1. Context
Approximately 50% of residents in rehabilitation centers for addiction experience psychosocial issues. This period of education is a critical time for increased awareness, as individuals struggling with addiction are particularly vulnerable to substance abuse and associated psychosocial problems (1). Social support is crucial for substance addiction recovery, preventing relapse, and fostering long-term sobriety. Research indicates that factors such as curiosity, peer influence, and drug availability contribute to addiction. Rehabilitation programs often combine medical therapy, such as methadone, with comprehensive social support that addresses vocational, physical, psychosocial, and spiritual aspects. Strong social networks, including new recovery communities, facilitate social identity change, which is crucial for sustained recovery. Essentially, robust social support significantly improves treatment outcomes and promotes lasting sobriety (2-4).
Social support is vital for individuals with substance addiction who are seeking a healthier, drug-free life. This support network — comprising rehab staff, family, friends, and the community — must offer empathy and understanding, helping individuals build a new identity and hope for the future. Positive social support is essential for success (3). The key features of socio-psychological rehabilitation include a multidisciplinary team approach and individualized treatment planning. Holistic interventions address physical, emotional, social, and vocational well-being, and community-based services.
1.1. Recovery-Focused Philosophy Emphasizing Hope and Empowerment
Kvieskiene (2003) defines social psychological rehabilitation as a targeted, comprehensive set of services designed to assist individuals with addiction issues. This approach aims to restore lost socio-psychological mechanisms, develop crucial social skills, promote a healthy lifestyle, foster independence, rebuild self-confidence, and cultivate other essential skills for societal reintegration. The ultimate goal of this rehabilitation process is to equip individuals with the necessary tools and abilities to fully participate in public life, overcoming the challenges posed by their addiction (5).
Given the high prevalence of psychosocial issues among addicted individuals in rehabilitation and the critical role of social support in achieving lasting recovery, a review study on the effectiveness of psychosocial interventions is clearly justified. Such a review can identify the most promising approaches for fostering social identity change, addressing diverse rehabilitation goals (like restoring socio-psychological mechanisms and building social skills), and ultimately facilitating successful societal reintegration for individuals battling addiction.
In this article, we have specifically emphasized the high prevalence of psychosocial issues among individuals in addiction rehabilitation, highlighted the critical role of social support in sustained recovery, and underscored the lack of comprehensive reviews evaluating the effectiveness of psychosocial interventions.
2. Objectives
These revisions aim to clarify the research gap and the importance of systematically identifying the most effective approaches for social-psychological rehabilitation in addiction recovery.
3. Methods
3.1. Review Question
Does social and psychological rehabilitation affect recovery among individuals with addiction?
3.2. Search Strategy
The search was conducted in English as well as other languages. Inclusion criteria were as follows: Studies were eligible if they included participants of any age or sex diagnosed with substance use disorders (SUDs) and evaluated social and/or psychological rehabilitation interventions. Eligible interventions included any structured psychosocial or social rehabilitation program, such as counseling, group therapy, or community-based support, aimed at supporting addiction recovery. Studies were required to include a comparison group (either pre- or post-intervention or a separate control group) and report outcomes related to social or psychological recovery (e.g., improved social functioning, psychological well-being, or quality of life). Only clinical trials or experimental studies published in peer-reviewed journals were included.
Exclusion criteria were: Studies focusing on non-addicted populations, those evaluating only pharmacological interventions, lacking relevant social or psychological outcomes, or not employing a comparative or experimental design were excluded. In the final phase of screening, 31 out of 41 assessed articles were excluded for not meeting the inclusion criteria, including:
- Study population: Participants who were not addicted individuals.
- Type of intervention: Studies lacking social or psychosocial rehabilitation interventions.
- Absence of a comparison group: Studies without pre- and post-intervention data.
- Not reporting relevant outcomes: Studies that did not report outcomes related to social or psychological recovery.
- Inappropriate study design: Such as reviews, case reports, or studies without a control group.
