Dear Editor,
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease of unknown etiology, characterized by symmetric peripheral polyarthritis. The disease is characterized by increased immune and inflammatory responses due to a complex interaction between genes and environment, which leads to accumulation of immune cells in the synovial tissue, causing matrix destruction and damage to bone and cartilage (1). Both B and T cells as well as monocytes can be seen with increasing tendency with the disease progression. The pathogenesis of RA is built upon the concept that self-reactive antibodies and T cells drive the chronic inflammatory response. T cells are activated and thus they proliferate and release cytokines. B Cells produce rheumatoid factor immunoglobulin M (IgM) and other antibodies. Monocytes produce pro-inflammatory cytokines such as interleukin 1 (IL-1), interleukin 6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which induce proliferation and activation of the synovium tissue (2, 3). Furthermore, prostaglandin E2 (PGE2), collagenase and other matrix metallo-proteinases are released (3). All the mechanisms of the disease and complications of its treatment can reduce patients’ quality of life and cause psychiatric diseases and sleep disorders, leading to patient dissatisfaction (4).
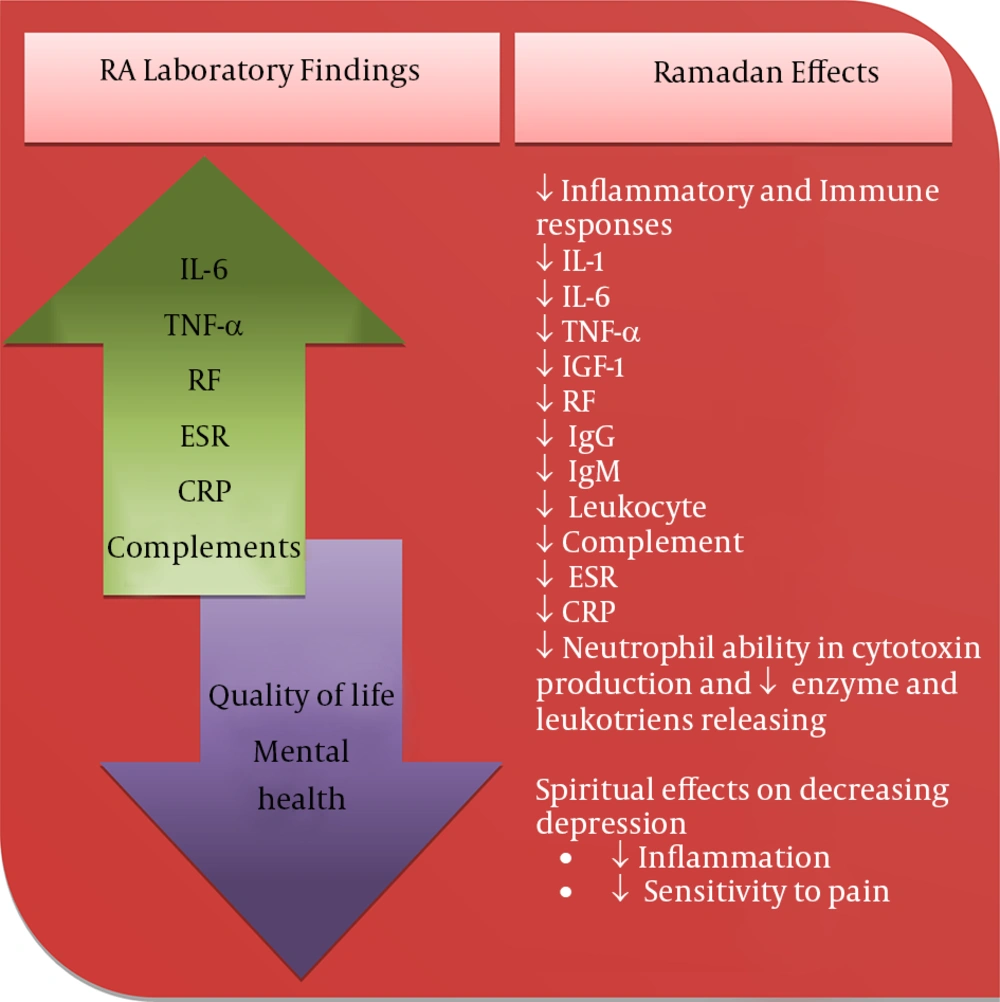
Some studies showed that fasting decreases the immune and inflammatory responses and affects both hormonal and cellular immune responses (1, 5, 6). Fasting decreases the serum concentration of TNF-α (1, 7), IL-1 (1), IL-6 (1, 7), insulin-like growth factor 1 (IGF-1) (7), rheumatoid factor (RF), IgM and immunoglobulin G (IgG) (8), leukocytes and leukotrienes (1), complements (8, 9), and the ability of neutrophils to produce cytotoxic metabolites and release enzymes (9). Fasting also decreases the erythrocyte sedimentation rate (ESR) (10) and C-reactive protein (CRP) (10). Figure 1 shows schematic laboratory findings of RA and Ramadan fasting effects on inflammatory and immune responses (Figure 1).
Ramadan is the ninth month of the Islamic lunar calendar and consists of 29-30 days. Muslims fast the whole Ramadan. Ramadan fasting implies the total abstinence from food ingestion and drinks from sunrise to sunset. Perhaps, more important is the positive effects of the general atmosphere during Ramadan on spiritual and mental health. Reciting Quran, praying during night, donating money and helping the needy, being thoughtful and watchful, and exercising restraints on soul and body may all contribute positively to mental health and quality of life of both healthy sick people, including those with RA (2, 3). It was also reported that Ramadan fasting was effective on diminishing stress and depression levels (4).
We hypothesized that Ramadan fasting may decrease the signs and symptoms of patients with RA. As such, fasting may be recommended as a complementary treatment to reduce both dosage and side effects of the conventional anti-inflammatory and immunosuppressive drugs. However, this hypothesis requires further concrete research for validation. On the other hand, by the same mechanism of regulating the immune system, it can be hypothesized that fasting can be effective on all autoimmune disease.
.jpg)