1. Introduction
Guillain-Barre syndrome (GBS) is an immune-mediated acute inflammatory polyneuropathy disorder. It is characterized by mild sensory symptoms, hypo-or areflexia and rapidly progressive and symmetrical weakness that begins distally in the lower limbs and progresses in ascending fashion to involve legs and arms (1, 2). Diagnosis is made by physical examination findings, the presence of cerebrospinal fluid albuminocytologic dissociation, electrophysiological findings supporting acute demyelinating neuropathy and exclusion of other similar clinical conditions (2, 3).
Infectious agents were accused of being the most common cause of GBS in the etiology of the disease. In 60% - 70% of patients, GBS is triggered by a preceding infection by one to three weeks (4). A few cases of GBS complicated by subdural and subarachnoid hemorrhage resulted from traumatic brain injury (TBI) have been reported in the literature (5-9).
In this paper the authors report the sixth case of GBS, which followed head trauma in association with subdural and subarachnoid hemorrhage.
2. Case Presentation
A 63-year-old male patient was consulted by the neurology clinic for GBS-related weakness in upper and lower limbs, numbness and difficulty in walking and transferred to the appropriate service for rehabilitation.
From the patient’s anamnesis, it was found that the patient’s complaints had started seventeen days before admission to our clinic. He began to show weakness and numbness of upper extremities within two days and the complications as remarkable facial paralysis, speech impairment and swallowing difficulties supervened on.
Computed tomography (CT) scans of the brain, magnetic resonance imaging (MRI) and lumbar puncture were performed for the diagnosis; right after the patient was admitted to the neurology clinic with the aforementioned complaints.
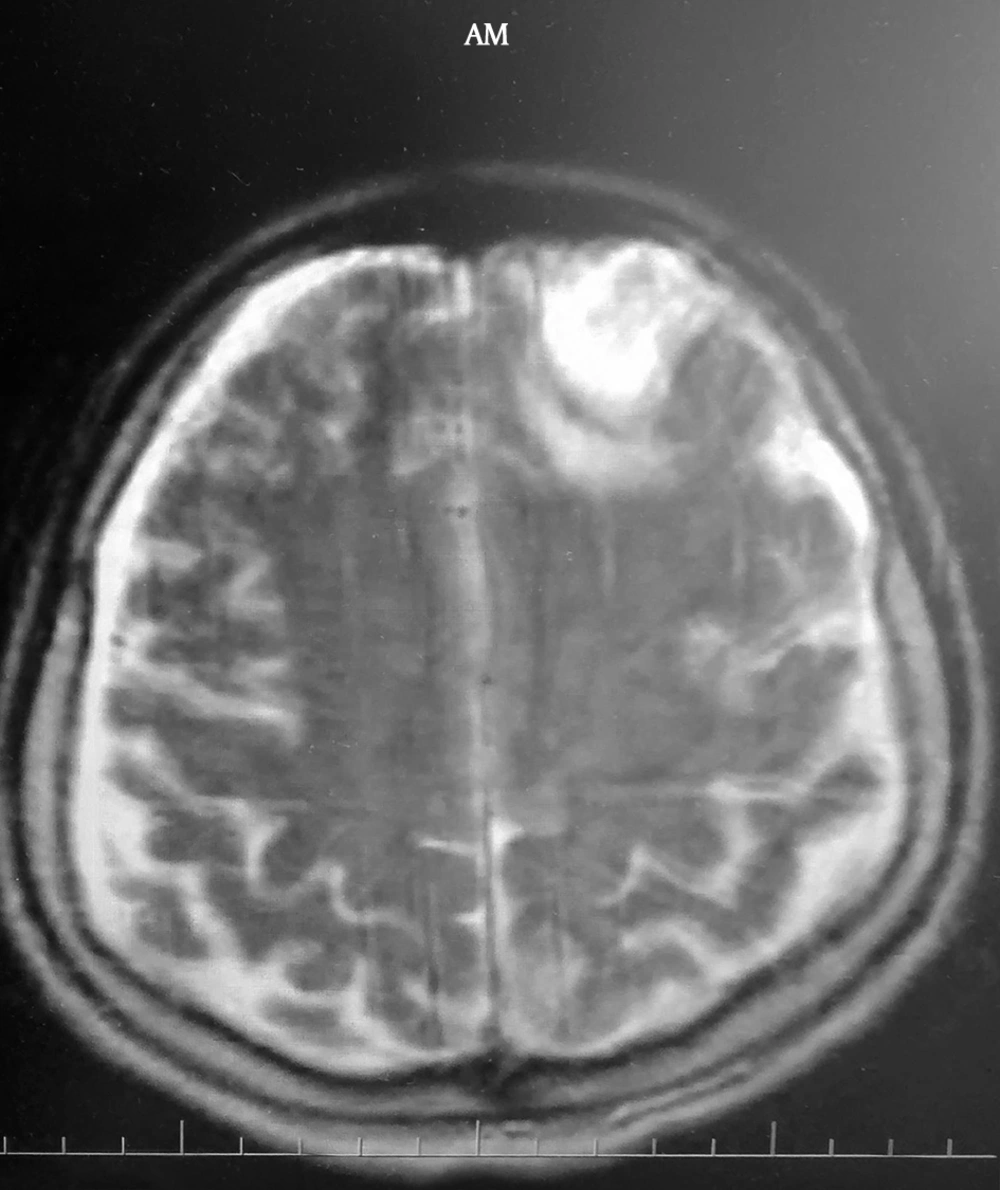
Magnetic resonance imaging showed acute 32 × 32 mm hematoma with surrounding edema on the left frontal lobe, chronic subdural hemorrhage area measuring 4 mm in maximal thickness over the right and 3 mm in maximal thickness over the left in the bilateral cerebral hemispheres and 20 × 27 mm acute hematoma at the peripheral region of the edema-gliosis area in cortical-subcortical area of the right temporal and occipital lobes (Figure 1).