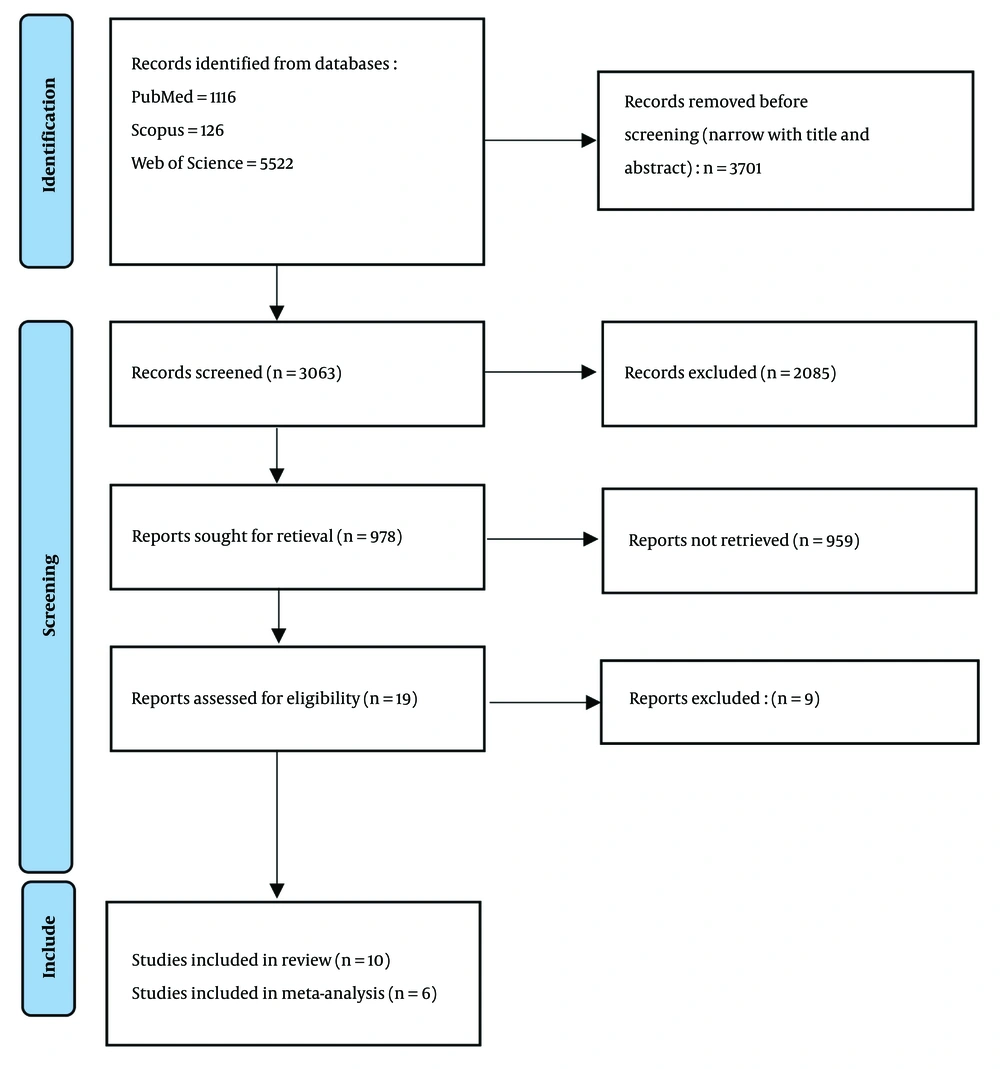
The most common reasons for exclusion were incompatibility with the required study design or intervention type, and the absence of an appropriate comparison group (Figure 1).
PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases (6).
The search was conducted using the PubMed, Scopus, and Web of Science databases with the following terms and phrases: (([([Social recovery (Title/Abstract)] OR [community recovery (Title/Abstract)]) OR [social rehabilitation (Title/Abstract)]) OR [psychological rehabilitation (Title/Abstract)]) AND [drug addiction (Title/Abstract)]) OR [substance abuse (Title/Abstract)] AND (["2000/01/01" (Date - Create) : "2025/03/31" (Date - Create)]). Finally, we examined additional sources for gray literature, such as conference papers and key academic journals (Figure 1).
3.3. Screening and Data Extraction
Two researchers independently conducted the screening of titles and abstracts for the study, with no disagreements arising during this process. Data extraction was also carried out by two reviewers independently, utilizing a standardized Excel form. The extracted data included four key components: (A) study identification (comprising the study title, first author, and publication year); (B) methodological characteristics [such as study design, sample size (SS), demographics including age and sex, rehabilitation strategies, validated measures, and quality assessment]; and (C) key findings.
