1. Context
Scoliosis is a three-dimensional deformity of the spine and trunk which includes lateral deviation, rotation, and a disturbance of the sagittal profile (1-4). Scoliosis treatment is indicated because scoliosis may lead to negative consequences with regard to the quality of life and other health issues for some patients (1, 5, 6). Scoliosis may be caused by disturbances of the neuromuscular system (neuromuscular scoliosis), alterations of the soft tissue (e.g. Marfan’s syndrome and Ehlers Danlos syndrome), alterations of the nervous system (neurofibromatosis), failures in the formation/segmentation of the vertebrae and ribs (congenital scoliosis), and many others (7). The majority of patients with scoliosis have idiopathic scoliosis (8, 9), and rarely, early onset scoliosis (EOS) (6, 7). Late onset idiopathic scoliosis, also called adolescent idiopathic scoliosis (AIS) is diagnosed in 80% - 90 % of the total population with scoliosis (10, 11).
Untreated symptomatic or syndromic scoliosis, as well as EOS, can sometimes cause severe health problems and higher mortality. However, AIS, the most common form of scoliosis, is relatively benign, and does not generally lead to severe health problems or early death (4, 5, 12).
A 50-year follow-up of untreated patients with AIS has shown that this population functions well. There were no more health problems in this group when compared to patients without scoliosis, other than a slight increase in back pain and cosmetic concerns (5). The indications for treatment rely largely on the Cobb angle (13), the angle of curvature as measured on an X-ray of the spine in the frontal plane. Historically the treatment of scoliosis consists of:
- Physical rehabilitation (15 - 25° Cobb)
- Brace treatment (20 - 40° Cobb)
- Spinal fusion surgery (> 40 - 50° Cobb) (1).
Two recent Cochrane reviews have shown that evidence for surgery is limited (14, 15), and currently, there is no proof that surgery would change the signs and symptoms of scoliosis over the long-term. Some authors have even concluded that in patients with AIS there is no actual indication for spinal fusion surgery (16, 17). The established medical indications and the evidence supporting surgery should be under as much scrutiny as those supporting conservative treatments. Therefore, the purpose of this review was to gather current and available information, and to search the recent articles on scoliosis for the evidence they provide for the different modes of treatment.
2. Evidence Acquisition
For this study, a PubMed search for review articles, prospective controlled trials (PCT) with an untreated control group, and randomized controlled trials (RCT) was performed. Retrospective papers were only included when long-term results were published with a follow-up time exceeding 10 years. The literature cited in the reviews has also been checked with respect to the available abstracts. When the abstract seemed to include the topic, a full paper review was performed, and in a few cases when these were not available on PubMed, a hand search was completed. The search terms included:
- Scoliosis, treatment (12,045 items found)
- Scoliosis, physiotherapy (776 items found)
- Scoliosis, brace treatment (1,447 items found)
- Scoliosis, surgery (10,485 items found)
3. Results
The results of our search have been summarized in Table 1.
| RCT/Meta-Analysis | Cochrane Review | PCT | |
|---|---|---|---|
| Physical rehabilitation | 5 | 1 | 1 |
| Brace treatment | 1 | 1 | 1 |
| Scoliosis surgery | NA | NA | NA |
Abbreviation: NA, not available.
aNo high level evidence (Level I and II) has been found supporting spinal fusion surgery. The numbers indicate the quantity of papers found in the various columns of the table.
