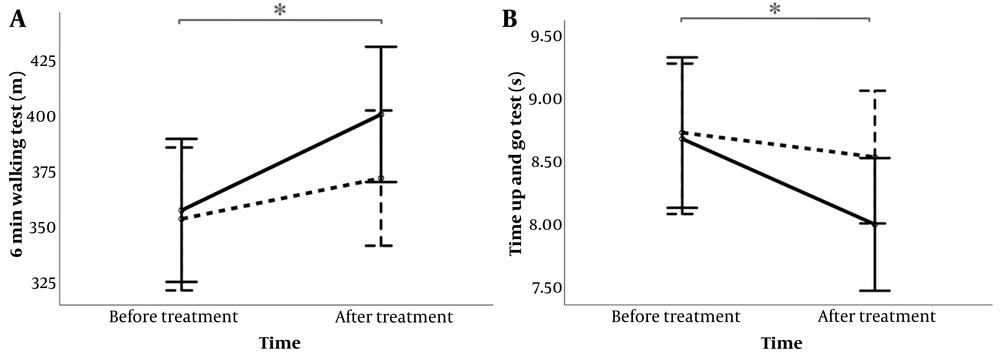
The results of the independent t-test showed no significant difference between the two groups in the pre-treatment condition for all variables (P > 0.05). Regarding the functional tests, the mixed ANOVA results indicated a significant time effect for the 6MWT (P < 0.001, ηp² = 0.386) and the TUG test (P = 0.003, ηp² = 0.272), with improvements observed after treatment as the distance for the 6MWT increased and the time for the TUG decreased for both groups. However, the trend of improvement was more pronounced for the IASTM group, as shown in Figure 2.
For the SF-36, the mixed ANOVA results revealed significant time effects in the subgroups for physical functioning (P = 0.002, ηp² = 0.292), role limitations due to physical problems (P < 0.001, ηp² = 0.367), energy/vitality (P < 0.001, ηp² = 0.369), pain (P < 0.001, ηp² = 0.544), and total score (P < 0.001, ηp² = 0.551), with scores increasing after treatment for both groups. Additionally, there was a significant time*group interaction for role limitations due to emotional problems (P = 0.005, ηp² = 0.251), where the IASTM group showed an increase after treatment, while the sham group showed a decrease. For the LAI questionnaire, a significant time effect was found (P < 0.001, ηp² = 0.873), with scores decreasing after treatment for both groups.
5. Discussion
This study explored the effects of IASTM combined with exercise therapy on individuals with KOA, comparing it to a sham intervention group to assess its efficacy in enhancing functional measures and quality of life.
The findings demonstrated significant improvements in functional performance involving knee motion during multi-joint, weight-bearing daily activities, as evidenced by the 6MWT and TUG test results. Both interventions effectively enhanced functional capacity, but the trend shown in Figure 2 suggests that the combination of IASTM and exercise therapy is more effective than exercise therapy alone. This aligns with previous studies that have highlighted the benefits of IASTM on pain reduction, increased range of motion, and muscle strength (7, 11, 12, 14-17). According to existing literature, IASTM can improve range of motion and alleviate pain by enhancing blood flow, breaking down crosslinks, reducing tissue viscosity, and decreasing stiffness. The tools used in IASTM may also help alleviate pain by aiding the healing process of inflammation and influencing pain receptors. Combining these mechanisms of IASTM with exercise appears to positively impact functional tasks (7, 8, 10, 13, 14). Additionally, it is worth noting that the exercise-only group also showed improvements. These exercises, conducted over just four sessions in two weeks, underscore the importance of prescribing exercises for KOA patients as part of their treatment routine.
Regarding the quality of life assessments, the SF-36 revealed significant improvements in several categories, including physical functioning, role limitations due to physical problems, energy/vitality, pain, and total scores. These findings indicate that both treatment approaches can effectively enhance various aspects of quality of life, particularly in areas related to pain, physical function, strength, and activities of daily living, both at home and outside. Additionally, a significant time*group interaction effect was observed in the role limitations due to emotional problems category, favoring the IASTM group. This suggests that while both groups experienced similar improvements in most SF-36 categories, the IASTM group had a more pronounced positive effect on emotional limitations. The LAI questionnaire, which specifically assesses pain and daily living activities related to the knee, also showed improvements in both groups after two weeks of intervention, further supporting the benefits of these treatments.
One limitation of this study was the limited number of IASTM sessions, necessitated by the COVID-19 pandemic, which impacted participants' willingness to attend clinic visits. Although four sessions were selected based on the positive immediate effects of IASTM and previous studies suggesting benefits within two weeks (27-31), we recommend additional sessions to fully explore the treatment's potential. Despite this constraint, the four sessions were sufficient to produce significant improvements in many variables. However, increasing the number of sessions could potentially enhance these outcomes further. Beyond the number of IASTM sessions, future research should delve into the biomechanical aspects of functional tasks to better understand how IASTM enhances functional performance and to optimize treatment protocols.
5.1. Conclusions
In conclusion, this study demonstrates that combining IASTM with exercise therapy significantly enhances functional performance in individuals with KOA, as evidenced by improvements in the 6MWT and TUG test results. Both interventions proved beneficial, but the IASTM group experienced greater gains, indicating enhanced effects on activities of daily living, which is particularly important for the elderly. The SF-36 and LAI questionnaires also showed improvements across various categories for both groups, with the IASTM group showing a slight improvement in the emotional role limitations category. While both groups showed significant improvements across most variables, underscoring the critical role of exercise therapy in the treatment regimen for patients with KOA, the trends favoring greater improvements in the IASTM group suggest that continued use of IASTM could lead to even better outcomes.