1. Background
Amputation, the surgical removal of a limb, presents significant challenges, affecting not only physical function and sensation but also self-perception, social interactions, and psychological well-being (1). Psychological responses vary among amputees, with many experiencing a profound sense of loss that extends beyond the physical absence of the limb to include diminished functional capabilities, self-worth, and social connections (2). This sense of loss disrupts normalcy, often leading to feelings of vulnerability and isolation.
Several factors influence post-traumatic adjustment and well-being. Key elements include a strong social support system (3), self-esteem, and psychological support (4), all of which play a role in fostering resilience—the ability to thrive amid adversity and reintegrate into society (5). Support networks and a positive self-image promote resilience, facilitate coping, and contribute to positive outcomes after amputation (6).
A clear relationship exists between resilience and key outcomes, including depression, fatigue, sleep quality, and physical function (7). This suggests that enhancing resilience is associated with better psychological well-being, improved health, and a higher quality of life for amputees.
Furthermore, scholarly evidence emphasizes that receiving professional psychological support enhances a person's overall resilience and aids in managing mental health conditions (8). Through targeted interventions, psychological support helps distressed individuals develop coping mechanisms, regulate their emotions, and foster resilient responses to adversity. Additionally, psychological support can enhance self-esteem by mitigating the adverse effects of perceived changes on one’s self-image (9).
Amputees can maintain a positive self-image and navigate social interactions with greater confidence and resilience when they receive support in developing their sense of self-worth, embracing physical changes, and cultivating self-confidence (10). Moreover, studies on limb loss have indicated that higher levels of resilience are associated with better preservation of self-esteem post-amputation. This underscores the connection between resilience and self-esteem, demonstrating how these constructs mutually reinforce each other in promoting psychological well-being (11).
In Oman, while traumatic amputations are less frequent than pathological ones, they carry significant repercussions. The challenges faced by traumatic amputees are multifaceted, requiring attention to both physical rehabilitation and the often-overlooked psychological aspects. These amputations can occur suddenly, leading to symptoms of post-traumatic stress disorder (PTSD) (12). Focusing solely on physical rehabilitation may hinder overall progress due to unresolved psychological challenges.
Incorporating psychological interventions is essential to mitigate the risk of developing mental health issues during the adjustment process following amputation. Such interventions are crucial for ensuring successful rehabilitation and smooth reintegration into society (13). However, current rehabilitation programs often overlook these vital psychological considerations (14). Additionally, within the Omani context, there is a no lack of research evidence regarding psychological interventions and outcomes related to traumatic amputations.
This study examines the factors affecting resilience in the traumatic amputee population, addressing a knowledge gap regarding the roles of psychological support, self-esteem, and protective factors in Oman. While physical rehabilitation is essential, psychological aspects are often overlooked, which can negatively impact well-being, prosthesis adaptation, and social reintegration. This investigation aims to provide insights for developing tailored support strategies to enhance resilience and improve the quality of life for amputees in Oman and beyond.
2. Objectives
This study aims to investigate the influence of psychological support, perceived self-esteem, and protective factors on resilience among traumatic amputees in Northern Batinah, Oman. Specifically, it seeks to: (1) Explore the experiences of traumatic amputees regarding the impact of psychological support, social support factors, and self-esteem on their resilience, and examine the relationships between professional psychological support, social support, self-esteem, and resilience among traumatic amputees and (2) identify the key factors contributing to high resilience and successful adaptation among traumatic amputees in Oman.
3. Methods
This study employed a mixed-method investigation approach. A single, comprehensive questionnaire was designed to be self-administered. This mode of administration was chosen due to the sensitivity of the subject matter and the time gaps between post-amputation medical interventions and the study period. The survey included basic demographic information, three psychometric scales, and an open-text field section.
The Rosenberg Self-esteem Scale was used to measure self-esteem through a 10-item, 4-point Likert scale. The study employed the validated Arabic version to ensure cultural relevance and accuracy (15). Resilience was assessed using the Connor-Davidson Resilience Scale-10 (CD-RISC-10), a 10-item scale with scores ranging from 0 to 40, designed to evaluate an individual's perceived ability to cope with stress and adversity (16). The validated Arabic version was utilized to maintain cultural appropriateness and measurement accuracy (17).
