1. Background
Osteoarthritis (OA) is the most prevalent joint disease (1, 2). A 10.2% of the Spanish population (over 4 million people) suffers from OA, and it is the cause of 50% of total disability in Spain (2). OA have a great impact on pain, function, and use of health resources. OA affects the quality of life of patients in the emotional, physical, and social aspects (3). In addition, OA is the most disabling disease in older adults, affecting 30% of people over 70 in Spain (4). OA is so prevalent that at least 70% of people over 50 have any sign of radiographic involvement (5). The direct cost of OA in Spain is 4738 million Euros per year, which corresponds to 0.5% of Gross Domestic Product (2). For these reasons, OA is a major public health problem.
The normal knee is composed of subchondral bone, synovial tissue, and articular cartilage (6). In osteoarthritis of the knee, there is destruction of articular cartilage, joint space narrowing, subchondral bone sclerosis, formation of osteophytes, and subchondral cysts (7).
Nowadays, there is no cure for OA. The main short-term objectives are to reduce symptoms such as pain, stiffness, swelling, to improve function; while long-term objectives are to reduce joint damage and decrease the destruction of the joint (2, 6, 8).
Knee OA affects mainly middle-aged people. Obesity, family history, body mass index (BMI), and repeated traumas are the likely factors that precipitate the development of OA, but are not the only factors (7). In this context, OA is not just a mechanical problem but a chronic inflammatory process with cellular and biochemical alterations that justify drug treatment and postulate Ozone as an alternative option (8-11).
Despite the paucity of clinical studies of Ozone on knee OA, in a recent review, Fernández-Cuadros et al. have stated that Ozone can reduce pain and inflammation and improve the function in these patients (12). Moreover, they have also mentioned that Ozone is able to act on multiple therapeutic targets (12).
There is no unanimous criteria for Ozone treatment protocols in knee OA (including number of doses, concentration, volume or frequency) (11, 12).
2. Objectives
The aim of this study was to: 1) demonstrate the efficacy of a treatment protocol on Ozone therapy over pain, function, and quality of life in patients with knee OA; and 2) to apply Ozone as a conservative therapeutic option in the treatment of knee OA with demonstrable level of scientific evidence.
3. Methods
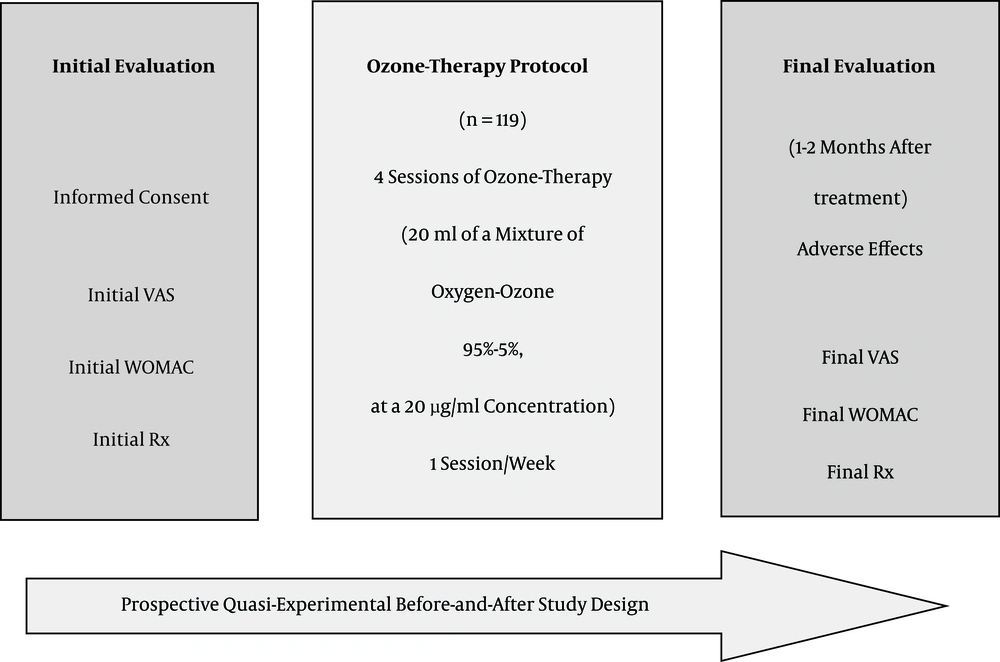
A prospective quasi-experimental before-after study was carried out on a total of 119 patients with knee OA, having Kellgren -Lawrence 2° degrees or more. They were referred to the University hospital of Santa Cristina, with clinical symptoms, demanding conservative treatment, and being failed in previous symptomatic treatment. The study was conducted from January 2012 to April 2016 (Figure 1). Patients were referred to the Traumatology and Rheumatology ward of the Multidisciplinary Musculoskeletal unit of rehabilitation department at the hospital. The study was approved by the hospital ethical committee.
