1. Background
Patellofemoral pain syndrome (PFPS) is one of the most common disorders affecting the lower extremities. It frequently occurs among the physically active population, with a higher incidence in women (1). The most common reason for PEPS is overuse (1). It is theorized that impaired gluteal muscle function may result in increased hip joint adduction and internal rotation movement during activities such as running, squatting, and descending stairs (2). This excessive hip motion is proposed to increase the lateral patellofemoral joint stress associated with PFPS development (2). Supporting this theory, gluteal muscle strengthening programs have been associated with a positive clinical outcome in individuals with PEPF (3-8). In addition, recent systematic reviews have found that women with PFPS demonstrated reduced strength of the gluteus medius (Gmed) and gluteus maximus (Gmax) on the affected side compared to those on the asymptomatic side (9, 10). All lower extremity joints and muscular forces are interconnected, and a weakness in any of the elements can affect the entire chain. Any underlying muscular weakness needs to be addressed to prevent further injury that is caused by the functional movements. Therefore, weight-bearing exercises are preferred, as they better mimic the functional movements during muscle strengthening of the lower extremities (11).
Electromyography (EMG) could be used to assess the activation of a muscle, as measured by the electrical activity levels in the muscle. A general consensus is that exercises that produce higher levels of activation in the muscles are most suitable for strengthening (12). It has been proposed that the minimum effort required to obtain a strengthening stimulus from the muscle is approximately 40-60% of the maximal voluntary isometric contraction (MVC). A muscle activity of less than 25% MVC indicates that the muscle is functioning in an endurance capacity or to maintain stability (12). Additionally, to classify low and high muscle activities, a previous study categorized 0% to 20% MVC as “low” muscle activity, 21% to 40% MVC as “moderate” muscle activity, 41% to 60% MVC as “high” muscle activity, and greater than 60% MVC as “very high” muscle activity (13). Numerous authors have attempted to quantify Gmed and Gmax activation during a wide variety of hip abduction, external rotation, and extension exercises (14-21). A systematic review demonstrated that EMG activity for Gmed ranged