The Protective Factors of Resilience Scale (PFRS) (18) was used to assess social resources across personal, family, and peer domains. This twenty-item scale employs a Likert-type rating on a seven-point continuum. The Arabic translation of the scale was conducted using a forward-backward translation process to ensure both linguistic and conceptual equivalence (19). A Cronbach's alpha of 0.98 indicated that the translation was highly reliable and suitable for use within Arabic-speaking communities. The Open-Ended Questionnaire aimed to explore participants' experiences with psychological support (if available) and its effects on resilience. Alongside personal data sheets and information forms, the self-administered scales were analyzed using the Statistical Package for Social Sciences (SPSS v.29). A codebook was created prior to data analysis, with coding based on the study's scope and psychometric scales. This systematic approach aligned with the research objectives, facilitating structured data exploration to identify common patterns and themes.
3.1. Inclusion Criteria
Participants in the study were required to have undergone an amputation due to trauma within the past five years prior to selection. Additionally, their medical care, from pre-amputation to post-amputation, must have been provided in North Batinah. The causes of trauma could include home accidents, work-related injuries, or traffic incidents. This specific criterion ensured that the study focused on individuals with a common background regarding the circumstances of their amputation and the healthcare services they received. This approach allowed for a more targeted investigation of the relevant factors affecting their self-esteem, resilience, and protective factors.
3.2. Exclusion Criteria
Individuals under 18 years of age were excluded from the sample to ensure compatibility with the psychometric scales used and to guarantee the full autonomy of participants in providing informed responses. Additionally, the study excluded all patients who had not received comprehensive medical care following their amputation in North Batinah healthcare facilities. This criterion was set to ensure consistency in the participants' recovery experiences, particularly concerning the healthcare services provided.
3.3. Sample
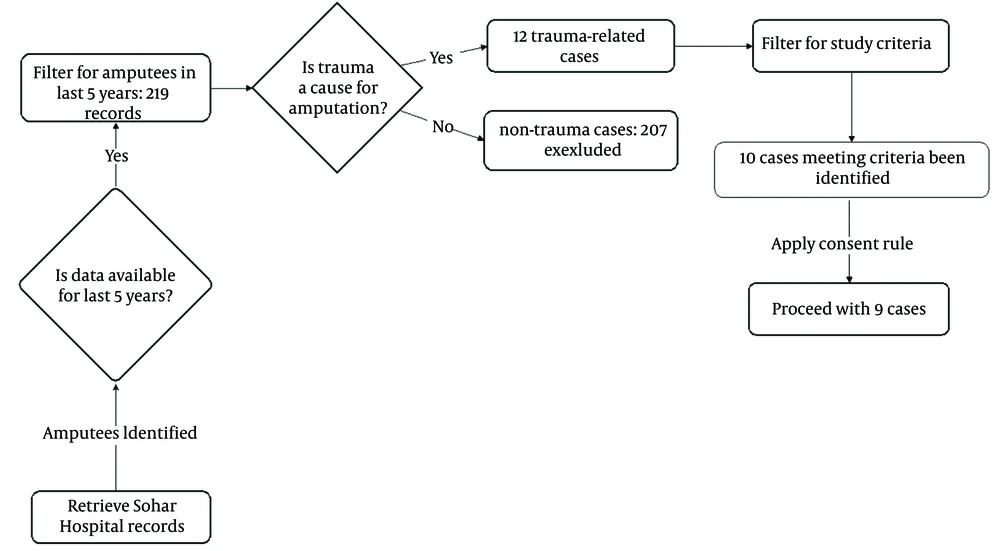
The sample selection process, illustrated in Figure 1, provides a detailed overview of the steps taken to identify and recruit participants for this study. The research team accessed the database of the Prosthetic and Physical Therapy Departments at Sohar Hospital, which serves the North Batinah region of Oman, the country’s second-largest province in terms of population.
According to Sohar Hospital records, 219 amputees received care at the facility over the past five years, with 12 individuals having undergone amputation due to trauma. From this database, 10 cases met the established selection criteria. Each of these individuals was subsequently contacted, and an invitation to participate in the study was extended. Out of these, 9 participants willingly consented to take part in this exploratory study.
