1. Background
Spinal cord injury (SCI) is a destructive condition (1). It is associated with any motor/sensory function, preserving the level of spinal cord trauma (2). Injured Individuals often experience bone loss (3). Osteoporosis is known inevitable complications in SCI persons (4). Bone loss starts from the first day post-injury and peaks at six months post-injury (5).
There are several therapeutic interventions after spinal cord injury including resistance exercise training, hydrotherapy, locomotor treadmill training (LT) with body weight-support training and functional electrical stimulation (FES) (6). For more than a decade it was illustrated that LT in animals can increase locomotor function following spinal cord transaction (7). LT is a safe therapy (8) for treatment of neuromuscular disorders (9). LT lets spinal cord injured persons walk on a treadmill with supported body weight (10). LT has emerged from the theory of central pattern generator (CPG) (11). Traditional rehabilitation since SCI is arranged to recover ambulation through improving muscles endurance in order to strengthen and compensate for weak lower leg muscles (12).
A number of scientific researches were conducted to verify the efficacy of LT on bone mass. They have shown that the passive standing and weight-bearing may affect bone mineral density (BMD) (13), while other researches claimed that LT seems not to be effective on bone density in SCI (14). Giangregorio et al. (15) showed that 12 months LT did not increase bone density in incomplete spinal cord injured persons (iSCI). But, Carvalho et al. (16) suggested that LT was efficient in increasing the rate of bone formation. In addition, they illustrated that six months gait training increased bone formation markers (serum alkaline phosphatase and osteocalcin levels), and decreased bone resorption markers (free pyridinoline and free deoxypyridinoline) (15). Alekna et al. (13) illustrated that SCI individuals who performed daily standing had significantly higher bone density in the lower extremities after 24 months. In another study, Astorino et al. (17) illustrated that 6 months activity based therapy did not reverse bone loss usually observed within the first 6 months post injury. Furthermore, the effectiveness of rehabilitation therapy interventions depends on the details of the associated bone-loading patterns.
Despite the great advances in therapeutic intervention in past few years, there are not enough investigations on the effect of different exercise rehabilitation interventions on osteoporosis in persons with SCI, and limited studies have been conducted concerning LT and its effects on bone density. To the best of our knowledge, exercise therapeutic interventions (LT vs. conventional exercises) are effective for reduction bone loss in people with SCI. So, this study aimed to investigate the effect of progressive locomotor treadmill training (LT) on muscle mass, bone mineral density and bone remodeling (bone formation and bone resorption) in paraplegic patients.
2. Objectives
We intended to assess the effect of LT on body composition, bone mineral density and bone remodeling (bone formation and bone resorption) in paraplegic patients.
3. Methods
3.1. Subjects
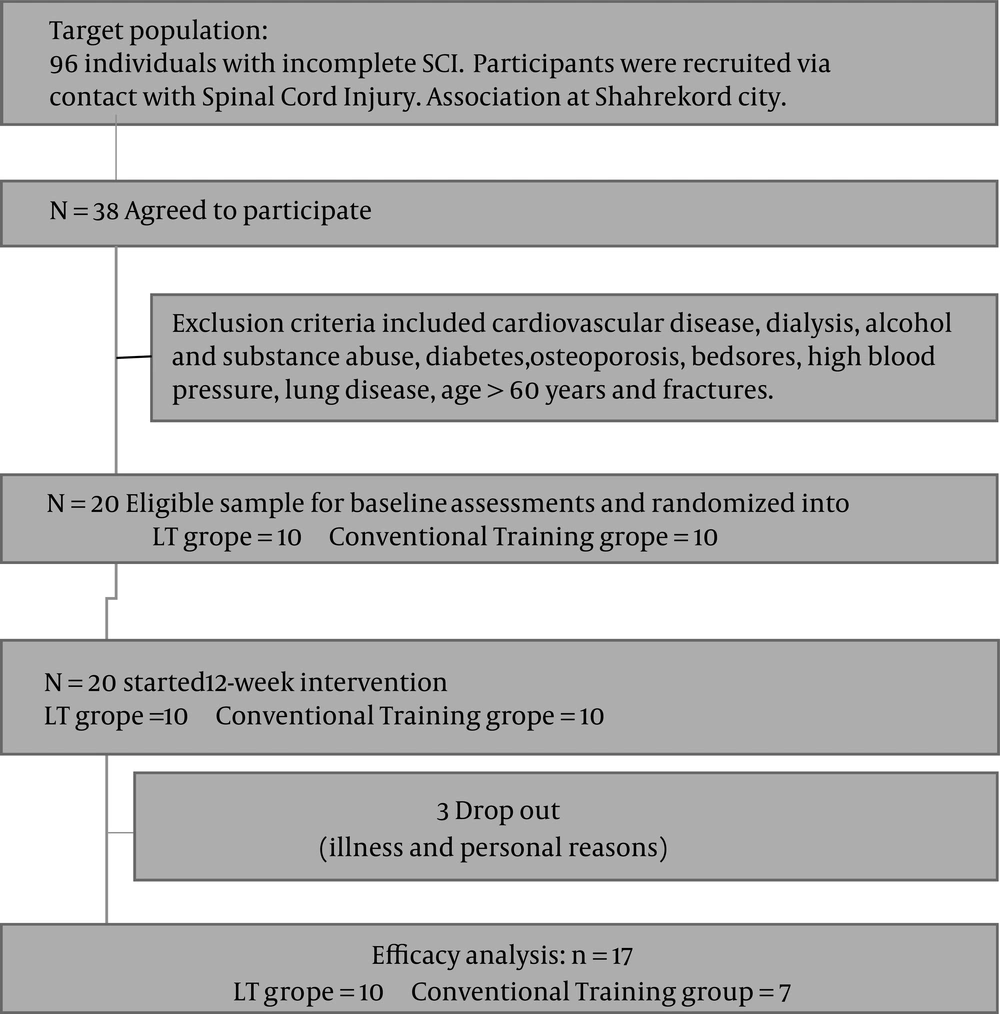