Lumbar puncture revealed an elevated level of protein and normal glucose levels in the cerebrospinal fluid whereas no cell was detected.
The patient received a course of 0.4 gr/kg bodyweight intravenous immune globulin (IVIG) per day for five consecutive days as electrophysiological evaluation showed sensorimotor demyelinating polyneuropathy characteristic of GBS, affecting all four limbs. After the treatment, the patient showed relative improvement in facial paralysis and achieved complete recovery of deglutition and speech disorders, and concordantly, became able to ambulate using a walker.
In the patient’s background, there was no recorded history of infection, inoculation or surgical intervention from one to three weeks prior to the onset of weakness. The fact remains that the patient had fallen down in the bathroom and hit his head to the sink on 11.05.2015, 18 days before the symptoms appeared, and for this reason, he had spent one week in a neurosurgery intensive care unit and received an inpatient treatment for another week in neurology services. There was no history of loss of consciousness, seizure, hemodynamic instability or need for resuscitation. The CT scan at that time revealed a fracture extending through the mastoid bone in the squamous part of the right temporal bone, 25 × 22 mm parenchymal hematoma with surrounding edema in the left frontal lobe, hyperintensity suggestive of subarachnoid hemorrhage and the apparent edema in the contusion areas imaged in the right temporo-occipital and in occipital sulcus and fissure. The patient was medically treated for hemorrhage by mannitol and dexamethasone, and subsequently discharged from the hospital as being conscious, cooperative, oriented and free of ambulation aids. Apart from that, there was no history of metabolic, endocrine, cardiac diseases, surgical procedure, smoking and/or alcohol consumption.
On admission to our clinic, neurological examination revealed normal levels of consciousness, cooperation and orientation. On his musculoskeletal system investigation, the patient was able to independently stand but required a walker to ambulate. The patient exhibited full range of motion of all four extremities and the medical research council (MRC) scale revealed that the muscle strength of the right hip flexor group was 3/5 while that of left hip flexor group was 4/5. In addition, strength of other muscles in both lower extremities was 4/5 as well as that of all muscles in upper extremities. Sensory examination revealed hypoesthesia of gloves-socks type and 2-point discrimination disorder in both lower extremities whereas proprioceptive sense was found to be normal. Deep tendon reflexes were absent in all four extremities and the pathological reflexes were negative. Disability scores based on the functional independence measurement (FIM) were 35/35 for FIM cognitive, 68/91 for FIM motor and 103/126 for total score. The nine-hole peg test was conducted in order to assess the hand dexterity. The patient completed the test in 15 and 18 seconds by the right hand and left hand, respectively (where normal limit ≤ 20 seconds). Laboratory parameters were at normal levels. The rehabilitation program consisted of five sessions of superficial hot pack application followed by electrical stimulation, occupational therapy and walking and balance exercises. At the end of one week, the patient was discharged from the hospital at his own request, and was using a forearm crutch instead the walker.
3. Discussion
Guillain-Barre syndrome typically occurs when the immune system malfunctions and hence, immune response develops against its own neural tissues due to foreign antigens triggered by infectious agents (1, 2, 10). Occasionally, autoimmunity is not due to infectious episodes, and surgery, spinal anesthesia and trauma can also be the reasons (5-7). Nevertheless, the autoimmune-attack damages myelin sheaths of the peripheral nervous system and in connection with that, it leads to nerve conduction blockade resulting in muscle paralysis, which can be accompanied by sensory and autonomic disorders (11). This syndrome is a peripheral nerve disease and in general, it does not yield nerve damage in the brain and spinal cord. Except that, the syndrome has a distinctive relevance with brain and spinal cord injury.