3.4. Risk of Bias (Quality) Assessment
To assess the methodological quality of the included studies, standard and validated tools appropriate to the study design were used. These tools were applied consistently and uniformly to all included studies to ensure the reliability and validity of the systematic review findings. The quality assessment was conducted utilizing the CONSORT statement for randomized trials of non-pharmacologic treatments. Two independent reviewers completed the checklist for each study. Any disagreement between raters was resolved by consensus (7).
3.5. Publication Bias
Publication bias was assessed by analyzing the Egger test (8). The analysis employed a one-tailed significance threshold of α = 0.05 for intercept evaluation, while the Egger method was implemented to account for potential publication bias by estimating and incorporating omitted studies into the effect size (ES) calculation (9).
3.6. Statistical Analysis
Our primary outcome was the review of social and psychological rehabilitation on addiction recovery, and the secondary outcome was the meta-analysis of included data from pre- to post-test assessments for psychological rehabilitation. As we expected considerable heterogeneity among the studies, we used the random effects model (10). The statistical analysis was performed using Stata (version 14).
4. Results
4.1. Characteristics of Studies
Of the total number of related articles that were systematically reviewed, the characteristics of 10 articles are reported in Table 1. The research revealed that various interventions of the social and rehabilitation programs influenced the results of the whole rehabilitation in addiction recovery (Table 1).
| Authors, Y | Design | Total SS | Mean Age | Target Group | Questionnaire | Type of Rehabilitation | Goals of Rehabilitation | Key Finding |
|---|---|---|---|---|---|---|---|---|
| Yousefi, 2020 (11) | Quasi-experimental study | 24 | 38.66 | Male with amphetamine use disorders | Bart’s Impulsivity Questionnaire | Psychological intervention with ACT | Executive functions and impulse control ability | The ACT — an innovative third-wave behavioral therapy — serves as an effective intervention for reducing impulsive behaviors in patients with methamphetamine use disorder. |
| Xu et al., 2021 (12) | Randomized controlled trial | 40 | 47 | Newly drug users designated to receive community-based rehabilitation | ASI | Cares + community-based addiction rehabilitation | The UDS results examined in overall percentage of drug-positive samples | The CAREs have the potential to enhance both the effectiveness and efficiency of community-based rehabilitation programs, offering valuable insights for further system improvements. |
| Freisthler et al., 2021 (13) | Quasi-experimental study | Adult participants (n = 250) who are matched with comparison groups | NR | Child welfare-involved adults who screen positive for substances | ASI-SR | (1) Matching participants with peer recovery supporters; (2) incentivizing participation in family treatment drug court; (3) providing medications for opioid use disorders; (4) offering home-based parenting supports | (1) To reduce abusive and neglectful parenting; (2) to reduce addiction severity in parents; (3) to improve permanency outcomes for families involved with the child welfare system due to substance abuse. | (1) Family involvement (especially via FTDC programs) boosts treatment success and family reunification; (2) parental identity motivates recovery, with many striving to rebuild trust and relationships; (3) family support is a cornerstone of long-term recovery, driving individuals to transform their lives. |
| Yeung, 2022 (14) | Naturalistic treatment outcome study | 199 | 42.3 | Recovering addicts | BMMRS | Secular-based treatment emphasized the role of biological, psychological, and environmental determinants of substance abuse and provided detoxification interventions. | Developing religiosity on abstinence of substance abuse | This study examines the evolving influence of religiosity in addiction recovery, proposing a psychosocial rehabilitation framework where treatment success is built upon two core pillars: Individual personal development and community-based support systems. |
| Mahmoudi and Ghaderi, 2017 (15) | Quasi-experimental study | 50 | NR | Ex-addicts men | DASS | Acceptance and commitment group therapy | Reducing depression, stress, and anxiety | The findings of this study indicate that ACT has a beneficial impact on reducing stress and anxiety among clients. However, it does not produce a significant effect on depression. In addition to ACT, it is recommended to incorporate other complementary therapies to enhance treatment outcomes. Furthermore, researchers are encouraged to investigate the long-term effects of this therapy. |