3.4. Sample Size Considerations
The strict inclusion and exclusion criteria resulted in a sample size of nine patients, reflecting both the rarity of the condition and the study’s focus on a specific population. Small sample sizes are not uncommon in studies involving specialized or rare populations and are considered appropriate for exploratory research, where the primary goal is to generate foundational insights (20).
While acknowledging the limitations associated with a small cohort, this study employs a rigorous methodology to ensure the validity and reliability of the results, consistent with research approaches in similar contexts (21).
3.5. Ethical Considerations
The study was designed to protect the dignity and well-being of all participants. Research tools were carefully selected to minimize potential emotional discomfort, with a particular focus on supporting participants' mental health. Participants received detailed information about the study’s objectives, procedures, and their right to withdraw at any time without penalty, ensuring fully informed consent.
To safeguard participants' privacy, responses were anonymized, and all data were handled with the highest level of care and security. The survey was made available in multiple accessible formats to encourage participation from diverse individuals, including those with different language needs.
Additionally, participants were informed about the availability of psychological support services in case the research process evoked emotional distress. The study was conducted with ethical approval, adhering to strict standards that prioritize fairness, respect, and the protection of participants' rights and well-being.
3.6. Data Collection
Data collection took place between October 2022 and March 2023. Due to the long intervals between patients' follow-up appointments, the process took longer than anticipated as participants required additional time to respond. All participants provided written consent to participate in the study.
Responses were submitted through an electronic platform, allowing participants to complete the questionnaire in a digital environment. Quantitative data were collected and analyzed using the Statistical Package for Social Sciences (SPSS).
The textual data from open-ended responses were analyzed using Braun and Clarke's six-step thematic analysis approach (22). Common patterns and potential themes were identified through data familiarization and repeated readings. The final selection of themes was determined based on statistical relevance, requiring their occurrence in at least half of the participants’ responses. To ensure validity, these coded responses were cross-referenced with direct quotations from the questionnaires.
4. Results
4.1. Quantitative Data
Table 1 provides an overview of the raw data collected from the participants. It includes demographic information such as sex, age, and working status, along with details regarding their amputation, including the cause and type. Additionally, the table presents participants' scores on several psychological scales, including the Rosenberg Self-esteem Scale, the CD-RISC-10, and the PFRS.
| Participants | Sex, Age | Working Status | Amputation Cause | Amputation Type a, b | Post amputation Psychological Support | Rosenberg Self-esteem Scale | CD-RISC-10 | PFRS | PFRS Subscales | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Personal Resources | Family Resources | Peer Resources | |||||||||
| 1 | M, 37 | Works | Car accident | Lower | 0 | 24 | 21 | 20 | 10 | 5 | 5 |
| 2 | M, 34 | Works | Car accident | Lower | 1 | 37 | 40 | 80 | 40 | 20 | 20 |
| 3 | M, 56 | Unemployed | Work accident | Lower | 1 | 35 | 32 | 125 | 61 | 32 | 29 |
| 4 | M, 46 | Unemployed | Work accident | Lower | 0 | 29 | 28 | 118 | 53 | 35 | 30 |
| 5 | M, 33 | Unemployed | Car accident | Lower | 0 | 16 | 27 | 75 | 39 | 20 | 16 |
| 6 | F, 18 | Study | Car accident | Lower | 1 | 36 | 39 | 140 | 70 | 35 | 35 |
| 7 | M, 52 | Unemployed | Work accident | Lower | 0 | 29 | 27 | 60 | 40 | 10 | 10 |
| 8 | M, 37 | Works | Car accident | Upper | 0 | 31 | 37 | 95 | 51 | 30 | 14 |
| 9 | M, 32 | Unemployed | Car accident | Lower | 0 | 24 | 25 | 99 | 64 | 30 | 5 |
Abbreviations: M, male; F, female; CD-RISC-10, Connor-Davidson Resilience Scale-10; PFRS, Protective Factors of Resilience Scale.
a Lower: Lower extremity amputation: Removal of part or all of the lower limb (e.g., toe, foot, below-knee, above-knee) due to trauma, disease, or infection.
b Upper: Upper extremity amputation: Loss of part or all of the upper limb (e.g., hand, forearm, arm) due to trauma, malignancy, or congenital causes.