As being the first case in literature, Duncan et al. (5) reported the development of GBS following head trauma as “post-traumatic GBS” in 1987. The case was a sixty-one-year-old patient, who had went through a head trauma resulting in bilateral frontal and parietal hemorrhage, and reported dysphagia and dyspnea on the ninth day accompanying tetra paresis with bulbar involvement and 3rd and 7th cranial nerve palsy. Hereafter, De Freitas et al. (6) presented a case of occipital hematoma and subarachnoid hemorrhage with concomitant bulbar involvement developed on the third day and ended up with mortality on the eighth day for a twenty-nine-year-old patient having a history of alcohol, marijuana and cocaine use. In a similar manner, Tan et al. (7) appraised a case where a forty-four-year-old patient with TBI with a history of alcohol use died one week after the bulbar involvement had appeared. Further, Battaglia et al. (8) enunciated another case in 2013 for a seventy-three-year-old patient with temporal and frontal hematoma where the patient had swallowing difficulties, facial weakness and tetra paresis fourteen days after spinal surgery. Lastly, Carr et al. (9) affirmed a GBS case with weakness in extremities and facial weakness that started developing on around the 17th day in a fifty-eight-year-old patient having bilateral frontal hematoma and subdural hemorrhage.
Similar to the cases reported in the literature, in our case, there were frontal lobe hemorrhage and subarachnoid hemorrhage in the occipital region resulting from serious brain injury, as well. Similar to the patients in the aforementioned reports except those presented by Freitas et al. (6) and Tan et al. (7), fully cooperative and oriented patients were exhibiting fulminant and rapidly progressive GBS involvement within one to three weeks after recovery without sequelae of musculoskeletal system. Unlike the patients mentioned in the reports of De Freitas et al. (6) and Tan et al. (7), the patient of this study did not have additional comorbidities or alcohol and substance abuse. Those patients might have already had poor immune systems due to alcohol and substance abuse. The studies investigating the association between alcohol abuse and the immune system have revealed that the number of lymphoid cells decreases in peripheral blood, spleen and thymus, and notably, there exists suppression of T cell dependent immune responses (12).
It was noted in reported cases, as well as here in this case study, that following the IVIG therapy, there was rapid recovery of the cranial nerve palsy in a few days and also slower functional recoveries occurred in motor functions, in particular at lower extremities in about five to eight weeks. The IVIG therapy was found to be effective on GBS, particularly where a rapid clinical progress, evident motor weakness and findings of bulbar involvement existed or the patient had respiratory insufficiency (10). It was shown that high-dose IVIG treatment binds the antibodies, in this way, prevents formation of new antibodies, and therewithal, has effects on the complement system. Also here in this case study, a rapid improvement was observed on facial weakness and dysphagia after IVIG treatment however, there was a partial loss of motor functions on the 18th day when the patient was admitted to our clinic. It was revealed in case reports that the improvement might be multifactorial depending on the severity of involvement during the acute stage and the degree of organ dysfunction (5-7). Similar to cases in the literature, the involvement in our patient was as severe and rapidly progressive as that which led to the development of dysphagia. In line with the literature, this result may demonstrate the loss of motor functions on the 17th day during the patient admission.
In addition to these, it was stated in literature that a statistically significant risk increase was found in GBS development following surgery as against the general population (13). Gensicke et al. (13) elucidated through their study with a sixty-three-year-old patient that the physiologic stress due to surgical trauma and changes in immunological functions might affect the cellular and humoral immune system by activation of the neuroendocrine stress axis. Rapidly progressive clinical picture of GBS improvement was evinced in postoperative phase about two to three weeks after surgery, similar to the one figured in case of TBI (14).
Previous studies reflected that TBI caused depression of cellular immunity and by extension; patients became more susceptible to infections and had anergy, namely, lack of immune response to antigens (5-9). Besides, it was reported that levels of B-cells and immunoglobulin-forming humoral immunity increased (5-9). Despite the fact that the mechanism of GBS improvement following head trauma could not be fully explained in the literature, it has been evinced that the one reason for the post traumatic pathogenesis of GBS was the molecules shown to be immunogenic such as myelin basic protein are perceived as foreign antigens due to crossing to the central nervous system depending on the impairment of blood-brain barrier (5-9). This finding has also been supported by some recent studies demonstrating that the levels of antibodies, such as anti-myelin antibodies or anti-ganglioside antibodies are increased following TBI (9), while it can be considered as a limitation of this study since the levels of antibodies were not assessed.
In conclusion, although the exact mechanism is unclear, GBS can develop around one to three weeks after TBI. Sudden onset of GBS symptoms following trauma such as facial paralysis and motor weakness in extremities may erroneously be assessed as secondary complications of the TBI and may cause a waste of time and unnecessary CT scan and MRI evaluations for a definitive diagnosis. The effect of early IVIG treatment on functional recoveries of GBS patients following TBI should also be in mind during the follow-up process.