| Mansoori et al., 2019 (16) | Experimental study | 30 | 33.02 | Addicts | Gambrill and Richey Assertion Inventory | Group counseling program sessions based on self-recognition sources | Increase assertiveness in male addicts undergoing rehabilitation | The findings indicate that group counselling education focusing on self-awareness resources enhances self-expression among individuals with addiction. This conclusion aligns with research demonstrating how structured group interventions help participants develop emotional insight and communication skills through shared experiences and guided reflection. |
| Jalili Gholami et al., 2024 (17) | Quasi-experimental study | 30 | NR | Addicted in treatment centers | RAS | Michael B. Frisch’s cognitive-behavioral psychotherapy approach | Improving the social and psychological capabilities of people addicted to social responsibility | CBT based on the Michael Frisch model leads to improved accountability in addiction treatment patients. |
| Nojavan Kanmiran et al., 2021 (18) | Quasi-experimental study | 30 | 34.66 | Subjects of addicted adolescents | Emotional Processing Scale | CFT | Emotional processing | The CFT demonstrates effectiveness in enhancing emotional regulation — the adaptive management and integration of emotional experiences — among individuals with SUDs during post-rehabilitation recovery phases. This conclusion is supported by empirical evidence showing structured compassion interventions reduce physiological stress markers (e.g., cortisol levels) while strengthening cognitive strategies for processing emotional information in addiction recovery populations. |
| Yazdanbakhsh et al., 2019 (19) | Quasi-experimental study | 20 | 46 ± 15.45 | Addicts with HIV | Temperament and Character Dimensions Scale | Cognitive-behavioral group therapy | Craving | The results showed CBT reduced the desire and risk of recurrence. |
| Yazdanbakhsh et al., 2019 (19) | Quasi-experimental study | 20 | 46 ± 15.45 | Addicts with HIV | Temperament and Character Dimensions Scale | Cognitive-behavioral group therapy | Relapse rate | |
| Forghani et al., 2021 (20) | Quasi-experimental study | 30 | 34.67 ± 8.98 | Methadone-maintenance treated patients | Luthans’s Psychological Capital Questionnaire | ACT | Psychological capital | The ACT approach had significant effect on the reduction of temptation and relapse in methadone-maintenance-treated patients |
| Forghani et al., 2021 (20) | Quasi-experimental study | 30 | 34.67 ± 8.98 | Methadone-maintenance treated patients | Wright’s Craving Beliefs Questionnaire | ACT | Temptation |
Characteristics of Included Studies
4.2. Quality Assessment of Included Studies
About 70% of the studies had a low risk of bias, and 20% had a moderate risk of bias. One article had a high risk of bias. In most studies, a clearly defined primary outcome for this report and the intervention intended for each group were not mentioned during the research, which was the biggest weakness that caused problems in the quality of the assessed studies (Table 2).
| Author, Y | Question 1 a | Question 2 b | Question 3 c | Question 4 d | Question 5 e | Result of Quality of Assessment |
|---|---|---|---|---|---|---|
| Yousefi et al., 2020 (11) | 1 | 0 | 0 | 1 | 1 | Moderate |
| Xu et al., 2021 (12) | 1 | 1 | 1 | 1 | 1 | High |
| Freisthler et al., 2021 (13) | 0 | 1 | 1 | 1 | 1 | High |
| Yeung, 2022 (14) | 1 | 1 | 1 | 1 | 1 | High |
| Mahmoudi and Ghaderi, 2017 (15) | 1 | 1 | 1 | 1 | 1 | High |
| Mansoori et al., 2019 (16) | 1 | 1 | 0 | 1 | 1 | High |
| Jalili Gholami et al., 2024 (17) | 1 | 0 | 0 | 1 | 1 | Moderate |
| Nojavan Kanmiran et al., 2021 (18) | 1 | 0 | 0 | 1 | 1 | High |
| Yazdanbakhsh et al., 2019 (19) | 1 | 0 | 0 | 1 | 1 | High |
| Forghani et al., 2021 (20) | 0 | 0 | 0 | 1 | 1 | Low |
Quality Assessment of Included Studies to Assess Risk of Bias
4.3. Social Rehabilitation and Psychological Rehabilitation in Addiction Recovery
Three main categories were identified according to interventional studies: The role of partner/significant other, emotional support, and social network. Social recovery should be viewed as a process that facilitates recovery within individuals, families, and communities, enabling them to maintain their recovery and avoid relapse after successfully overcoming drug addiction. Identifying these factors can strengthen individuals’ recovery processes and encourage successful integration into the community.