Table 2 provides the descriptive statistics for the three psychological scales. The Rosenberg Self-esteem Scale had a mean score of 29.0 (SD = 6.82), with scores ranging from 16 to 37. The CD-RISC-10 showed a mean score of 30.67 (SD = 6.69), with scores ranging from 21 to 40. The PFRS exhibited the greatest variability, with a mean score of 90.22 (SD = 36.64) and scores ranging from 20 to 125.
| Scales | Count | Mean ± SD | Min - Max |
|---|---|---|---|
| Rosenberg Self-esteem Scale | 9 | 29.00 ± 6.82 | 16.0 - 37.0 |
| CD-RISC-10 | 9 | 30.67 ± 6.69 | 21.0 - 40.0 |
| PFRS | 9 | 90.22 ± 36.64 | 20.0 - 125.0 |
Abbreviations: CD-RISC-10, Connor-Davidson Resilience Scale-10; PFRS, Protective Factors of Resilience Scale.
Spearman’s correlation analysis was used to explore the relationships across the three psychological scales, as it is well-suited for small sample sizes and non-normally distributed data. Table 3 displays the correlation coefficients between the Rosenberg Self-esteem Scale, CD-RISC-10, and the PFRS. The analysis revealed a strong positive correlation between self-esteem and resilience (r = 0.76). Additionally, there was a moderate positive correlation between self-esteem and protective factors (r = 0.49). Resilience and protective factors also demonstrated a moderate positive correlation (r = 0.57).
Abbreviations: CD-RISC-10, Connor-Davidson Resilience Scale-10; PFRS, Protective Factors of Resilience Scale.
a Correlation is significant at the level (P ≤ 0.05).
Comparisons across the three psychological scales were conducted based on participants' employment status. Mean scores were analyzed between employed and unemployed participants to identify any significant differences. This analysis aimed to account for potential confounding effects of employment status on self-esteem, resilience, and protective factors, ensuring a more accurate interpretation of the results.
Study participants reported the highest mean scores across all three psychological scales, with a self-esteem score of 36.0, a resilience score of 39.0, and a protective factors score of 140, as shown in Table 4. Employed participants exhibited intermediate scores, while unemployed participants reported lower scores across all scales, indicating potential differences linked to employment status.
| Working Status | Rosenberg Self-esteem | CD-RISC-10 | PFRS |
|---|---|---|---|
| Works | 30.67 | 32.67 | 65.0 |
| Unemployed | 26.60 | 27.80 | 95.4 |
| Study | 36.00 | 39.00 | 140.0 |
Abbreviations: CD-RISC-10, Connor-Davidson Resilience Scale-10; PFRS, Protective Factors of Resilience Scale.
In Table 5, participants were grouped based on whether they had received psychological support, and comparisons were made across the three scales. This analysis highlighted notable differences in mean scores between the two groups, providing insights into the potential influence of psychological support on self-esteem, resilience, and protective factors.
| Psychological Support (Post-amputation) | Rosenberg Self-esteem | CD-RISC-10 | PFRS |
|---|---|---|---|
| 0 (no support) | 25.5 | 27.5 | 77.83 |
| 1 (received support) | 36.0 | 37.0 | 115.0 |
Abbreviations: CD-RISC-10, Connor-Davidson Resilience Scale-10; PFRS, Protective Factors of Resilience Scale.
As shown in Table 5, participants who received psychological support exhibited significantly higher scores on the Rosenberg Self-esteem Scale (36.0 versus 25.5), the CD-RISC-10 (37.0 versus 27.5), and the PFRS (115.0 versus 77.83) compared to those who did not receive such support.
Due to the small sample size, advanced statistical analyses were not feasible. However, the results were interpreted with careful consideration of the effects of psychological support and employment status to maintain transparency and reduce potential bias.