These studies aimed to focus on individuals with incomplete SCI. Participants were recruited via contact with the spinal cord injury association in Shahrekord city. 20 male patients with traumatic paraplegic spinal cord injury (18-20) (32.30 ± 1.50 years) took part in this quasi-experimental study knowingly and voluntarily. They were classified by the American spinal injury association (ASIA) as ASIA grade B and C (21). The time since injury was more than six months (18).
All subjects signed an informed consent. The subjects had no cardiovascular illness, osteoporosis, diabetes, bedsores, and high blood pressure, and aged more than 60 years. They filled out the physical activity readiness questionnaire (PAR-Q). They were assured that all questions contained in the survey would be kept strictly confidential. The study was approved by the Ethics Committee of Shahrekord University. After baseline tests, they were assigned to a LT group (n = 10) or a conventional group (n = 10) based on simple randomization. In the conventional group, three patients left the project. Most participants were injured in motor vehicle accidents or falling from height.
All subjects signed an informed consent for protection of human subjects. Based on the inclusion criteria, subjects who were classified by the American spinal injury association (ASIA) as ASIA grade B and C, were recruited in this study. Exclusion criteria included cardiovascular disease, dialysis, alcohol and substance abuse, diabetes, osteoporosis, bedsores, high blood pressure, lung disease, age > 60 years, and fractures. After exclusion of ineligible subjects, 20 iSCI patients remained as study units. The subjects filled out the medical history questionnaire. They were assured that all questions contained in the survey would be kept strictly confidential.
3.2. Exercise Training Protocols
Two kinds of exercise modalities were used. The training interventions were performed during a 12-week period on LT and conventional training (18).
3.2.1. LT
A body weight supported device was used to suspend patient’s body by wire harness, and body weight was supported by counter weight. Subjects participated in LT 4 times per week for 60 minutes per session over a 12-week period. Supported bodyweight started with a 50 percent and decreased to ensure full weight bearing. Subjects started with a speed of 0.3 km/h. Each LT session included a 10 minutes warm-up, three bouts of gait training on LT, and 10 minutes cool down.
3.2.2. Conventional Training
Conventional exercise intervention included a 10 minutes warm-up with passive stretch exercises, 45 min stretch training, over ground walking, and strengthening exercises. Therapeutic training aimed to strengthen the weak skeletal muscles and activate the paralyzed muscles. It was followed by a 10 minutes cool down period.
3.2.3. Dual-Energy X-Ray Absorptiometry
Bone mineral content (BMC) and BMD were measured using dual-energy X-ray absorptiometry (DXA) at the lumbar spine (L1 - L4) and proximal femur (18).
3.2.4. Blood Analysis
In order to examine serum osteocalcin and bone alkaline phosphatase level, a blood sample (10 cc) were collected from the patients 24 hours before the intervention and 48 hours after the last session of training in 12 hours fasting status from the antecubital vein. Blood samples were then centrifuged for 10 minutes at 4°C at a speed of 500g to separate the serum. A Boster’s human osteocalcin (N-Mid ® Company) ELISA kit was used to assess serum osteocalcin while total alkaline phosphatase was assayed by OSTASE® BAP EIA (IDS, UK) kit.