4.3.1. Role of Partner/Significant Other
4.3.1.1. Cares + Community-Based Addiction Rehabilitation
They discovered that the beneficial influence of personal relationships on recovery goes beyond just family connections. In particular, individuals with a significant other, like a partner or spouse, demonstrated notable advancements in their recovery from addiction. This approach integrates family involvement (e.g., care sessions) to strengthen communication and parenting skills, addressing systemic barriers like housing and employment (12).
4.3.1.2. Network Support (e.g., Peer Recovery Supporters)
It is important for patients to be involved in a supportive network and social participation. This approach explicitly connects participants with recovery-oriented social networks, reducing ties to substance-using peers and fostering accountability. The study conducted by Freisthler et al. (2021) in Ohio focused on the significance of social networks in the addiction recovery process (13).
4.3.1.3. Behavioral Couples Therapy (Implied in "Family Treatment Drug Court")
This therapy improves relationship dynamics and reduces enabling behaviors, though it is not explicitly listed in the provided interventions. Freisthler et al. (2021) showed that this intervention establishes formal collaboration across child welfare, behavioral health, and juvenile courts to assist families impacted by addiction. The implementation of three evidence-based or evidence-informed strategies creates an opportunity to identify the most effective methods for reducing the severity of addiction. Additionally, this intervention incorporates multiple funding sources to enhance sustainability beyond the duration of the Regional Partnership Grant (13).
4.3.2. Emotional Support
4.3.2.1. Acceptance and Commitment (Group) Therapy
According to the included studies, acceptance and commitment therapy (ACT) is a highly effective technique for psychological intervention in addiction recovery (15, 16, 19). This psychological intervention enhances emotional regulation through mindfulness and value-driven actions, fostering self-compassion and resilience in group settings. Yazdanbakhsh et al. (2019) showed that cognitive behavioral therapy (CBT) significantly reduced cravings and the risk of relapse compared to the control group (P < 0.001). These findings highlight the importance of incorporating psychological therapy alongside traditional drug treatments to address addiction (19). Furthermore, Mahmoudi and Ghaderi (2017) showed that ACT effectively reduced stress and anxiety but did not significantly affect depression. The authors recommend using additional therapies alongside ACT and suggest further research on its long-term effects (15). Mansoori et al. (2019) studied the impact of self-knowledge-based group counseling on assertiveness in male addicts at Razi Psychiatric Hospital in Tehran. Thirty male participants were randomly assigned to experimental and control groups. The experimental group attended ten sessions focused on self-recognition. Results showed significant improvements in self-expression for the experimental group (P < 0.01), demonstrating the effectiveness of this counseling approach in aiding rehabilitation (16).
4.3.2.2. Compassion-focused Therapy
Compassion-focused therapy (CFT) targets shame and self-criticism, building emotional resilience through self-compassion practices and soothing-system activation. Nojavan Kanmiran et al. (2023) explored the effectiveness of compassion-based therapy on improving the lifestyle and emotional processing of opioid-dependent addicts in the non-drug rehabilitation phase. Utilizing a quasi-experimental design with a control group, the research involved 30 adolescents. Results indicated that compassion therapy significantly enhanced various lifestyle components and emotional processing, leading to improved physical and psychological health while reducing emotional suppression and avoidance. Therefore, the therapy appears beneficial for addicts seeking recovery (18).
4.3.2.3. Cognitive-Behavioral Therapy (Including Michael Frisch’s QOLT)
This technique addresses maladaptive thought patterns (e.g., “I’m unworthy”) and teaches coping strategies to manage emotional triggers. The findings of Jalili Gholami et al. (2024) indicated that Michael Frisch’s CBT enhances the cognitive well-being of individuals seeking addiction treatment. Psychological well-being is a crucial factor in assessing quality of life. The CBT emphasizes an individual’s achievements and strengths, which boosts self-efficacy and promotes greater success. Additionally, this therapy teaches effective coping strategies to manage stress, empowering individuals to take responsibility for their actions and reinforcing their sense of accountability (17).