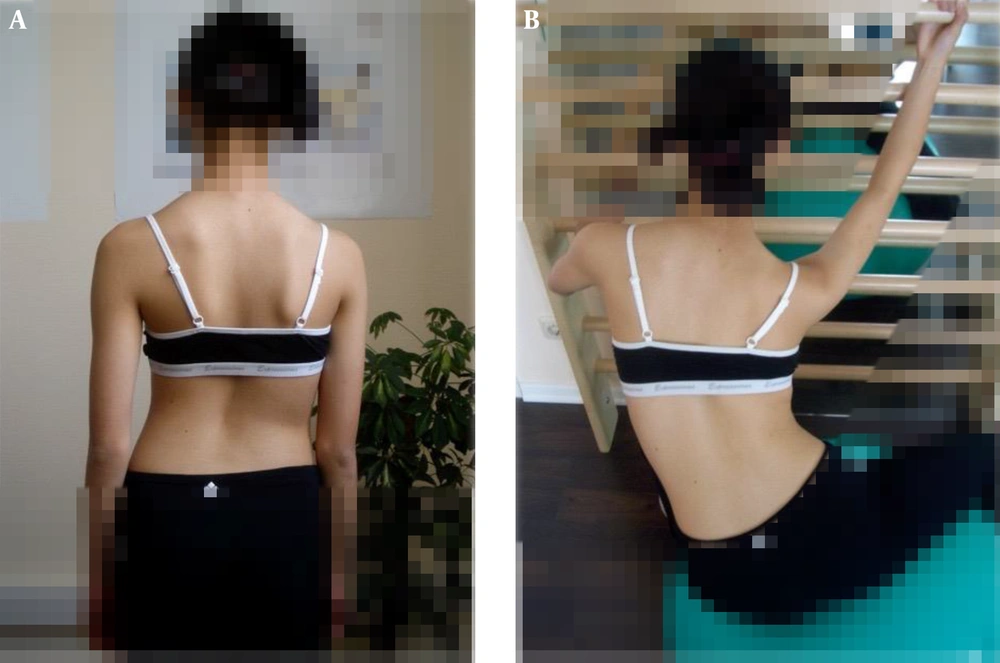
With regard to evidence for physical rehabilitation (physiotherapy, Figure 1), one meta-analysis (18), four RCTs (19-22), and one PCT (23) with an untreated control group were found supporting physiotherapy. Previously, a Cochrane review was published showing that there was little evidence for physiotherapy/physical rehabilitation at the time the review was performed (24).
Furthermore, no studies have been included that lack treatment indications as discussed in a critical review (25). Long-term retrospective studies have not been found supporting physiotherapy. Some evidence has been found for general exercises (22); however, specific correction exercises (Schroth, Side Shift, and Monticone) have been shown to be superior to exercises without a curve pattern specific exercise routine (e.g., Yoga, SEAS, Dobomed, and Clear) (19-21).