3.3. Statistical Analyses
Mann-Whitney test was used to compare the changes between LT and conventional exercise training groups after the intervention.
4. Results
The obtained results before and following 12-week exercise training interventions are presented in Tables 1 and 2, respectively.
| Variables | LT Group (n = 10) | CON Group (n = 7) | Between Group 95% CI | P Value |
|---|---|---|---|---|
| Body mass, kg | 74.30 ± 2.71 | 67.71 ± 4.31 | -9.19, 7.76 | 0.015b |
| BMI, kg/m2 | 23.90 ± 0.93 | 22.14 ± 1.50 | -2.52, 6.10 | 0.845 |
| % Body fat | 23.92 ± 1.09 | 23.73 ± 1.87 | -2.25, 5.83 | 0.78 |
| Alkaline phosphatase, U/L | 221.60 ± 22.36 | 232.57 ± 26.67 | -27.25, 20.70 | 0.04b |
| Osteocalcin, ng/mL | 13.70 ± 0.48 | 15.52 ± 0.64 | -3.47, 0.54 | 0.001c |
| BMC of the femoral neck, gr | 31.92 ± 2.50 | 28.31 ± 3.11 | -4.84, 12.06 | 0.051 |
| BMD of the femoral neck, g/m2 | 0.78 ± 0.04 | 0.75 ± 0.05 | -0.169, 0.123 | 0.464 |
| BMC of the lumbar spine, gr | 57.89 ± 0.97 | 57.25 ± 2.82 | -6.19, 4.91 | 0.626 |
| BMD of the lumbar spine, g/m2 | 0.89 ± 0.01 | 0.85 ± 0.02 | - 0.08, 0.009 | 0.051 |
Abbreviations: LT, locomotor training; CON, conventional training; BMI, body mass index; BMD, bone mineral density; BMC, bone mineral content.
aValues are expressed as mean ± SD.
bP < 0.01.
cP < 0.05.
| Variables | LT Group (n = 10) | CON Group (n = 7) | Between Group 95% CI | P Value |
|---|---|---|---|---|
| Body mass, kg | -3.59 ± 1.36 | 0.86 ± 2.32 | -8.19 , 6.76 | 0.009b |
| BMI, kg/m2 | -1.40 ± 0.52 | 0.42 ± 1.02 | -2.42 , 3.10 | 0.006b |
| % Body fat | -2.40 ± 0.43 | 0.45 ± 0.72 | -2.15, 4.73 | 0.007b |
| Alkaline phosphatase, U/L | 14.70 ± 11.20 | -22.0 ± 13.2 | -21.35, 24.70 | 0.016c |
| Osteocalcin, ng/mL | 0.25 ± 0.29 | -2.02 ± 0.31 | - 2.148 , 2.22 | 0.005b |
| BMC of the femoral neck, gr | 1.96 ± 1.20 | 0.01 ± 1.80 | -5.19, 3.91 | 0.004b |
| BMD of the femoral neck, g/m2 | 0.13 ± 0.02 | 0.01 ± 0.03 | -0.26 , -0.027 | 0.007b |
| BMC of the lumbar spine, gr | 6.01 ± 0.42 | 0.54 ± 1.04 | -12.03 , -1.20 | 0.006b |
| BMD of the lumbar spine, g/m2 | 0.08 ± 0.05 | 0.01 ± 0.01 | - 0.02, 0.009 | 0.004b |
Abbreviations: LT, locomotor training; CON, conventional training; BMI, body mass index; BMD, bone mineral density; BMC, bone mineral content.
aValues are expressed as mean ± SD.
bP < 0.01.
cP < 0.05.
Table 1 shows that before the intervention, there was a significant difference between groups in body mass, alkaline phosphatase, and Osteocalcin; and no significant between-group difference was observed in terms of other variables including BMC of the lumbar spine, BMC of the femoral neck, BMD of the femoral neck BMC of the lumbar spine, and BMD of the lumbar spine.
The obtained results showed that there were significant differences between LT and conventional training groups with respect to changes of body mass after 12 weeks of intervention (4.8% vs. 1.27%, respectively, P = 0.009). BMI decreased in the LT group after training; in conventional training group, on the contrary, the BMI increased during the experiment (-5.85% vs. 1.94%, P = 0.006). The changes in body fat percentage between the two groups were also significantly different, so that in the LT group body fat decreased, while in the conventional training group this variable increased during the 12-week period (-10.03% vs. 1.89%, P = 0.007).