4.3.3. Social Network Reinforcement
4.3.3.1. Matching Participants with Peer Recovery Supporters
Freisthler et al. (2021) demonstrated that utilizing lived experiences can help diminish isolation, exemplify recovery behaviors, and foster community support networks, with a primary goal of assisting parents in accessing treatment. Peer recovery supporters offer a range of services, including thorough clinical assessments, service planning, referrals, advocacy, case management, and outreach efforts (13).
4.3.3.2. Group Counseling (Self-recognition Sources)
This approach utilizes peer interactions to normalize recovery experiences, enhance social skills, and foster collective accountability. Mansoori et al. (2019) showed that a lack of self-expression heightens the inclination toward substance use, and therapy focused on sources of self-recognition is a relatively new approach that can effectively enhance self-expression. Psychological rehabilitation grounded in self-recognition improves self-esteem and enhances social communication skills while promoting respect for the rights of others (16).
4.3.3.3. Cognitive-Behavioral Group Therapy
This therapy combines CBT techniques with group dynamics to improve interpersonal functioning and social confidence. The findings from Yazdanbakhsh et al.’s 2020 study highlighted the significance of cognitive-behavioral group therapy in reducing cravings and relapse among individuals with HIV who are addicted. Consequently, considering the crucial role of complementary drug therapies, psychological therapy may help address psychological issues related to addiction (19).
4.3.3.4. Interventions Spanning Multiple Categories
4.3.3.4.1. Secular-Based Treatment (Biopsychosocial Model)
This model integrates social (environmental determinants), emotional (psychological interventions), and network (community resources) components through holistic care. The study by Yeung (2022) examined the impact of religiosity on substance abuse abstinence among recovering addicts in faith-based versus secular treatment programs. By measuring religiosity at treatment initiation, discharge, and six months later, the research found that those in faith-based programs showed greater levels of religiosity and religious development, which contributed to better post-treatment abstinence. The findings underscore the significance of understanding how religiosity evolves during recovery and its role in sustaining sobriety after treatment (14).
4.3.3.5. Acceptance and Commitment Therapy
While primarily psychological, its group format indirectly strengthens social networks through shared experiential exercises. Yousefi et al. (2020) performed a study aiming to reduce impulsivity in individuals with methamphetamine use disorder through ACT. It demonstrates that ACT, an innovative approach in the third wave of behavioral therapy, serves as an effective intervention for decreasing impulsive behaviors in these patients (11). Furthermore, Forghani et al. (2021) showed that the ACT approach had a significant effect on the reduction of temptation and relapse in methadone-maintenance treated patients (20).
4.4. Results of the Meta-Analysis on the Effect of Psychological Rehabilitation on Addiction Recovery
The pooled standardized mean difference (SMD) is 1.25, but its 95% confidence interval (-0.576 to 3.086) includes zero, indicating that the overall effect is not statistically significant (P = 0.179). Heterogeneity is extremely high (I2 = 95.8%, Tau2 = 6.4263), reflecting substantial differences across study outcomes. Some studies, like Yazdanbakhsh et al., demonstrate strong positive effects (SMD ≈ 6.8), while Mansoori et al. (2019) reported a significant negative effect (SMD = -5.8) (16, 19). Recent studies, such as Forghani et al. (2021), showed trivial or non-significant effects. To identify sources of heterogeneity, subgroup analysis will categorize studies based on characteristics, while meta-regression will examine relationships between continuous variables and treatment effects (20).
4.4.1. Subgroup Analysis
To reduce heterogeneity, a subgroup analysis was conducted based on the variable "type of psychological rehabilitation for addiction recovery". The results indicated different patterns of heterogeneity and effectiveness among the therapeutic approaches. Moreover, the marked difference in Tau2 between CBT and CFT (25.86 vs. 0) suggests that heterogeneity in CBT is likely due to conceptual factors rather than statistical errors. It is therefore recommended that qualitative synthesis be used for CBT instead of quantitative analysis. In ACT, heterogeneity was very high (I2 = 90.8%), and the pooled effect was not significant (P = 0.447). The CBT also showed heterogeneity at a critical level (I2 = 97.3%), with a non-significant pooled effect (P = 0.550). In CFT, no heterogeneity was observed (I2 = 0%), and there was a strong, statistically significant pooled effect (P < 0.001).