4.2. Qualitative Data
The participants come from different age groups, sexes, and employment statuses, reflecting a diverse range of backgrounds. Each participant’s unique characteristics contribute to their individual psychological journey. The responses to the open-ended questions, presented in Box 1, provide an in-depth perspective on their experiences and adaptation processes following amputation.
| Questions |
|---|
| What difficulties did you encounter when adapting to life after the amputation? |
| How have your feelings about yourself changed since the amputation? |
| Did you receive professional psychological support? If so, how did it affect your adaptation process? |
| What helped you adapt well after the amputation? |
| Can you share how your family and friends have supported you during your journey of adaptation after amputation? |
The written responses provided by the study participants were carefully analyzed line by line. The data were analyzed using a six-step thematic analysis based on Braun and Clarke’s framework (2006), with the support of ATLAS.ti software (version 24.1.0) for coding and organizing themes, as shown in Table 6, within a structured framework and maintaining a strict systematic data classification and interpretation method.
| Themes | Sub-themes | Codes | Frequency of Mention (No. of Patients) |
|---|---|---|---|
| Self-perception as a determinant of resilience | Positive self-perception | Self-confidence boost | 12 (7) |
| Self-acceptance | 13 (5) | ||
| Challenges in self-perception | Doubts about self-worth | 3 (1) | |
| Social support theme | Family support | Emotional support from family | 6 (4) |
| Practical assistance from family | 8 (6) | ||
| Friendship and social connections | Contact with friends | 5 (3) | |
| Social isolation | Social withdrawal | 0 | |
| Impact of professional psychological support on resilience | Improved coping skills | Improved coping strategies | 0 |
| Growth in emotional strength | Growth in emotional resilience | 10 (8) | |
| Key contributors to resilience | Prosthetic adaptation and independence | Prosthesis acceptance | 6 (6) |
| independence | 7 (6) |
Thematic analysis was conducted using the six-step approach (22). This process consisted of familiarization with the data, generating initial codes, searching for themes (descriptive), reviewing themes (concepts and reflections), further defining and naming themes, and writing up the results. A deductive coding process was employed, using pre-existing concepts and theories as a guide. The thematic analysis of the narratives of the nine patients resulted in four main themes: Self-perception as a determinant of resilience, perceived social support, influence of psychological support on resilience, and key contributors to resilience. These themes broadly capture the significant patterns found in the data and correspond to our research aims.
4.2.1. Theme 1: Self-perception as a Determinant of Resilience
Seven patients cited a gain in self-confidence, emphasizing the empowering effect of self-perception on their ability to cope with adversity. This highlighted that patients with a more favorable perception of themselves felt better adjusted after amputation.
- “I could do everything for myself.” – Patient 2
- “I didn’t change after the accident, and I feel good about myself. This is predestination.” – Patient 6
- “I have overcome challenges that I never thought I could. I became strong... and I got married and I have children after the accident.” – Patient 3
- “I am independent of everything in my daily activities.” – Patient 4
- “I am well and able to do most of my daily activities independently.” – Patient 5
- “I feel okay, and I am still strong.” – Patient 8
- “I’ve become more capable of doing most things on my own, but I still need help sometimes.” Patient 9
Conversely, only one patient expressed self-doubt and a negative self-image, which may have negatively impacted their recovery:
- “Going for a prosthetic was not easy, and I was unsure if this would help me to mobilize. Being alone was difficult during that time.” – Patient 1
4.2.2. Theme 2: Social Support
Social support emerged as another significant factor in the participants' responses. Six participants cited receiving practical family assistance, while four participants highlighted both emotional and practical support from their families. This underscores the crucial role of family commitment in the recovery process. Interestingly, none of the patients reported experiencing social withdrawal; instead, they maintained strong connections with others rather than isolating themselves.
Additionally, three participants stated that interactions with friends played a supportive role during their recovery, suggesting that both family and social networks contribute to better adjustment following amputation.