from 12 to 103% MVC and Gmax ranged from 4 to 113% MVC during hip abduction and hip external rotation exercises (21). EMG activity can be affected by changes in body position and complexity of the exercise (14-21). These studies provide an indication for the amount of muscle activity generated by basic strengthening and rehabilitation exercises, which may assist practitioners in making decisions for Gmed and Gmax strengthening and injury rehabilitation programs. When strengthening a weaker muscle, practitioners may wish to prescribe a gradual and progressive exercise program to ensure the targeted area is developed. This may be of importance if individuals implement a compensatory movement pattern when faced with weakness or dysfunction (21).
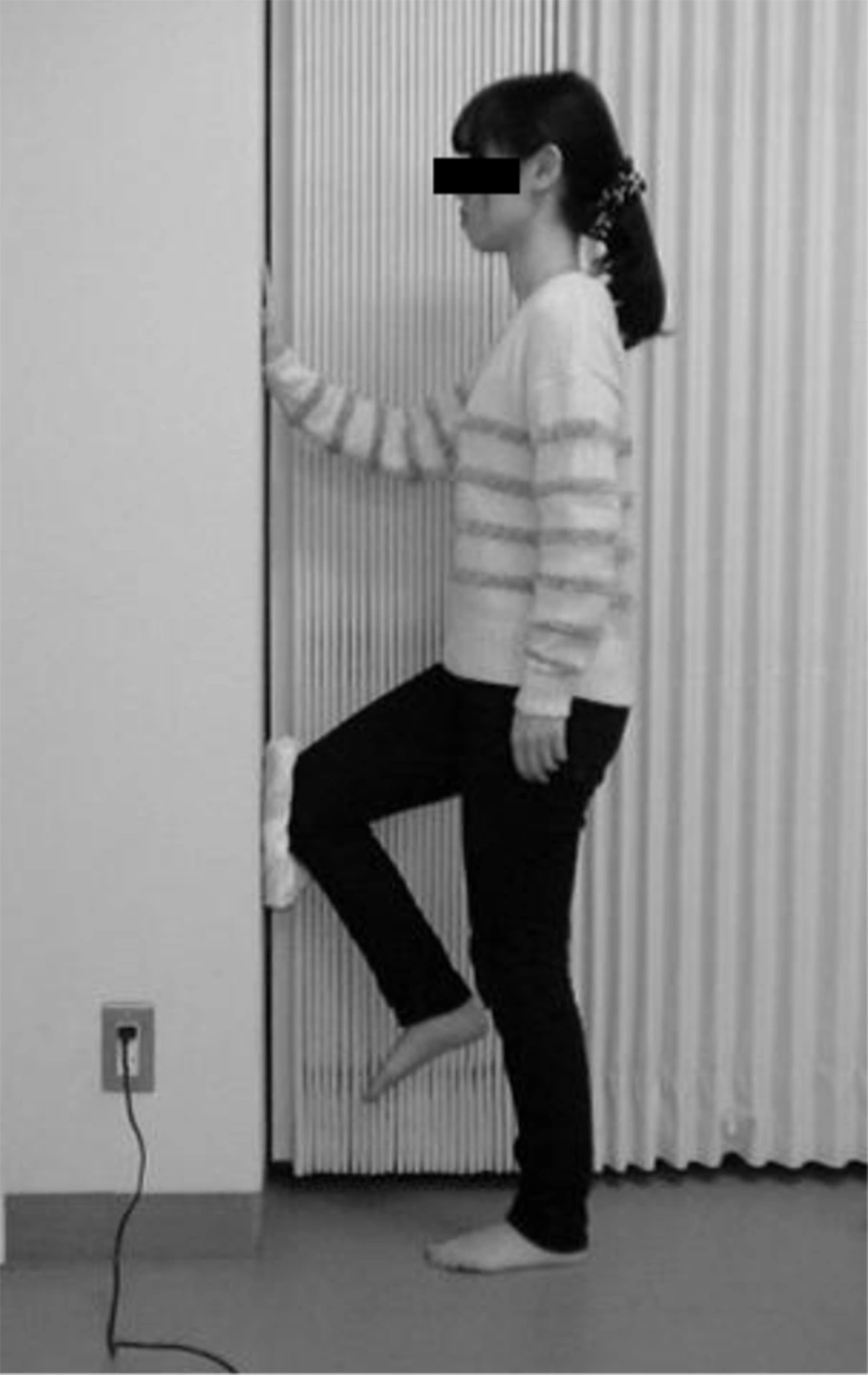
Lateral wall press (WP) exercise is one of the weight-bearing exercises of the gluteal muscle strengthening programs (Figure 1) (3). This exercise requires the hip on the weight-bearing side to maintain relative hip abduction despite the creation of an addiction torque by the opposite knee pushing laterally against the wall (14). O’Sullivan et al. (14) demonstrated that the lateral WP exercise is an effective isometric strengthening exercise for Gmed using EMG. However, little is known about the activity level of Gmax on the weight-bearing side during the lateral WP exercise. The primary actions of the Gmax muscle are hip extension and hip external rotation (17), and the superior area of the Gmax also functions as a hip abductor (22). We considered that the frontal WP exercise could require the hip on the weight-bearing side to maintain a relative hip extension despite the creation of a flexion torque by the right knee pushing forward against the wall (Figure 2). We hypothesized that not only lateral but also frontal WP exercise might induce high EMG activity in the Gmax.
2. Objectives
The purpose of this study was to quantify the EMG activity of the Gmax on the weight-bearing side during lateral and frontal WP exercises.
3. Patients and Methods
3.1. Participants
Twelve healthy women (university students) participated in this study. Their age, height, and weight (Mean ± SD) were 20.3 ± 0.5 years-old, 158.1 ± 3.6 cm, and 51.5 ± 4.3 kg, respectively. All participants were right-handed. None of them had a history of limb surgery or neuromuscular disorders. The study was explained to the subjects, whose verbal consent was obtained prior to their participation.