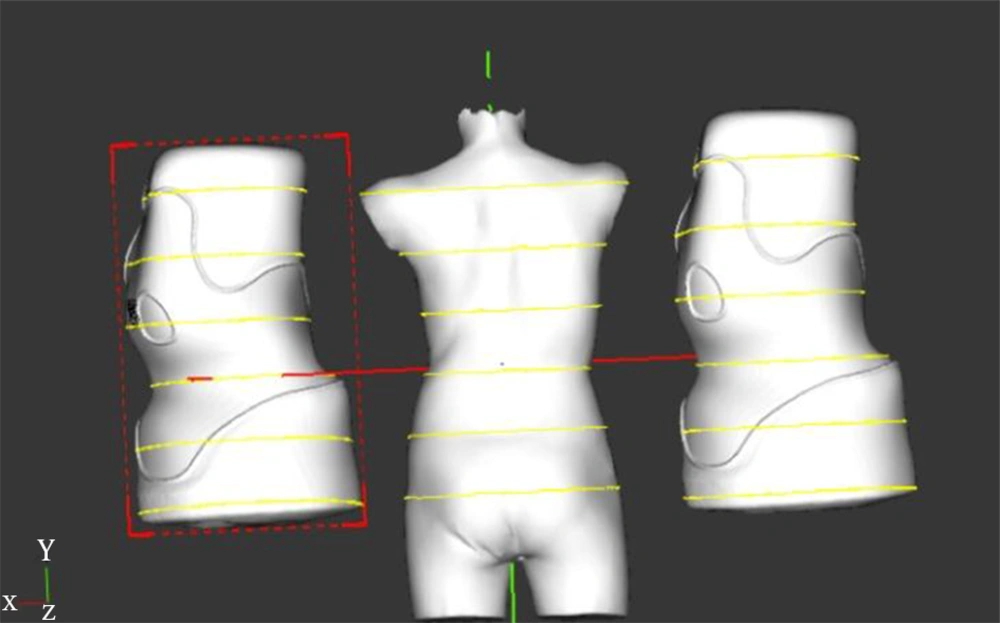
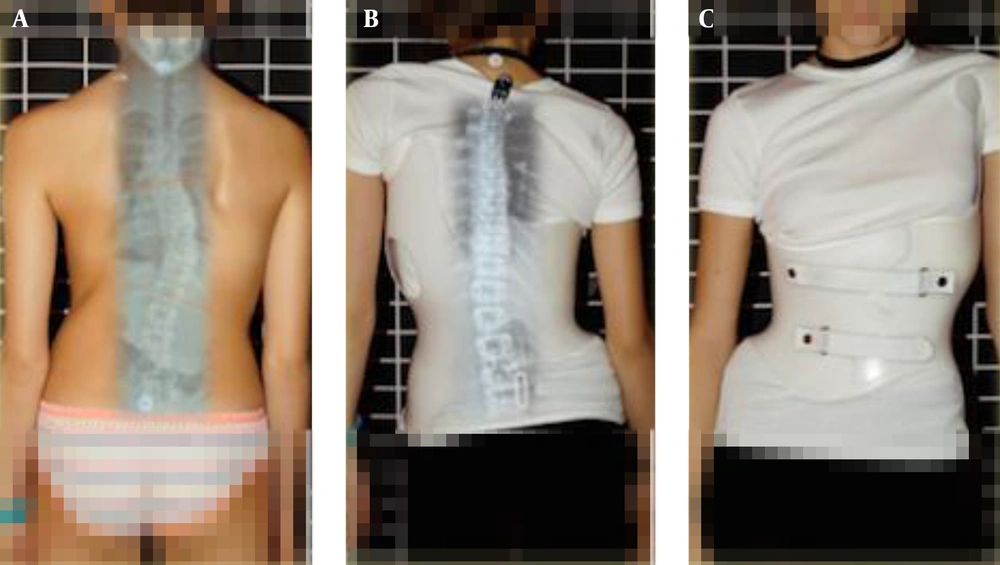
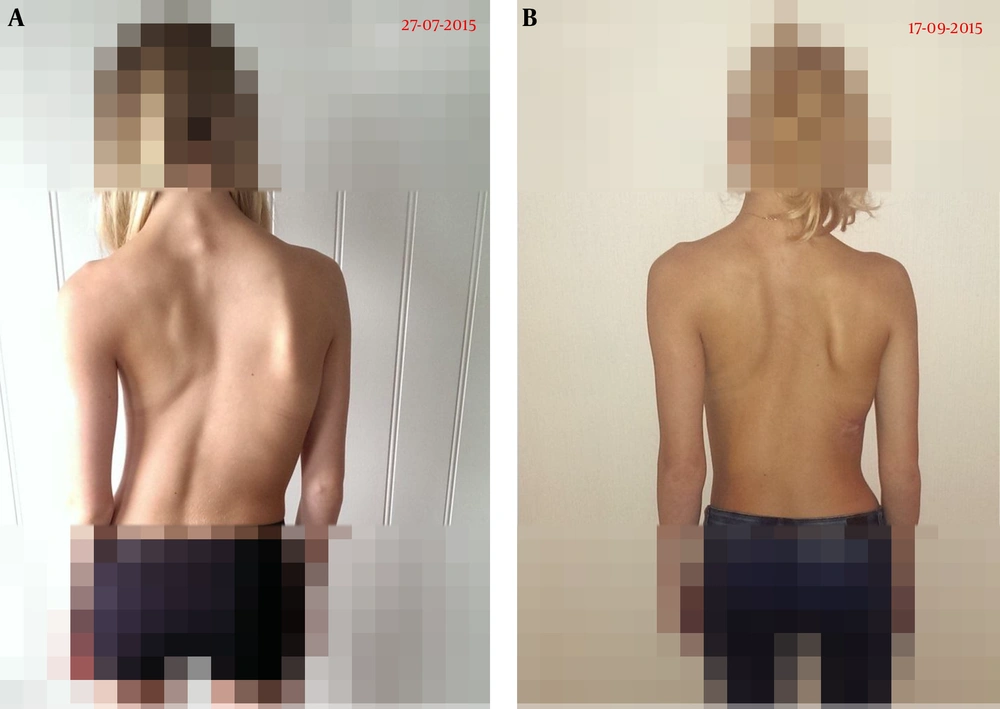
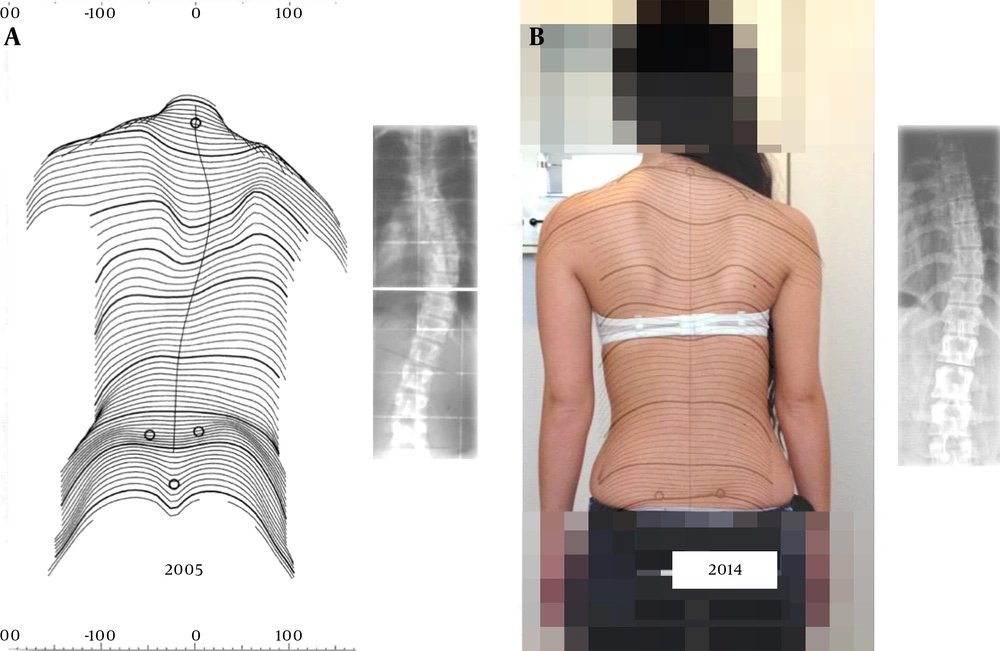
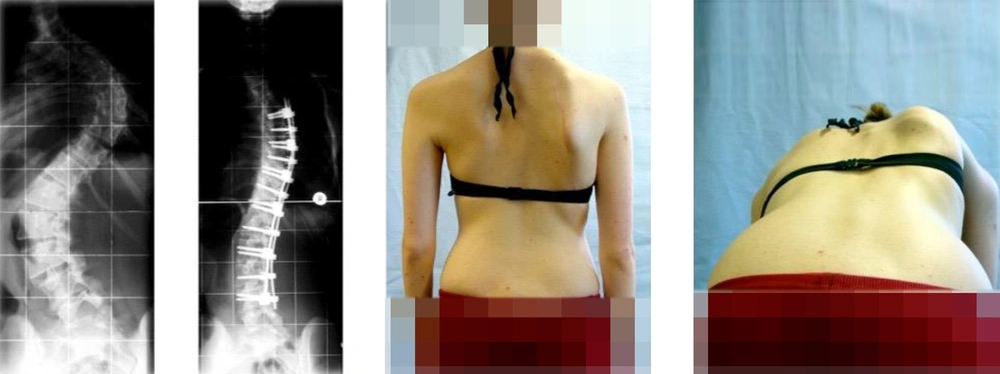
With regard to evidence for bracing (Figures 2 - 5), one meta-analysis (26), one RCT (27), and one multi-center PCT (28) were found supporting brace treatment. There are long-term cohorts published in the literature supporting the Boston and Cheneau brace treatment (29-31). In addition, Landauer and colleagues have concluded that compliance (brace wearing time) and in brace correction determine the outcomes of brace treatment (32, 33).
This shows that stable corrections can be achieved when treatment starts early enough, and if there is enough growth for correction. This case is described more deeply in a case report (33).
The success rate with the Boston brace was about 70% (27, 28), and with the actual Cheneau standard it was > 90% (Figures 2 and 3) (30, 34). However, the same definition of success has not been applied in all of the studies. Usually, the standard definition of success is “no progression of 6° or more, or an improvement of 6° or more” (28, 34). In the RCT (27) by Weinstein et al. the rate of success was defined as the prevention of curve progression to more than 50°, while in the Italian paper on the Cheneau brace (30), the rate of success was defined as an improvement to 5° or more, or no change within the limits of ± 4°.