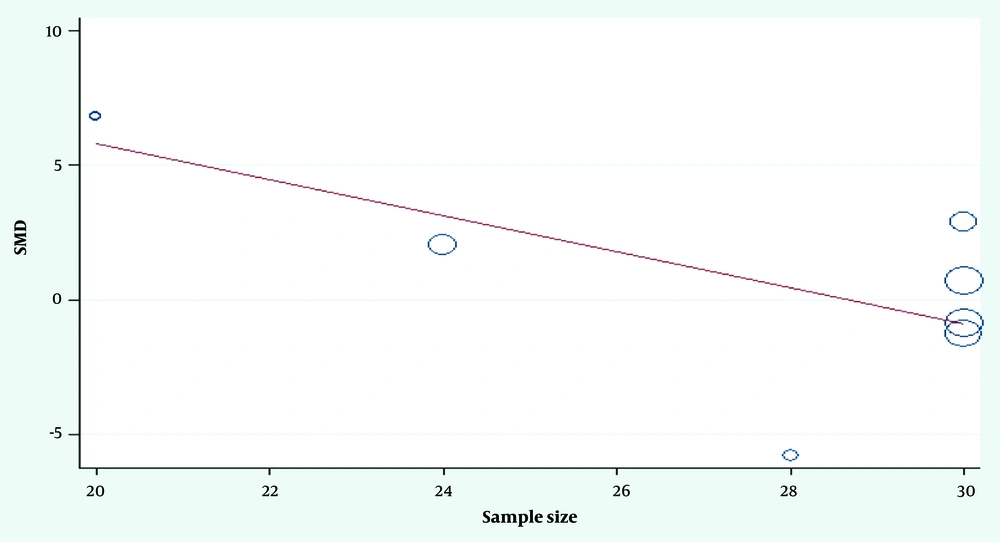
4.4.2. Meta-Regression
According to the meta-regression results, there is a relationship between SS and ES: The coefficient for SS is -0.668, which is statistically significant (P = 0.047). This indicates a negative relationship between SS and ES. In other words, studies with larger SS tend to report smaller ES. The value of I-squared is 94.65%, indicating that even after accounting for the effect of SS, there remains substantial heterogeneity among the studies. In summary, the meta-regression results show that SS is significantly associated with ES, but considerable heterogeneity between studies still exists that cannot be explained by SS alone (Figure 2).
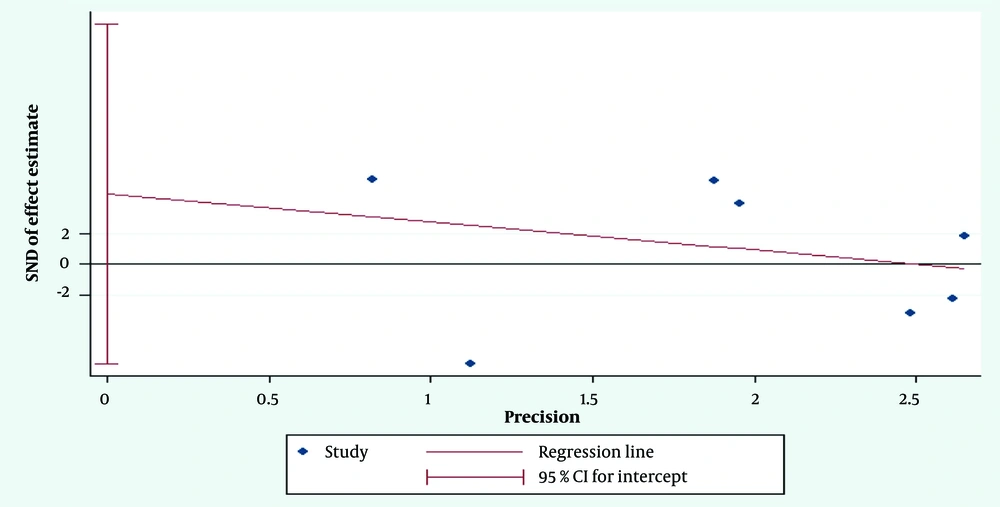
4.4.3. Publication Bias
The P-value obtained from Egger’s test is 0.350. Since this value is greater than the conventional alpha level of 0.05, the null hypothesis of no small-study effects cannot be rejected. According to the result of Egger’s test, there is insufficient evidence for publication bias or small-study effects in this meta-analysis. In other words, the results of this meta-analysis are unlikely to be influenced by small studies with unrealistically positive findings (Figure 3).
