1. Background
Osteoarthritis (OA) is the most common joint disease (1), affecting 60 - 90% of individuals over the age of 65, and is the leading cause of chronic disability in most populations (2). Approximately 80% of patients with OA experience restricted mobility, and 25% report difficulty completing essential daily activities (3). Key symptoms of knee osteoarthritis (KOA) include pain, morning stiffness, joint swelling, reduced range of motion, diminished physical function, limitations in social activities, and/or a decline in work capacity (4).
Patients with KOA exhibit significantly reduced proprioception compared to healthy individuals (5). Proprioception is best described as the perception of limb and joint position and movement in space and is considered a component of the somatosensory system (6, 7). In the knee joint, proprioception relies on mechanoreceptors that detect changes in joint position, movement, and forces. Key contributors include muscle spindles, which sense muscle stretch, and Golgi tendon organs, which monitor muscle tension. Other mechanoreceptors, such as Ruffini endings and Pacinian corpuscles, also play vital roles in maintaining joint stability and movement control (8).
Proprioceptive impairments among people with KOA have significant ramifications for daily life (9). The treatment of proprioceptive impairment is a neglected area of rehabilitation, although enhancing neuromuscular control is an important component in the restoration of functional movement (10). Exercise-based interventions are effective in mitigating the decline in proprioception in older adults (11). For example, Khajeh et al. found that eight weeks of aquatic neuromuscular exercises significantly improved knee proprioception and pain in women with moderate to severe KOA (12).
Apart from proprioceptive deficits, patients with KOA also exhibit variations in temporal-spatial, kinematic, and kinetic parameters in gait analysis. In this context, Zeni and Higginson (13) concluded that most gait variables vary due to a reduction in walking speed, as patients with KOA tend to walk at a slower pace. This reduction in gait speed influences various measures of lower-limb gait, resulting in an overall decline in mobility and functional independence.
Furthermore, it has been estimated that over 50% of falls in the elderly occur during walking and are primarily attributed to a lack of adequate physical fitness and muscular strength (14-16). Therefore, interventions targeting these factors, such as balance and strength training, are likely to be beneficial for improving gait and reducing fall risk.
Exercise is generally recognized as a uniformly effective intervention for KOA. However, older adults are often excluded from specific exercises due to their increased vulnerability to both general and, more importantly, musculoskeletal injuries compared to younger adults (17). Prevention-focused exercises are essential for older adults to ensure they benefit from physical training without further joint deterioration.
Aquatic therapy is frequently recommended because the properties of water, including buoyancy and hydrostatic pressure, make it an ideal environment for rehabilitation. Buoyancy provides a supportive force that minimizes joint impact, allowing exercises to be performed with less pain and strain. Hydrostatic pressure or resistance acts equally in all directions on the body, enhancing movement awareness, control, and balance. This controlled environment enables more efficient engagement in exercises than is typically possible on land, especially for patients with KOA (14).
Fantozzi et al. found that walking in water significantly alters gait speed in elderly individuals (18). Garbi et al. demonstrated that a structured aquatic physiotherapy program significantly improved functional capacity and mobility in elderly patients with OA (19). Taglietti et al. showed that an eight-week aquatic exercise program significantly improved pain and function in individuals with KOA compared to a patient-education program, with sustained benefits observed at a three-month follow-up. However, no significant differences between the groups were noted in functional mobility (20).
Although aquatic therapy has been widely documented in the literature to have positive effects on physical function (21) and pain intensity (22) in patients with KOA, there is still limited knowledge about its effects on proprioception and gait speed in older women with KOA.
The necessity of this study lies in the profound impact of KOA on the daily lives of older adults. Impaired proprioception and reduced gait speed are critical consequences of KOA that directly affect mobility, increase fall risk, and diminish overall quality of life. Falls, a leading cause of injury and loss of independence in the elderly, are strongly linked to deficits in proprioception and reduced walking ability. For older women, who often have a higher prevalence of KOA and are at greater risk for osteoporosis and fractures, these issues become even more pressing.