- “They told me I need to be strong and face my reality.” – Patient 2
- “My family always said to me that I am capable of doing anything I want.” – Patient 3
- “Everyone in my family encouraged me to be strong. My family helped me every day until I recovered fully.” – Patient 4
- “The support from my family and my closest friends was great.” – Patient 5
- “My family has been helpful, and it’s made things a bit easier.” – Patient 8
- “I’ve received some support from my family, which has been nice.” – Patient 9
- “It’s been good to have friends check in on me from time to time.” – Patient 9
However, two participants expressed dissatisfaction with the level of family support they received, indicating that gaps in support can affect the recovery experience:
- “I was alone through this… my family is not here, but my friends did support me.” – Patient 1
- “My family tried to help me, but they didn’t really understand how I felt.” – Patient 6
4.2.3. Theme 3: Impact of Professional Psychological Support on Resilience
Three participants reported experiencing a positive impact from professional psychological support, which played a significant role in helping them adapt to life after amputation. Their responses highlighted how psychological interventions, such as counseling or support from healthcare professionals, contributed to improved coping mechanisms and emotional well-being during the recovery process.
- “The doctor taught me valuable ways to be positive… it was useful.” – Patient 2
- “I received help… I felt better after talking about my situation with a specialist.” – Patient 3
- “The social worker kept in touch often, which helped me through my recovery.” – Patient 6
4.2.4. Theme 4: Key Contributors to Resilience
Most of the responses highlighted the acceptance of prostheses and the ability to regain independence as key factors in the adaptation process. Six patients discussed how prostheses had helped them return to an independent lifestyle, considering them essential for resuming daily activities and restoring a sense of normalcy.
- “My prosthesis gave me the freedom to move again.” – Patient 3
- “The prosthesis gave me the freedom to move again. I received training to take care of it and use it.” – Patient 4
- “The artificial leg is very useful, and now I can do many things by myself.” – Patient 5
- “With the prosthesis, I can take care of myself.” – Patient 6
- “Using the artificial part made it easier to adjust and get through the tough times.” – Patient 9
Employment also emerged as an influential factor, serving as an incentive for recovery among employed participants. This finding aligns with the overall results, which showed that employment played a motivating role in the adjustment process.
- “Work… returning to work makes me feel better after the incident.” – Patient 1
- “My family and work helped me to be strong during the difficult time… I work and can do my job.” – Patient 2
- “Going to work helped me a lot.” – Patient 8
5. Discussion
This study is the first in Oman to assess the significance of psychosocial resiliency factors in amputee rehabilitation, making it a valuable contribution to understanding the various factors that contribute to recovery.
The analysis of the three scales showed differences in scores. Self-esteem and resilience had a more limited range, indicating less variability and reflecting similar psychological dimensions both within and outside individuals. In contrast, the PFRS showed significantly greater variability. These differences in responses likely reflect a broader range of external factors, primarily social and emotional support, which must be addressed to improve treatment outcomes. These results align with the themes that emerged during the thematic analysis, particularly the importance of social and psychological support as central to the participants' narratives.
The correlation analysis revealed a moderate to strong association between self-esteem, personal character strength, and protective factors. This indicates that high levels of self-esteem are linked to increased resilience, suggesting that self-esteem may play a crucial role in bolstering resilience among individuals with amputations. However, the weak correlation between self-esteem and protective factors highlights the necessity of external resources to complement internal psychological strengths.
The comparison among demographic groups demonstrated how external factors influenced the rehabilitation process. Unemployed individuals consistently scored the lowest across all scales, indicating the potential impact of employment status on psychological well-being and resilience. The significant difference between recipients of psychological support and those who did not receive such support highlights the vital role of psychological interventions in improving post-amputation recovery outcomes. This distinction underscores the critical influence of psychological support on post-amputation results, emphasizing the need for integrating mental health services into rehabilitation programs.
5.1. Qualitative Analysis and Quantitative Data
The thematic analysis resulted in four overarching themes that describe the participants’ lived experiences: Self-perception as a determinant of resilience, perceived social support, the impact of professional psychological support on resilience, and key contributors to resilience. These themes closely align with the quantitative results, reinforcing the interconnected roles of self-esteem, resilience, and protective factors in recovery.
