1. Background
Imagery refers to the cognitive process of mentally recreating sensory experiences in the absence of external stimuli. It arises when individuals access and manipulate perceptual information stored in memory (1). Often referred to as "seeing with the mind’s eye" or "hearing with the mind's ear", imagery is integral to many daily activities, such as decision-making, recalling past events, and envisioning the future (2). Despite its pervasive role in human cognition, research on imagery remains relatively limited.
From a clinical standpoint, cognitive interventions that focus exclusively on modifying information-processing patterns have inherent limitations in addressing psychopathology (3). This underscores the necessity for innovative therapeutic approaches, as the mechanisms driving cognitive behavioral therapy (CBT) alone appear insufficient to fully account for psychopathological change (4). Hackmann et al. emphasized that understanding a patient’s imagery can provide deeper insights into their symptoms. They suggested that imagery-based interventions could overcome current therapeutic limitations and pave the way for more innovative and effective treatments. Imagery interventions are particularly advantageous because they can induce changes in meaning systems at a deeper, more emotional level (5, 6).
Recent empirical research has increasingly highlighted the significance of imagery, which is distinguished by three fundamental characteristics. First, imagery is intrinsically linked to emotional processes, with emotionally charged memories demonstrating a greater tendency to be encoded as visual images (7). Interventions involving imagery tend to evoke stronger emotional responses compared to verbal representations (8). Second, imagery influences behavioral tendencies. Visualizing specific actions increases the likelihood of performing them, and mental expectations about the future facilitate goal-directed behaviors (9-11). Third, imagery actively shapes psychopathology by reinforcing negative emotions and cognitive biases. Dysfunctional mental images can directly worsen symptoms and sustain psychological disorders (12). Intrusive and vivid imagery is not only a hallmark symptom of various disorders such as obsessive-compulsive disorder, post-traumatic stress disorder, anxiety disorders, specific phobias, depression, and bipolar disorder but also a key factor in their onset and maintenance (13, 14). Given these characteristics, imagery is deeply implicated in various psychopathologies, and targeting it in therapy can significantly alter emotional and behavioral outcomes (15).
A growing body of research indicates that the tendency to mentally simulate future events, whether in a positive or negative light, serves as a critical maintaining factor in depressive disorders, significantly influencing both their onset and persistence (16). However, in Iran, there is a notable lack of tools to measure imagery abilities. Currently, the only available tool in the region is the Questionnaire on Mental Imagery (QMI) (17), a shortened version of a self-report scale originally developed by Betts in 1909 and later modified by Sheehan in 1967. While the QMI assesses sensory-related imagery abilities, its results have been inconsistent, particularly regarding the relationship between imagery vividness and symptom severity (18). Moreover, the QMI is rarely used in international research and has not undergone standardized validation in Iran. Previous studies suggest that positive and negative imagery abilities are independent constructs (19, 20), with depressed individuals exhibiting reduced ability to envision positive futures and heightened ability to imagine negative ones (21, 22). The QMI, however, does not measure imagery abilities based on valence, limiting its utility in research.
The prospective imagery task (PIT) has been developed as a potential solution to bridge these gaps. This tool shows promise in addressing the identified limitations effectively (23). The study by Renner et al. found that depressed individuals struggle to generate positive mental images of the future, leading to reduced reward anticipation and motivation. This impaired future imagery was directly linked to decreased goal-directed behavior. The findings suggest that enhancing positive mental imagery could help improve motivation and reward processing in depression treatment (24). Marciniak et al. examined how positive prospective mental imagery traits relate to depressive symptoms in young adults, finding that reduced vividness and positivity of future-oriented imagery were linked to higher depression. Their research highlights the role of dysfunctional mental imagery in mood pathology and potential therapeutic targets (16).
According to Pearson et al., the PIT is unique in its ability to measure imagery abilities across two independent dimensions: Positive and negative (25). Positive and negative mental images differ significantly in nature and psychological impact. Positive mental images boost well-being by evoking joy and hope, enhancing mood and self-confidence, and reducing stress. Vividly visualizing these images is crucial for emotional regulation and mental health (26-28). Negative mental imagery is associated with unpleasant memories, negative emotions, and stress, and can exacerbate symptoms of psychological disorders. When experienced as intrusive and uncontrollable, these images may increase the risk of developing mental health problems (29, 30). The PIT has demonstrated consistent results in assessing the imagery abilities of individuals with depression and is sensitive to state changes, making it suitable for evaluating the effectiveness of imagery-based interventions.