Existing evidence supports the use of aquatic therapy in reducing pain and enhancing joint function in older adults with OA (23). However, targeted studies focusing on its impact on proprioception and gait mechanics, specifically in older women, remain limited.
2. Objectives
This study aims to address this gap by evaluating the effects of an eight-week aquatic therapy program on knee proprioception and gait speed in older women with KOA. By focusing on these two functional outcomes, this research seeks to provide evidence-based recommendations for non-pharmacological interventions that are safe, effective, and accessible for this population.
3. Methods
3.1. Participants
This study was conducted as a randomized controlled trial (RCT) with a single-blind, pre-test, and post-test design. Prior to participation, all participants provided written informed consent and were assured of their right to withdraw from the research at any stage. Ethical approval for this research was granted by the Institutional Review Board of Urmia University, with the ethical code IR.URMIA.REC.1402.027. This study was registered as a clinical trial on the Iranian Registry of Clinical Trials (IRCT20190908044722N7) on 26 November 2024. The trial was conducted in accordance with the CONSORT 2010 guidelines to ensure adherence to best practices in reporting and transparency.
A total of 34 elderly women with KOA were recruited using a non-random, convenience-driven method based on strict adherence to the inclusion and exclusion criteria. The minimum sample size, calculated using G*Power software version 3.1.9.2 (effect size F: 0.5; α error probability: 0.05; power: 0.80; numerator: 1; number of groups: 2; number of covariates: 1), was determined to be 34 participants.
Participants were required to meet the following inclusion criteria:
- Women aged 63 to 68 years, diagnosed with KOA by a certified rheumatologist through clinical assessment and X-ray examination.
- Inactive individuals, defined as engaging in less than one hour of physical activity per week (24).
- Free from severe medical conditions such as diabetes, asthma, cardiovascular diseases, neurological conditions (e.g., seizures, brain surgeries, or chronic headaches), or skin diseases (25).
- Body Mass Index (BMI) below 40 kg/m².
- Not participating in any other clinical study at the time of recruitment.
- No history of brain implants or cardiac pacemakers.
Participants were excluded if they met any of the following exclusion criteria:
- A history of knee surgeries or other joint diseases that could impair gait or affect performance in assessments.
- A cortisone injection in the knee joint within the past month (26).
- Severe respiratory, neurological, or musculoskeletal disorders, or left ventricular dysfunction.
- Untreated hypothyroidism or hyperthyroidism.
- Symptoms of cold, infections, or other illnesses reported during the study period.
Participants were recruited from a clinic in Ardabil, Iran, by reviewing the records of patients who had visited the center over the past two years. Eligible patients were contacted and invited to attend an information session where the research objectives, procedures, and potential side effects were thoroughly explained. Patients were examined by a rheumatologist, and participants were required to have completed the Kellgren-Lawrence (KL) grading scale assessment within the last six months. The KL scale is a widely used method for evaluating the severity of KOA. Participants were included in the study only if they had a KL grade of 1 or higher, indicating the presence of some degree of osteoarthritis (27).
Afterward, participants underwent a pre-test assessment. A total of 34 patients were randomly assigned to either the aquatic therapy group or the control group using Random Allocation Software version 1.0.0 (Freeware for Windows XP/Vista/7/8/10/11). This software generated a random sequence to ensure equal allocation of participants to each group. A single individual, blinded to the group allocation, managed the enrollment and assignment process to maintain the integrity of the randomization.
Following the 8-week intervention, a post-test assessment was conducted. All evaluations were performed by an author blinded to the participants' group assignments. The study was supervised by an experienced exercise professional and a medical doctor. Participants were allowed to continue taking any medications they had been prescribed for at least 30 days prior to study enrollment.