The level of alkaline phosphatase increased more following LT compared to other modality (P = 0.016). The results also showed that there were significant differences in changes of osteocalcin level between two intervention groups (P = 0.005). Based on the data, there was a greater improvement in BMC of the femoral neck (P = 0.004) and BMD of the femoral neck (P = 0 007) after LT compared to conventional training. The data also indicated that the 12-week period of LT better works than the same period of conventional training in improving BMC of the lumbar spine (P = 0.006) and BMD of the lumbar spine (P = 0.004).
5. Discussion
We examined the effect of two types of exercise interventions (LT vs. conventional training) on body composition, bone mineral density and bone remodeling (bone formation and bone resorption) in paraplegic patients. In our study, regular LT showed to be able to reduce the body mass, body fat percent and BMI compared to conventional training. It seems that BWSTT provided a greater stimulus and reduced body fat percentage and body mass in iSCI compared to conventional training through involvement of a larger muscle mass and the postural challenge of being upright, (22). Similar results despite the differences in subject populations were also cited by Hicks and Ginis (2008) (22) who found that BWSTT (2 - 3 sessions/week) decreases total body fat. Recently, in accordance with our research Koury et al. (23), illustrated that despite of difference in age, type of training, exercise duration and spinal cord injury level ,three months physical training decreased total body mass (-13%), body mass index (-16%), and fat mass (-39%). Our study is inconsistent with some research reported that LT had no effect on body fat percent in iSCI (24, 25). Differences may be related to the level of spinal cord injuries (ASIA C vs. ASIA B, C), history of injury (6 months vs. 12 months), age of subjects and number of sessions per week (three times/week vs. four times/week). This study showed that the present LT training was sufficient in terms of intensity and duration to induce a decrease in the body mass, body fat percent and BMI.
These results demonstrate that 12 weeks thrice-weekly LT in this population results in significant gains in bone parameters in comparison with conventional training. However, there was no similar research to be compared with our study. In accordance with our research, some researches illustrated that prolonged exercise training improved osteocalcin levels (16). However, in acute SCI persons, training therapy did not improve osteocalcin levels (10). Previous studies varying in exercise mode, intensity, and duration and injury level, measured BMD of the femoral neck and lumbar spine (L1 - L4) by DEXA. In this study, completion of three months of LT increased BMC and BMD in comparison with conventional training. A number of researches have illustrated the effects of weight-bearing on BMD. Ben et al. illustrated that 12 weeks tilt-table standing has a little or no effect on femur bone mineral density. Mohr et al. (26) also observed that in SCI, the loss of bone mass can be partially reversed by FES cycle exercise. In a study, Jones et al. (27) showed that following activity-based training increased BMD and remained osteocalcin and alkaline phosphatase unchanged. They suggested that alternative treatment is needed to reverse osteoporosis of the lower extremities. The discrepancy in these findings may be due to differences in mode and number of exercise sessions per week. Unlike our results, intensive exercise regimens do not prevent demineralization in the lower body. Some of these differences are due to differences in intervention. Furthermore, Alekna et al. (13) confirmed that following daily standing more than five times per week had significant effects on BMD in the lower extremities. They demonstrated that standing can stimulate bone renovation. Giangregorio et al. (10) showed that twice-weekly LT for approximately six months did not prevent bone loss in acute spinal cord injured individuals. They measured bone formation marker osteocalcin and bone resorption marker deoxypyridinoline. In a case study, Davis et al. (28) illustrated that standing alone and partial weight bearing on feet with vibration did not produce positive changes in BMD. But they showed that weight bearing combined with whole body vibration had significant positive effects on BMD at trunk and spine. It seems that weight-bearing exercises produce an enough overload to cause an increase in BMD and BMC combined with body vibration. In addition, Dolbow et al. (29) illustrated that rehabilitation exercise interventions that provide enough stress are suitable for improving BMD. Some studies showed that functional electrical stimulation-cycling did not have significant effects on bone loss after SCI (30-32), But others illustrated that regular long-term FES cycle exercise can reverse loss of bone mass in SCI (26, 33).
5.1. Conclusion
Despite the fact that numerous researches showed significant differences between LT and another type of rehabilitation regime, we showed that LT may be more effective than other interventions. 12 weeks of thrice-weekly LT effectively improved BMD, BMC, and biochemical markers of bone metabolism in iSCI (ASIA classification of B and C).
5.2. Limitation
Lack of long term follow-up post interventions is a certain limitation of this study. Another limitation of this study is that we did not know whether or not patients altered their diet. Because we did not quantified the energy and mineral intake of them in the present study and there was no information about appetite changes following interventions.