The PIT was developed through a series of studies, beginning with MacLeod et al. (as cited by Liu et al.), who pioneered the development of the subjective probability task (SPT), a psychological assessment tool designed to evaluate individuals’ perceived likelihood estimates of both positive and negative future events (31).
2. Objectives
This study addresses a critical gap in the Iranian context, where no standardized tools exist to measure imagery abilities by valence. The adaptation of the PIT enables culturally relevant assessments, paving the way for research on imagery’s role in psychopathology and its therapeutic potential. This study aimed to adapt and validate the positive and negative imagery test for use in Iran, providing a reliable tool to assess positive and negative mental imagery abilities. Despite the known role of mental imagery in mental health, the lack of standardized measures in Iran represents a significant research gap. By validating the PIT, this research facilitates future studies on imagery’s impact on psychological well-being, particularly in depression. The main gap addressed was the absence of culturally adapted tools to assess this construct, highlighting the need for cross-cultural research in this field. The findings can enhance understanding of cognitive mechanisms in depression and inform targeted interventions.
3. Methods
3.1. Study Design and Participants
This cross-sectional study utilized convenience sampling to recruit 365 Iranian participants (aged < 60 years, literate). The sample size was determined based on: (1) The recommended 10:1 participant-to-item ratio for exploratory factor analysis (EFA); (2) a power analysis (α = 0.05, power = 80%, medium effect size) using G*Power 3.1; and (3) accounting for potential missing data (0.7% imputed using multiple imputation with m = 5 datasets). Inclusion criteria required participants to be of Iranian nationality, aged below 60 years, and proficient in reading and writing. Exclusion criteria consisted of incomplete questionnaires, history of psychotic disorders, traumatic brain injury, intellectual disabilities, moderate-to-severe learning difficulties, substance use, epilepsy, seizures, or electroconvulsive therapy (ECT) within the past six months. Participants were recruited through university networks and community centers, targeting literate individuals aged < 60 years. While convenience sampling limits generalizability, demographic stratification (e.g., age, marital status) was employed to enhance diversity. Potential biases, such as overrepresentation of women (79.45%) and younger adults, are acknowledged as limitations.
3.2. Cultural Adaptation of the Prospective Imagery Task
The cultural adaptation of the PIT followed a rigorous five-step process: (1) Independent forward translation by two bilingual clinical psychologists; (2) back-translation by two independent translators blinded to the original version; (3) expert panel review (two clinical psychologists and one linguist); (4) cognitive interviews with 20 target population participants; and (5) final approval by the original PIT developers, achieving > 90% conceptual equivalence. Psychometric analyses included EFA with oblique rotation (using Kaiser’s eigenvalue > 1, scree plot, and parallel analysis for factor retention) and confirmatory factor analysis. Items were retained based on primary loadings > 0.40 and cross-loadings < 0.30. The adapted PIT demonstrated excellent reliability (α = 0.85 - 0.92, intraclass correlation coefficient (ICC) = 0.78 - 0.85). Although formal face validity assessment was not conducted, cultural appropriateness was verified during the adaptation process. While convenience sampling may limit generalizability, demographic stratification and comparison with population data (where available) were employed to enhance external validity.
3.3. Measures
3.3.1. Prospective Imagery Task
Assessed two distinct dimensions: (1) Vividness (clarity of mental imagery); and (2) likelihood (perceived probability of occurrence). Participants were instructed to mentally imagine 20 future scenarios (10 positive, e.g., "You will perform well in your course"; 10 negative, e.g., "You will have a serious disagreement with a friend"), then rate each scenario on two 5-point Likert scales: Vividness (1 = "no image at all" to 5 = "extremely vivid") and likelihood (1 = "very unlikely" to 5 = "very likely"). This adapted version demonstrated strong content validity (CVI = 0.92) through expert panel evaluation while preserving the core methodology of established protocols (20, 21).
3.3.2. Spontaneous Use of Mental Imagery Scale
A 12-item tool used to assess the spontaneous use of mental imagery in daily life. Participants rated each item on a 5-point scale, ranging from "never appropriate" to "entirely appropriate". The total score ranges from 12 to 60, with higher scores indicating greater use of imagery in everyday activities. The SUIS showed acceptable internal consistency (Cronbach’s alpha = 0.83) and has been standardized in the Iranian population, with a reported Cronbach’s alpha of 0.75 and a moderate correlation with the AST-D (r = 0.34, P < 0.01) (19, 20). In this study, the SUIS exhibited a baseline internal consistency of 0.72 (32).