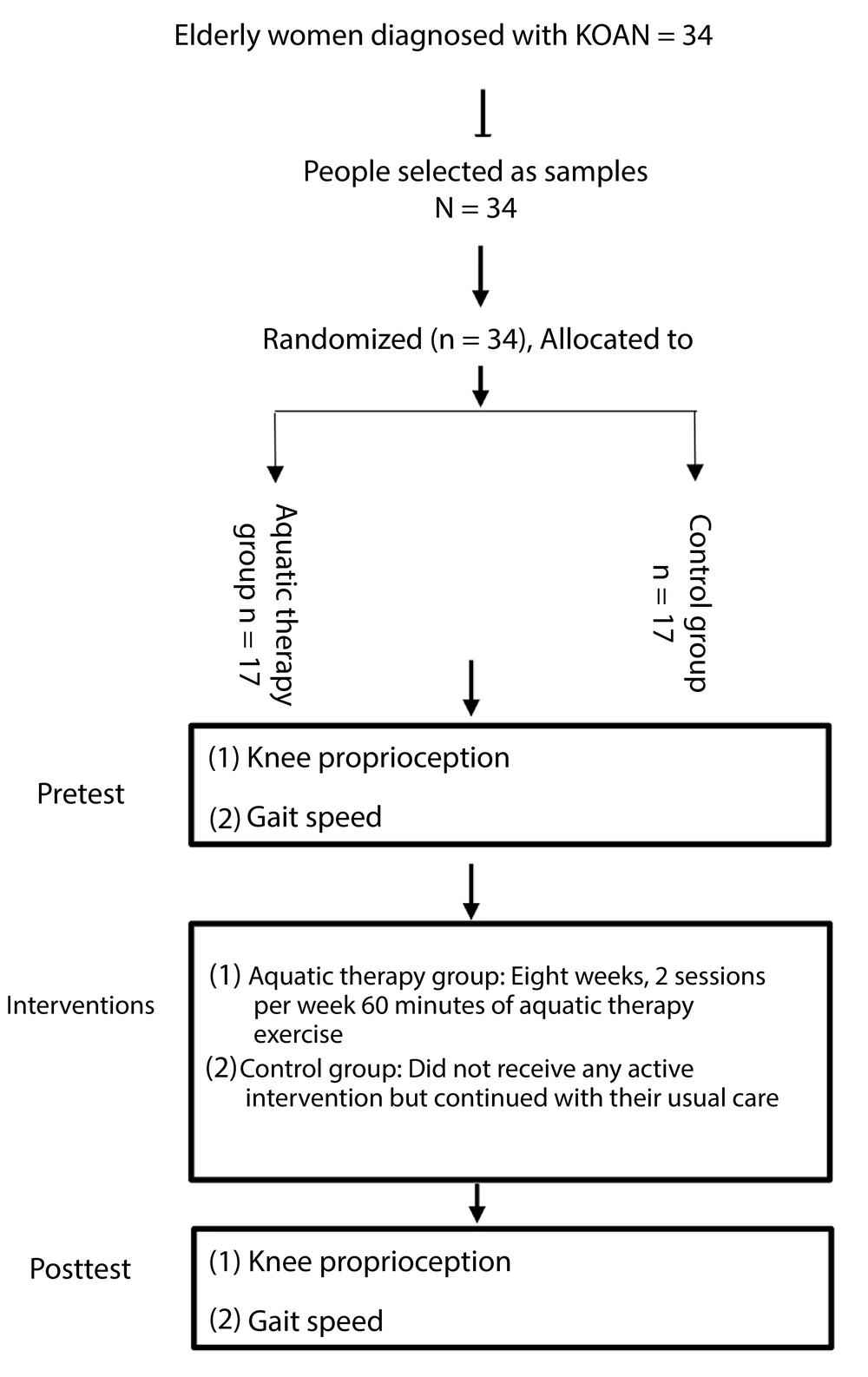
A flow diagram summarizing the study process is presented in Figure 1.