3.2. Procedure
The surface EMG was conducted using the MQ8 system (Kissei Comtec, Japan). Skin preparation of the electrode sites involved cleansing with alcohol. Disposable silver/silver chloride surface electrodes with a recording diameter of 1 cm (Blue Sensor P-00-S, Ambu, Denmark) were used. The used surface EMG electrodes were self-adhesive. The EMG signal of the left superior area of the Gmax was recorded. Electrode placement was based on a previous study (23). The bipolar electrodes for the Gmax were placed halfway between the sacrum and greater trochanter. The inter-electrode distance from center to center was 25 mm. A ground electrode was placed over the anterior superior iliac spine.
During the WP exercise, the subjects were asked to assume a left single leg stance position by flexing their right hip to 60 degrees and their right knee to 90 degrees using goniometric measures (Figures 1 and 2) (14). The subjects were allowed to touch the wall with their right hand to maintain balance. For the lateral WP exercise task, the participants were asked to push against the wall using the lateral side of their right knee. For the frontal WP exercise task, the participants were asked to push against the wall using the frontal side of their right knee. During both the exercises, a towel was inserted between their right knee and the wall to prevent knee pain. They were then asked to maintain these positions while concurrently pushing their right knee against the wall with maximum strength. For the lateral and frontal WP exercises, they were asked to push maximally laterally and frontally, respectively. They were specifically told not to contract their gluteal muscles on the weight-bearing side. The subjects kept their trunks in a vertical alignment to their pelvis throughout the exercise. They maintained isometric contraction for 5 seconds during each trial. Prior to testing, they performed three practice trials of each exercise for familiarization. During the trial, any subject performance errors, including pelvic rotation or twisting, were corrected (14). They performed three repetitions of each exercise, with a 30 seconds rest period between the trials and 60 seconds rest period between the exercises to reduce the possibility of fatigue (14). The order of the exercises was randomized. The EMG signals, which were recorded for 5 seconds while holding each trial of exercise, were amplified, band-pass filtered (10-500 Hz), and full-wave rectified. The average values of muscle activities over the 5 seconds sample of the three trials performed for each of the two exercises were normalized to the MVC, which was obtained in the isometric maximal exertion tasks, using a standard manual muscle test described by Hislop et al. (24). The MVC was held for 5 seconds and the average of EMG activity obtained for Gmax was used to determine the MVC. The percent MVC values of the three trials performed for each of the two exercises were averaged and used in the statistical analysis.
3.3. Statistical Analysis
IBM SPSS Statistics 22 was used for all statistical analyses. The paired t-test was used to examine the significance of differences in the Gmax muscle activities between the lateral and frontal WP exercises. Differences were considered statistically significant at values of P < 0.05. The G-Power software (Franz Faul, Univesitat Kiel, Germany) was also used to calculate the post-hoc effect size and actual power of the sample.
4. Results
The Mean ± SD of the averaged EMG during the lateral and frontal WP exercises were 40.1 ± 19.1, and 23.7 ± 11.3 µV, respectively. The averaged EMG of the Gmax during the lateral WP exercise was significantly higher than that during the frontal WP exercise (P = 0.001, 95% confidence interval = 8.1-24.8, effect size = 1.25, power = 0.98).