3.3.3. Dimensional Anhedonia Rating Scale
A 17-item self-report questionnaire that evaluates four domains of hedonic response: Hobbies, sensory experiences, social activities, and food/drink. Items are rated on a 5-point Likert scale, from 1 ("not at all") to 5 ("very much"). The Dimensional Anhedonia Rating Scale (DARS) demonstrated strong reliability (Cronbach’s alpha = 0.75 - 0.92) and has been validated in the Iranian population, with a Cronbach’s alpha of 0.84 and a test-retest reliability coefficient of 0.77. It also exhibits acceptable convergent validity with depression measures (r = -0.37, P < 0.01) (21, 22). In this study, the internal consistency of the DARS was 0.81 at baseline, 0.86 post-training, and 0.87 at follow-up (33).
3.3.4. Beck’s Depression Inventory
A 21-item self-report measure used to evaluate the severity of depressive symptoms, scoring this inventory on a 4-point scale, ranging from 0 to 3. The Beck’s Depression Inventory (BDI-II) showed high internal consistency (Cronbach’s alpha = 0.91) and has been validated in Iran, with a reported Cronbach’s alpha of 0.91, a split-half reliability coefficient of 0.89, and a one-week test-retest reliability coefficient of 0.94 (34, 35).
3.3.5. Ambiguous Scenarios Test relevant to Depressed Mood II
A self-report test with 30 items that asks participants to vividly imagine various scenarios (e.g., related to performance, past experiences, or future situations) and rate the pleasantness of each scenario on a Likert scale, ranging from -5 ("extremely unpleasant") to +5 ("extremely pleasant"). This test was designed to evaluate depression-related interpretation biases, with higher scores indicating a more positive bias. It demonstrated acceptable internal consistency (Cronbach’s alpha = 0.87) and a significant correlation with depression scores (36). In a study in Iran, Nasrollah et al. reported that the psychometric properties of this instrument were appropriate, with good internal consistency (Cronbach’s alpha = 0.90; McDonald’s ω = 0.91). The validation of this instrument was also acceptable, with significant correlations with the BDI-II (r = -0.42, P < 0.01) (37).
3.4. Statistical Analysis
Descriptive and inferential statistical methods were used to analyze the data. Central tendency and distribution measures were calculated using descriptive statistics. The EFA was conducted to identify the underlying factor structure of the PIT. Statistical analyses were performed using SPSS 24. Discriminant validity and inter-correlations among subscales were assessed using Pearson correlation coefficients. Prior to analysis, outliers were identified using box plots, with values exceeding ± 3 standard deviations from the mean considered univariate outliers. Visual inspection confirmed that the data were normally distributed. Reliability was assessed using internal consistency measures.
3.5. Ethical Considerations
The Research Ethics Committee of the School of Medicine, Shahid Beheshti University of Medical Sciences (Ethical Code No: IR.SBMU.MSP.REC.1403.433) approved this study. Participants provided informed consent after being briefed on the study conditions, and their participation was entirely voluntary. They were assured that their data would remain confidential. Questionnaires were collected anonymously, and all information provided by participants was kept strictly confidential.
4. Results
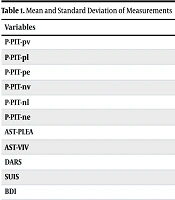
The Persian version of the prospective imagery task (P-PIT) demonstrated strong psychometric properties in a sample of 365 participants (age = 28.2 ± 7.21 years; 79.45% women). Internal consistency was excellent for all subscales, with Cronbach’s alpha values ranging from 0.82 to 0.90 (Table 1). Test-retest reliability over a two-week interval was robust (r = 0.75, P < 0.001; ICC = 0.84, P < 0.001), indicating high reproducibility.