3.2. Outcome Measures
3.2.1. Knee Proprioception
To evaluate the sense of knee joint position, a digital goniometer (Model: XYZ, Zanij Industrial Research and Development Co., Iran) with an accuracy of 0.1 degrees was used. This device features a protractor system, a digital reader, a calibration package, information recording and processing software, and two arms—fixed and movable—made of aluminum. Previous studies have demonstrated the reliability and validity of digital goniometers for similar assessments (e.g., r = 0.75 for validity) (28).
Participants were seated with their knee flexed at 85°, and they were asked to replicate a target knee angle of 60° without visual feedback. Three trials were conducted, and the average error from the target angle was recorded as the measure of knee proprioception (29). The right knee was used for the proprioceptive evaluation.
3.3. Gait Speed
Gait speed was evaluated using the 10-Meter Walk test (10MWT) under two conditions:
(1) Gait: Participants were instructed to walk at a comfortable speed over a 10-meter distance. Time was recorded for two trials, and the average time was used for analysis.
(2) Cognitive task condition: Participants were asked to perform a dual-task by walking the 10-meter distance while simultaneously engaging in a visuospatial N-back task. The N-back task is a cognitive test in which participants monitor a series of stimuli and respond to whether the current stimulus matches a stimulus presented a specific number of items earlier in the sequence (in this case, one item back). Participants were instructed to respond verbally to each stimulus by saying “similar” or “dissimilar” as appropriate (30).
3.4. Interventions
3.4.1. Aquatic Therapy Protocol
Participants in the aquatic therapy group completed an 8-week program, consisting of 2 sessions per week, held at Ardabil's Jam swimming pool. Each session lasted 60 minutes, including a 10-minute warm-up, 45 minutes of water exercises such as: Heel raises, mini squats, hip abduction, hip extension, hip flexion, step-ups, and arm movements, followed by a 5-minute cool-down. The water temperature was maintained at 34 - 36°C, and the air temperature at 24°C. Exercises, performed in chest-deep water, included walking forward and backward, hip flexion and extension, hip rotation, side walking, and single-leg standing. A lifeguard was present during all sessions, and a physician supervised the intervention (31).
Participants began with three repetitions of each exercise in the first session, progressing to three sets of ten repetitions by the end of the program, in accordance with the principle of progressive overload.
3.4.2. Control Group
The control group did not receive any active intervention and continued with their usual care.
3.5. Data Analysis
All statistical analyses were performed using SPSS 26.0. The Shapiro-Wilk test, Levene's F test, and ANCOVA test were used to check the normality of data distribution, homogeneity of variances, and homogeneity of regression slopes. Analysis of covariance (ANCOVA) was used to analyze the findings.
4. Results
The characteristics of the patients are presented in Table 1. There were no significant differences in demographic characteristics between the groups.
| Characteristics | Aquatic Therapy (n = 17) | Control (n = 17) | P-Value |
|---|---|---|---|
| Age (y) | 65.05 ± 1.34 | 65.17 ± 1.66 | 0.82 |
| Weight (kg) | 75.12 ± 7.809 | 73.74 ± 6.53 | 0.46 |
| Height (m) | 163.06 ± 1.74 | 162.19 ± 2.63 | 0.13 |
| Mean disease duration (y) | 3.41 ± 1.41 | 3.70 ± 1.53 | 0.56 |
| Radiological stage (K.L) | |||
| Left | |||
| Stage II | 7 (41.2) | 7 (41.2) | |
| Stage III | 10 (58.8) | 10 (58.8) | |
| Right | |||
| Stage II | 10 (58.8) | 7 (41.2) | |
| Stage III | 7 (41.2) | 10 (58.8) |
Characteristics of Patients a
Using ANCOVA with pretest values as the covariate, the results of this study (Table 2) indicate that both gait speed and knee proprioception were significantly affected by the eight-week aquatic therapy intervention. After adjusting for the pretest scores, a significant effect was observed for gait speed under normal conditions [F (1, 31) = 37.754, P < 0.001, partial ƞ² = 0.549], indicating that the intervention accounted for 54.9% of the variance in gait speed improvement. A comparative analysis of the adjusted group means revealed that the aquatic therapy group’s mean score for gait speed (estimated mean = 10.08) was significantly lower than that of the control group (estimated mean = 12.16).