5. Discussion
The results of this study highlight the crucial role of both social and psychological rehabilitation in addiction recovery. Three main categories emerged from the analysis of interventional studies: The involvement of partners or significant others, emotional support, and the broader social network. Recent research consistently underscores that social support systems are among the most important factors in initiating and sustaining recovery from SUDs. Belonging to a supportive social network significantly predicts sustained remission and reduces the risk of relapse.
In recent years, innovative approaches in addiction treatment and rehabilitation, with an emphasis on social empowerment and psychosocial support, have played a significant role in the sustained recovery of individuals overcoming addiction. Comprehensive rehabilitation programs, in addition to pharmacological treatment and psychotherapy, focus on life skills training, family support, vocational training, and the creation of employment opportunities for individuals in recovery, thereby facilitating successful reintegration into society and preventing relapse. Research indicates that the quality of family functioning and the level of social support are significantly associated with reduced high-risk behaviors and increased success in addiction cessation (21, 22).
Furthermore, the use of novel interventions such as compassion-based therapies, group therapy, family therapy, and leveraging the capacity of non-governmental organizations and social entrepreneurs can enhance self-esteem, reduce feelings of loneliness, and increase motivation to maintain recovery (22, 23). However, individual differences, social circumstances, and access to supportive services continue to influence the effectiveness of these interventions, highlighting the need for personalized programs and ongoing monitoring of treatment outcomes (21-23).
Social recovery should be viewed as an ongoing process that facilitates recovery not only for individuals but also for families and communities, empowering them to maintain recovery and prevent relapse after overcoming addiction. Community-based recovery support, such as participation in sober active communities and mutual-help organizations, has been shown to foster positive changes in social networks and support the development of a "recovery identity". These social environments provide emotional, instrumental, and informational support, which are critical for long-term recovery (24).
Moreover, the role of significant others and partners cannot be overstated. Studies demonstrate that individuals who receive support from mentors, peers in recovery, and family members experience greater success in maintaining sobriety. Emotional support, in particular, helps buffer stress and promotes psychological well-being, further strengthening resilience against relapse (25). Emotional resilience, fostered by these supportive relationships, is a key factor in reducing relapse risk and enhancing long-term recovery outcomes (25, 26).
Despite the growing body of evidence supporting social and psychological rehabilitation, challenges remain. The heterogeneity among studies is very high (I2 = 95.8%, Tau2 = 6.4263), likely due to differences in intervention methods, sample characteristics, and measurement tools. Although some evidence suggests positive effects, overall psychological rehabilitation does not show a statistically significant impact on addiction recovery skills. Subgroup analyses revealed inconsistent results for ACT interventions, highlighting the need to clarify key concepts like "acceptance" and "committed action". The CBT studies showed high variability, possibly due to differences in session content, duration, or therapist experience.
While overall psychological rehabilitation did not show a statistically significant impact on addiction recovery, specific interventions — particularly CFT — demonstrated a strong and significant effect. This suggests that the effectiveness of psychological rehabilitation may depend on the type of intervention used. Future research should focus on standardizing protocols, improving study designs, and identifying factors that explain these variations (27). High heterogeneity in intervention outcomes suggests that individual and contextual factors influence the effectiveness of these approaches. Future research should focus on identifying the specific characteristics of social ties that yield the most support and on developing tailored interventions that address the unique needs of diverse populations (27, 28).
One of the main limitations of this meta-analysis was the substantial heterogeneity and imprecision among the included studies, which resulted in a wide confidence interval and lack of statistical significance for the pooled effect. Therefore, the overall ES should be interpreted with caution (29).
5.1. Conclusions
In conclusion, strengthening social networks and integrating psychological rehabilitation are essential strategies for addiction recovery. Identifying and leveraging the roles of partners, emotional support, and social networks can enhance recovery processes and facilitate successful reintegration into the community. As innovation in addiction treatment continues in 2025, combining evidence-based psychological therapies with robust social support systems will be key to improving long-term outcomes for individuals recovering from addiction (25).