| Variables | Mean ± SD |
|---|---|
| P-PIT-pv | 41.8290 ± 6.33854 |
| P-PIT-pl | 40.4535 ± 6.14814 |
| P-PIT-pe | 40.3140 ± 6.57766 |
| P-PIT-nv | 32.0261 ± 9.59390 |
| P-PIT-nl | 26.2464 ± 6.83316 |
| P-PIT-ne | 27.7449 ± 8.17568 |
| AST-PLEA | 80.19 ± 35.60 |
| AST-VIV | 120.70 ± 20.68 |
| DARS | 52.1416 ± 7.87476 |
| SUIS | 42.6477 ± 7.32261 |
| BDI | 10.6877 ± 9.00962 |
Mean and Standard Deviation of Measurements
The convergent validity of the P-PIT was supported by significant correlations with established measures (Table 2). Specifically, positive imagery showed moderate positive correlations with the ambiguous scenarios test for positive life events and activities (AST-PLEA) (r = 0.38, P < 0.001) and the DARS (r = 0.34, P < 0.001), while negative imagery was positively correlated with the BDI-II (r = 0.42, P < 0.001) and negatively correlated with DARS (r = -0.15, P < 0.01). Gender differences emerged, with women reporting significantly higher negative imagery vividness than men (d = 0.42). Additionally, positive imagery accounted for 11% of the variance in anhedonia scores (R2 = 0.11). The P-PIT demonstrated only weak correlations with the SUIS (r = 0.18, P < .01 for positive imagery; non-significant for negative imagery), consistent with previous findings that differentiate valence-specific imagery from general imagery use. These results collectively confirm that the P-PIT is a psychometrically sound instrument for evaluating positive and negative imagery abilities in the Iranian population.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | P-PIT-pv | 1 | - | - | - | - | - | - | - | - | - | - |
| 2 | P-PIT-pl | 0.685 a | 1 | - | - | - | - | - | - | - | - | - |
| 3 | P-PIT-pe | 0.734 a | 0.832** | 1 | - | - | - | - | - | - | - | - |
| 4 | P-PIT-nv | 0.419 a | 0.071 | 0.164 a | 1 | - | - | - | - | - | - | - |
| 5 | P-PIT-nl | -0.128 b | -0.153a | -0.151a | 0.438 a | 1 | - | - | - | - | - | - |
| 6 | P-PIT-ne | 0.073 | -0.088 | 0.066 | 0.591 a | 0.700 a | 1 | - | - | - | - | - |
| 7 | AST-PLEA | 0.329** | 0.381** | 0.378** | -0.015 | -0.212 a | -0.193 a | 1 | - | - | - | - |
| 8 | AST-VIV | 0.676 a | 0.462 a | 0.534 a | 0.424 a | -0.097 | 0.168 a | 0.286 a | 1 | - | - | - |
| 9 | DARS | 0.342 a | 0.451 a | 0.416 a | -0.002 | -0.150 a | -0.124 b | 0.383 a | 0.293 a | 1 | - | - |
| 10 | SUIS | 0.217a | 0.218 a | 0.224 a | 0.068 | -0.035 | -0.006 | 0.217 a | 0.344 a | 0.305 a | 1 | - |
| 11 | BDI | -0.328 a | -0.404 a | -0.327 a | 0.109 b | 00.424 a | 0.347 a | -0.344 a | -0.198 a | -0.39 a | -0.080 | 1 |
Correlation Matrix of Prospective Imagery Task, and (Convergent, Discriminant Validity)
The EFA revealed a two-factor structure (positive and negative imagery), accounting for 55.1% of the total variance (positive: 32.1%, eigenvalue = 6.42; negative: 23.0%, eigenvalue = 4.61). All items loaded strongly on their respective factors (> 0.40) with minimal cross-loadings (< 0.30; Table 3), confirming discriminant validity.