| Variables | Aquatic Therapy | Control | F | P-Value b | Partial Eta Squared |
|---|---|---|---|---|---|
| Gait speed under normal conditions | 10.10 ± 1.42 | 12.14 ± 1.56 | 37.754 | 0.001 | 0.549 |
| Gait speed under dual task conditions | 12.52 ± 2.12 | 14.66 ± 1.23 | 15.371 | 0.001 | 0.331 |
| Knee proprioception | 11.41 ± 3.53 | 14.41 ± 3.18 | 10.316 | 0.003 | 0.250 |
Effects of Aquatic Training on Knee Proprioception and Gait Speed Among Female Older Adults with Knee Osteoarthritis a
Similarly, gait speed under dual-task conditions demonstrated a significant intervention effect [F (1, 31) = 15.371, P < 0.001, partial ƞ² = 0.331], with 33.1% of the variance explained by the training. Examination of the adjusted mean scores indicated that the aquatic therapy group’s average gait speed under dual-task conditions (estimated mean = 12.50) was lower than that of the control group (estimated mean = 14.68).
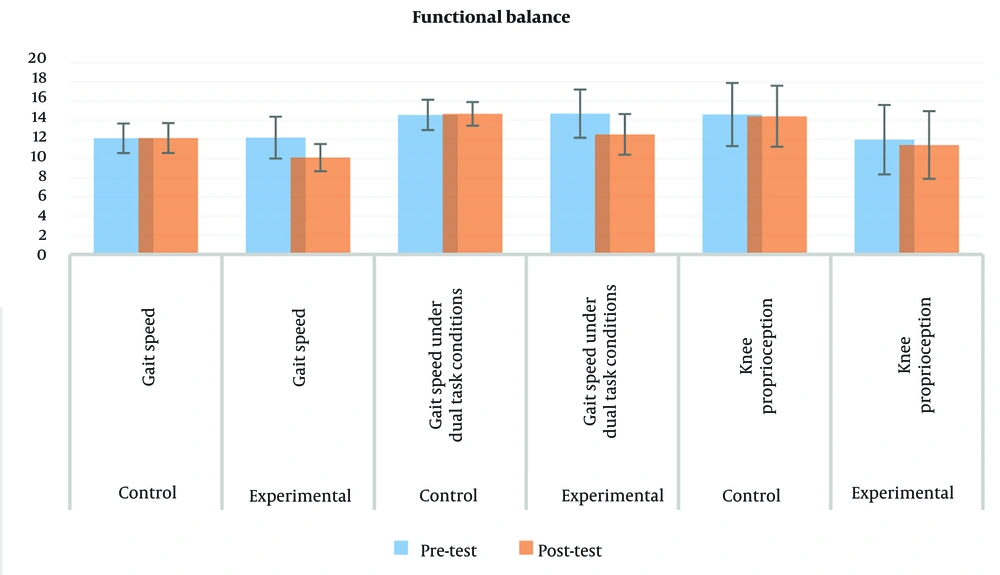
In terms of knee proprioception, the intervention showed a statistically significant effect [F (1, 32) = 10.316, P = 0.003, partial ƞ² = 0.250], with the aquatic training explaining 25% of the improvement in knee proprioception. The adjusted mean comparisons revealed that the aquatic therapy group’s average knee proprioception (estimated mean = 12.68) was significantly lower compared to the control group (estimated mean = 13.14) (Figure 2).
5. Discussion
The results of this study demonstrate that an eight-week aquatic therapy intervention significantly improved both gait speed—under normal and dual-task conditions—and knee proprioception in elderly women with KOA. These findings align with previous studies that highlight the positive effects of aquatic therapy on joint function and mobility (32, 33). Aquatic therapy is known to enhance proprioception in various populations, including athletes recovering from injuries. For example, a study on athletes following ACL reconstruction found that aquatic proprioceptive training significantly improved joint position sense and knee function compared to traditional land-based rehabilitation (34). These benefits are likely due to the unique properties of water, such as buoyancy and hydrostatic pressure, which reduce non-weight-bearing stresses on the joint while amplifying sensorimotor responses.