No evidence has been found to support spinal fusion surgery (Figure 6), not in four systematic reviews (17, 35-37), nor in two Cochrane reviews (14, 15). While the complication rate of spinal fusion directly after an operation may be small, the long-term rate of complications seems to exceed 50% of the population operated on (35, 38, 39). In addition, there is no evidence that spinal fusion surgery improves signs and symptoms of scoliosis and some literature state that the deformity may well increase again as a later effect even when the instrumentation remains stable (35). Long-term retrospective studies on the effects of surgery are rare, and most of them contain patient samples operated on using the Harrington instrumentation (40-43).
The first modern dorsal double rod instrumentation (CD instrumentation) showed a re-operation rate of 48% within the follow-up period of 20 years (44); but for the instrumentations currently used, no long-term studies exist. With the stapling operation, within only two years, a re-surgery rate of more than 50% was found (45).
Additionally, other side effects have been found; as one study points out, spinal fusion surgery may lead to post-traumatic stress disorder (46). Another study has shown that bone morphogenetic protein 2 (BMP-2), a protein applied during spinal fusion surgery, has a long list of side effects, including carcinogenesis (47, 48).
4. Discussion
Based on the current literature, high quality evidence (Level I) has been found to support physical rehabilitation and brace treatment in scoliosis (19, 21, 27), while no evidence has been found to support spinal fusion surgery in the long-term (14, 15, 17). The meta analyses (18, 26) and RCTs (19-21, 27) seem to support conservative management, while only the retrospective studies support the use of outdated surgical approaches like the Harrington rod (40-43). Long-term studies on recent surgical approaches do not exist, with the exception of one long-term study on the first modern dorsal double rod instrumentation (44). This study shows a re-surgery rate of 48% within a follow-up of 20 years (44). Moreover, one recent development shows a re-surgery rate of > 50% within two years (45). Therefore, the long-term effects of other recent instrumentations are simply not known (49). The many possible adverse effects patients may face in the long-term after the operation, and the lack of evidence for spinal fusion surgery indicate that there is no clear medical indication for surgery in AIS (17).
This study does indicate the necessity to focus on conservative treatment. Many different approaches are offered today, most of them without evidence. Therefore, it is necessary to compare the conservative approaches to ensure the most effective approaches are used. Especially when considering that during the pubertal growth spurt there is no time to waste, from the patients’ perspective, with unproven methods of treatment.
Yoga, SEAS, Dobomed, and Clear cannot claim to be the best approaches to treatment since, according to the current evidence, the new high correction approaches provide better results (19-21). The Schroth best practice approach shows the widest range of corrections and improvements of the signs and symptoms of scoliosis (37, 50-53).
With respect to highly corrective bracing, correction can be maintained even two years after wearing these braces (Figure 5) (32). Although the Boston braces have been supported by a high level of evidence, the final results of the asymmetric Cheneau standard seem to lead to a better outcome, which has also been described in a recent paper on CAD/CAM braces (54). CAD/CAM braces, when constructed appropriately, can be standardized, and these standards can be constantly improved. The smallest brace with the best possible correction available today is the Gensingen brace (GBW) (54). Therefore, a high standard of bracing can be provided in all parts of the world for the benefit and comfort of the patients (50).
Since there is no evidence for spinal fusion surgery in the treatment of scoliosis, the quality of conservative treatment should be a matter of further research. According to the literature, pain is more frequent in the population with scoliosis (55). This has been found for untreated patients, braced patients, and operated patients in the long-term as well. Indeed, pain increases post-operation over time (56); therefore, pain is not a valid indication for spinal fusion, because pain can be treated successfully with conservative measures (20, 57).
The papers on surgery, as found in PubMed, total more than 10,000, while the papers on conservative treatment are more rare. This disproportion reflects the interest and the influence of surgeons within the spinal literature. Moreover, the conflict of interest in this field has been described by Hawes (58).
4.1. Conclusions
There is a high level of evidence for the conservative treatment of scoliosis, but there are varying levels of success in the different approaches. The better the correction the better the end result. This is supported by current evidence. Therefore, in physiotherapy and in bracing only high corrective procedures should be applied.
However, spinal fusion surgery is not supported by the current evidence. According to the literature, the long-term complications of surgery for AIS far outweigh the consequences of untreated AIS.