5.1.1. Theme 1: Self-perception as a Determinant of Resilience
Seven out of nine participants emphasized the importance of self-perception as a critical component in adjusting after amputation, asserting that maintaining strength and confidence helped them remain resilient. In the quantitative analysis, a moderate correlation (r = 0.76) was found between self-esteem and resilience, supporting the interplay between these factors in facilitating better adjustment experiences. This finding underscores the variability of self-esteem among individuals and highlights the need to promote positive self-perception when developing rehabilitation support strategies.
5.1.2. Theme 2: Perceived Social Support
Social support emerged as another strong theme, with most participants believing that practical or emotional help from family and friends significantly contributed to their recovery. This finding aligns with existing research suggesting that social support serves as a protective factor in fostering resilience. The quantitative data revealed a moderate positive correlation between resilience and protective factors (r = 0.57), indicating that stronger social networks are associated with greater resilience.
However, despite the generally positive views on family support, two participants reported feeling inadequately supported by their families. Their scores on familial subscales reflected this sentiment, highlighting the importance of not just the presence but the quality of social support. This suggests that rehabilitation efforts should aim to engage the social support systems of amputees, helping families and friends provide meaningful support that meets both the emotional and practical needs of individuals.
5.1.3. Theme 3: Impact of Professional Psychological Support on Resilience
Three participants mentioned that communicating with doctors or social workers helped them adjust after amputation. This finding was consistent with the group comparison based on psychological support performed in the quantitative analysis. The quantitative assessment showed that participants who received psychosocial assistance post-amputation had significantly higher scores in self-esteem, resilience, and protective factors. This demonstrates the importance of incorporating psychological support into rehabilitation programs to improve emotional well-being and enhance resilience.
5.1.4. Theme 4: Key Contributors to Resilience
A central contributor to resilience was the acceptance of prostheses and the ability to regain independence. Six participants reported that their prosthesis enabled them to return to daily life and regain their usual level of activity. These findings align with previous research (23), highlighting the crucial role of prostheses in helping individuals adapt to their new physical conditions and maintain independence.
Another key motivator was employment. All working participants identified employment as a helpful coping mechanism after amputation, aiding them in rebuilding their lives. This observation is consistent with the quantitative comparison based on employment status, where employed participants had significantly higher self-esteem and resilience scores compared to unemployed participants.
5.2. Conclusions
The provision of psychological support for traumatic amputees is a universal necessity. This study demonstrates that access to professional psychological help significantly aids post-amputation adaptation, positively influencing self-esteem and inner resilience for those who received such support. Furthermore, the study identifies gaps in the support systems of participants, which could be addressed by integrating psychological assistance and educational programs into rehabilitation plans for both amputees and their families. Addressing the psychological burden during the rehabilitation phase is essential to ensure full recovery and improve the quality of life for amputees. It is recommended that future research be conducted on a larger scale to further explore the importance of including expert psychological support in rehabilitation programs for traumatic amputees in Oman.
5.3. Implications for Rehabilitation
The findings of this study are integral to the rehabilitation process of amputees, emphasizing the equal importance of psychological and physical factors encountered during recovery. Interventions should not only address physical rehabilitation but also target psychosocial factors, both internal and external. Programs designed to enhance positive self-perception, strengthen social support networks, and provide psychological services are crucial for fostering resilience and overall well-being.
Additionally, the role of prosthetics in restoring independence highlights the need for continued investment in assistive technology and comprehensive training. However, these potential improvements require further investigation, as the findings of this study are not generalizable due to the limited sample size and the specific population within the study’s geographic location.
5.4. Limitations and Future Directions
This study has several limitations, primarily due to the small sample size (n = 9). The limited number of participants restricted the ability to conduct extensive subgroup comparisons, such as those based on gender, and reduced the generalizability of the findings (24). Furthermore, the reliance on self-reported data introduced potential biases, including social desirability and recall inaccuracies (25), which may have influenced the results.
While advanced subgroup analyses were not feasible, the study addressed key variables such as employment status and psychological support to explore meaningful trends. Future research should consider larger sample sizes and longitudinal designs to provide deeper insights into self-esteem, resilience, and protective factors from a lifespan perspective. Additionally, focusing solely on three psychological constructs may have overlooked other relevant factors. Incorporating variables such as anxiety and depression could offer a more comprehensive understanding of the recovery process and psychological adaptation following amputation.