| Items | Scenario Type | Factor 1 (Positive) | Factor 2 (Negative) | Communality |
|---|---|---|---|---|
| 1 | Negative | 0.12 | 0.59 | 0.63 |
| 2 | Positive | 0.64 | 0.08 | 0.72 |
| 3 | Negative | 0.09 | 0.62 | 0.68 |
| 4 | Negative | 0.05 | 0.68 | 0.71 |
| 5 | Positive | 0.68 | 0.11 | 0.75 |
| 6 | Negative | 0.07 | 0.62 | 0.66 |
| 7 | Positive | 0.72 | 0.06 | 0.78 |
| 8 | Positive | 0.75 | 0.04 | 0.81 |
| 9 | Negative | 0.03 | 0.75 | 0.79 |
| 10 | Positive | 0.43 | 0.21 | 0.58 |
| 11 | Negative | 0.10 | 0.72 | 0.74 |
| 12 | Positive | 0.61 | 0.09 | 0.70 |
| 13 | Negative | 0.06 | 0.79 | 0.82 |
| 14 | Negative | 0.04 | 0.77 | 0.80 |
| 15 | Negative | 0.08 | 0.79 | 0.81 |
| 16 | Positive | 0.63 | 0.12 | 0.73 |
| 17 | Positive | 0.61 | 0.10 | 0.71 |
| 18 | Negative | 0.05 | 0.75 | 0.78 |
| 19 | Positive | 0.69 | 0.07 | 0.76 |
| 20 | Positive | 0.45 | 0.18 | 0.60 |
Exploratory Factor Analysis Results for the Persian Prospective Imagery Task (N = 365) a
5. Discussion
This study presents the first validated P-PIT, establishing its psychometric properties while highlighting important cultural considerations in mental imagery assessment. Our findings demonstrate excellent reliability (α = 0.82 - 0.90) and a robust two-factor structure (positive/negative imagery) accounting for 55.1% of variance, aligning with the original English version (21) but showing higher reliability than the Korean adaptation (8). This pattern suggests potential cultural differences in response patterns that warrant further investigation. The observed gender difference in negative imagery vividness (d = 0.42) contrasts with some Western samples but finds support in Middle Eastern studies (38), possibly reflecting cultural variations in emotional expression norms.
The correlation between positive imagery and anhedonia measures (R2 = 0.11) supports theoretical models (24) while highlighting the need for longitudinal validation, as these correlational findings suggest potential relationships rather than establishing causal mechanisms. The discriminant validity pattern differs from previous Western findings (39), underscoring the importance of cultural adaptation in imagery assessment tools. The current literature presents both consistencies and contradictions regarding imagery’s role in psychopathology that merit careful analysis. While our results generally support valence-specific models (25), they contrast with some anxiety-focused findings (40), with these discrepancies potentially stemming from cultural differences in sample characteristics, varying methodological approaches, or diagnostic heterogeneity across studies. These comparative analyses reveal both universal aspects of mental imagery processing and culturally mediated variations that complicate direct cross-study comparisons.
The clinical implications of these findings must be considered cautiously, as the cross-sectional design prevents causal inferences about imagery’s role in psychopathology. The P-PIT may help identify imagery patterns associated with psychological conditions and could potentially inform treatment planning, though its applications remain limited by the non-clinical nature of our sample and the inherent constraints of self-report methodology. Several important directions emerge for future research to address these limitations and build on our findings. Longitudinal designs are needed to examine temporal relationships between imagery patterns and clinical symptoms, while clinical validation across diagnostic groups would strengthen the tool’s practical utility. Integration with behavioral and neurophysiological measures could help overcome self-report biases, and cross-cultural comparative studies would further elucidate the cultural dimensions of mental imagery.
This culturally adapted tool advances mental health assessment in Persian-speaking populations while contributing to a broader understanding of imagery’s cross-cultural manifestations. The findings highlight both universal aspects of mental imagery and culturally specific expressions, offering a foundation for more nuanced, culturally sensitive approaches to imagery assessment and intervention across diverse populations. Future work should particularly focus on reconciling divergent findings across cultures and establishing the clinical predictive validity of these imagery measures through rigorous longitudinal designs.
5.1. Conclusions
This study successfully validated the Persian version of the PIT, establishing its strong psychometric properties, including excellent internal consistency (α = 0.85 - 0.92), test-retest reliability (ICC = 0.78 - 0.85), and construct validity. The PIT’s unique capacity to separately assess positive and negative imagery abilities makes it particularly valuable for clinical applications in the Iranian context, where it can: (1) Enhance diagnosis by identifying imagery disturbances characteristic of PTSD (intrusive trauma imagery) and depression (recurrent negative imagery); (2) guide imagery-focused interventions such as imagery rescripting therapy; and (3) monitor treatment progress in cognitive-behavioral and other imagery-based therapies. While the convenience sampling approach suggests caution in generalizing findings, this validated tool fills a critical gap in Iran’s mental health assessment toolkit and provides a foundation for future research on imagery processes in Persian-speaking populations. Future studies should examine the PIT’s predictive validity in longitudinal treatment outcomes and its sensitivity to cultural variations in imagery experiences.