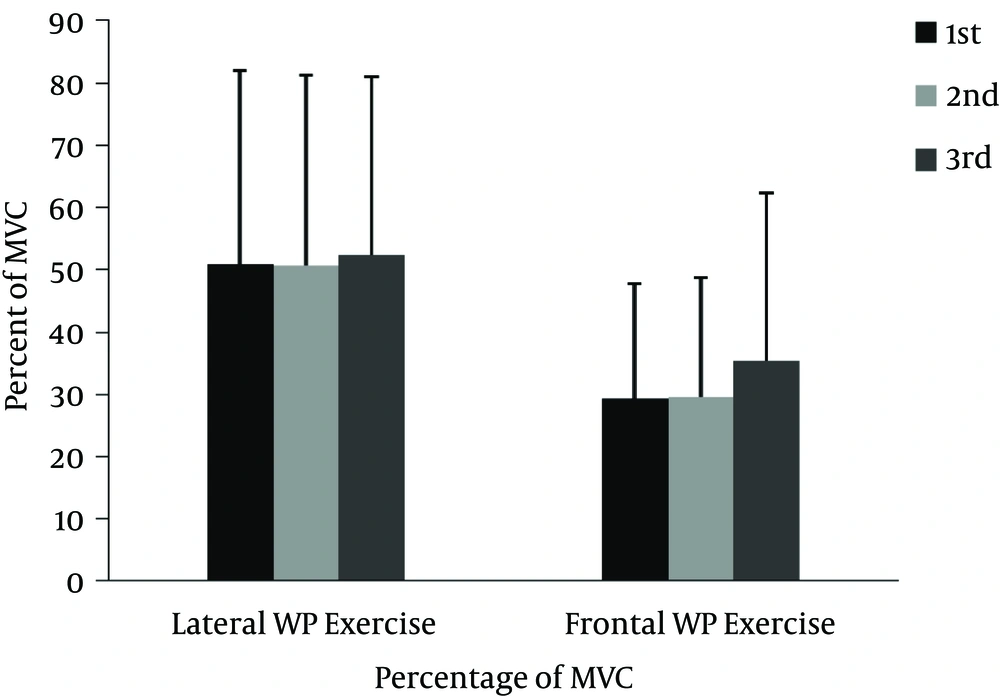
The percent MVC of the Gmax for each of three attempts during the lateral and frontal WP exercises was showed in Figure 3. The Mean ± SD of the percent MVC of the Gmax during the lateral and frontal WP exercises were 51.4 ± 29.7, and 31.3 ± 20.5, respectively. The percent MVC of the Gmax during the lateral WP exercise was significantly higher than that during the frontal WP exercise (P = 0.001, 95% confidence interval = 10.5 - 29.7, effect size = 1.33, power = 0.99).
5. Discussion
To the best of our knowledge, this study is the first to quantify the EMG activity of the Gmax on the weight-bearing side during lateral and frontal WP exercises. Our results show that lateral and frontal WP exercises induce “high” and “moderate” muscle activity of Gmax, respectively (13). The intensity of the Gmax activity during the lateral WP exercise may be suitable for providing strength (12). There are various Gmax strengthening exercises, and details of intensity of the Gmax activity during those exercises were reported in a systematic review (21). For example, the intensity of the Gmax activity during the lateral WP exercise was similar to that during the lateral step up (49.6% MVC) and transverse lunge (53.5% MVC), which are classified as Gmax high-activity exercises (21). By knowing the Percent MVC of the Gmax that occurs during various exercises, potential for strengthening of the Gmax can be inferred (15). Additionally, exercises may be rank ordered to appropriately challenge the Gmax during rehabilitation.
A study reported that the hip strength of abduction was lower compared to that of flexion (25). The difference in the Gmax activity between the lateral and frontal WP exercises might be related to not only the creation of an addiction or flexion torque of the hip on the weight-bearing side by pushing the opposite knee laterally or frontally against the wall, respectively, but also to the requirement of the hip external or internal rotation during the exercises. To maintain balance, a relative hip external rotation was required in the lateral WP exercise, whereas, a relative internal rotation was required in the frontal WP exercise. The primary actions of the Gmax are hip extension and hip external rotation (17), and the superior area of the Gmax also functions as a hip abductor (22). In this study, activity in the superior area of the Gmax was detected using EMG. To maintain relative hip abduction and external rotation during the lateral WP exercise, a higher activity of Gmax might be elicited compared to that elicited during the frontal WP exercise. Our results indicate that the lateral WP exercise is more suitable for strengthening the Gmax on the weight-bearing side than is the frontal WP exercise.
We recognize several limitations of our study, including the use of healthy subjects and not recording the subjects’ hip joint movements during the exercises. Our participants were healthy, thereby limiting the generalization of our findings to individuals with reduced hip muscle performance. Additional research must be conducted in populations with PFPS to increase the clinical applicability of our findings. Before data collection, the subjects were trained to perform the lateral and frontal WP exercises by the same investigator. However, we did not record hip joint movements during the exercises. Thus, we cannot claim that the exercise position was uniform across the subjects. Further investigation is necessary to clarify the activity level of the Gmax during the lateral and frontal WP exercises in PFPS individuals. In conclusion, the subjects only performed the WP exercise in this study. Future studies should investigate exercises other than the WP exercise to examine Gmax activity and to generalize the findings.