Similar benefits have been reported in stroke patients, where aquatic interventions have shown improvements in gait speed and balance. Specifically, underwater gait training, particularly with progressively increasing speed, led to greater improvements in gait speed and balance compared to land-based training for both conditions assessed (35). Additional studies on water-based treadmill retraining in stroke patients have also demonstrated enhanced gait speed and lower extremity function, further supporting the use of the aquatic environment in rehabilitation interventions (36). The mechanisms underlying the improvements in gait speed under normal and dual-task conditions are likely multifaceted. In the normal condition, aquatic therapy may improve gait speed by enhancing muscle strength, reducing joint pain, and improving neuromuscular coordination.
During dual-task conditions, the cognitive demands of the N-back task can interfere with gait performance. However, aquatic therapy may improve cognitive function and attention (37), enabling individuals to better manage dual-task demands and maintain gait speed. These findings also align with previous research demonstrating the positive effects of aquatic therapy on gait speed and balance in older adults with KOA. Fantozzi et al. (18) and Garbi et al. (19) have shown that aquatic exercises can significantly improve functional capacity and mobility in elderly populations. However, this study differs from previous research by specifically focusing on proprioception. While prior studies have examined broader functional outcomes, these findings highlight the unique contribution of aquatic therapy in improving proprioception, which is a critical component of balance and gait control.
The discrepancy in functional mobility findings, compared to Taglietti et al. (20), may be attributed to several factors. First, our study population may have had a higher baseline level of functional impairment, which could have limited the potential for significant improvements in this domain. Second, differences in the intensity, duration, and specific exercises of the aquatic therapy programs could have influenced the outcomes. Finally, the assessment tools used to measure functional mobility may have differed in sensitivity and specificity.
Results from the present study indicate that aquatic therapy may offer a valid therapeutic alternative for improving gait speed and proprioception in older female patients with KOA. Aquatic exercises, due to their low-impact nature, reduce pain by lessening the load on the knee, thereby creating better conditions for gait and proprioception (38). The constant resistance of the water challenges proprioceptive receptors, improving joint position sense and neuromuscular strength (34, 39). Muscle strengthening is also enhanced by the water's resistance, which promotes stability, walking efficiency, and gait speed. Water buoyancy aids in improving joint mobility/ROM and flexibility, while hydrostatic pressure challenges balance and further promotes improvement in proprioception and coordination (40).
The findings of this clinical trial have significant clinical implications for the management of KOA in older adults. Aquatic therapy can be a safe and effective intervention for improving gait speed, balance, and proprioception, ultimately enhancing functional independence and quality of life. Healthcare providers should consider incorporating aquatic therapy into treatment plans for patients with KOA, particularly for those who may not tolerate high-impact land-based exercises.
While this study primarily focused on proprioception and gait speed, future research should explore a broader range of potential benefits, including pain reduction and quality of life. Additionally, the generalizability of these findings to diverse populations warrants further investigation. To optimize the effectiveness of aquatic therapy, future studies should investigate the optimal dosage and intensity, as well as the impact of individual factors such as age, sex, and comorbidities.
5.1. Conclusions
The present study found that an eight-week aquatic therapy program significantly improved gait speed and knee proprioception in older women with KOA. These findings suggest the therapeutic value of aquatic exercises as a non-pharmacological treatment to enhance mobility and reduce functional limitations in individuals with KOA. Aquatic therapy may provide an excellent alternative for improving quality of life and independence by enhancing major functional outcomes, such as proprioception and gait speed, in elderly individuals with KOA. Further studies are recommended to explore the long-term effects of aquatic therapy, its exact mechanisms for improving proprioception and gait speed, and the response to water-based exercise in aging populations with joint disorders.