Note. VAS, visual analogical scale; WOMAC, Western Ontario and Mc Master Universities osteoarthritis index; Rx, posterior-anterior weight-bearing plain radiography with the knees fully extended. Protocol applied at the department of rehabilitation at Santa Cristina’s University hospital. The study ran from January 2014 to April 2016.
The Inclusion criteria included patients: 1) with knee OA, K-L grade 2 or more; 2) with pain greater than 3 on the visual analogue scale (VAS); 3) who have failed any other conservative treatments (Non-anti-inflammatory steroidal drugs, rehabilitation, physical therapy); and 4) unwilling or not candidate for knee arthroplasty replacement.
The exclusion criteria were: 1) any formal contraindication to Ozone Therapy (favism, pregnancy, angiotensin converting enzyme inhibitors treatment, hyperthyroidism, thrombocytopenia, serious cardiovascular instability and allergy to Ozone) 2) patients who failed to complete the whole Ozone therapy treatment protocol; and 3) patients who failed to fill out any of the applied questionnaires (VAS/Western Ontario & McMaster Universities Osteoarthritis Index (WOMAC).
In the initial consultation, the goal of treatment, procedure, indications and contraindications were explained to the participants, informed consent was signed, and VAS and WOMAC scales were applied prior to treatment (Figure 1).
The proposed treatment protocol consisted of intra-articular injection of a mixture of medical Oxygen-Ozone (95% - 5%) at a concentration of 20 ug / mL (since the therapeutic dosage is between 10 - 80 ug/mL) (12), in 20 mL volume applied on 4 sessions with a weekly interval between each application. Medical Ozone generator was Ozonosan α-Plus ®. 20 mL silicone coated syringes of three bodies, with 27 G Quincke needles 4 cm in length, were used (Figure 2).
The infiltration of the knee joint was performed with the patient supine on mild knee flexion, with slight external displacement of the patella (Figure 2). In case of failure, infiltration was performed with the knee flexed 90° and it was punctured on anterior external or anterior internal patellar recess.
To clean the skin, 1% antiseptic chlorhexidine solution was used, and the area was anesthetized using a cold spray solution of ethyl chloride (100 g) dispensed as needed.
Infiltration was slowly applied to reduce the pain caused by joint distension. In the Rehabilitation Department, it is common to apply the Pérez-Moro maneuver, that is to flex and to extend the knee and get the “sign of crepitus joint”, which is audible and gives an indirect proof that the Ozone administration was performed intraarticularly. In addition, this maneuver helps distribute ozone in the joint, including patellar recesses (Figure 2). The appearance of erythema and excessive pain indicates that infiltration was performed in periarticular manner; however, this discomfort usually disappears in 10 - 15 minutes.
After the infiltration protocol is finished, a 1 - 2 month post-treatment control was performed to assess the effect of Ozone, to fulfill the VAS/WOMAC scales, and to record any adverse effect (Figure 1).
Pain was measured by visual analogue scale VAS (0 - 10), representing 10 score as the maximum pain experienced, and 0 as the absence of pain. WOMAC scale contains 24 items comprising three sections (subscales) corresponding to pain, stiffness, and function (13). Each question has five response choices (none, mild, moderate, severe, and extreme). The subtotal scores of pain (5 items), stiffness (2 items) and function (17 items) ranged 0-20, 0-8, and 0-68, respectively; where the higher the value, the worse the patient condition (13). Kellgren-Lawrence is a radiological scale, which is the most used scale in OA. This scale goes from 0 to 4 (0 = no radiological changes; 1 = doubtful osteophytes, 2 = osteophytes present; 3 = joint space narrowing; and 4 = impingement + subchondral sclerosis + subchondral geodes + marginal osteophytes) (13).
For statistical analysis, SPSS ® statistical package, version 20.0, was used. Frequencies, averages, and percentages were used in the analysis of quantitative and qualitative variables. To compare the change before and after treatment, the statistical Student t test was used, which evaluates paired quantitative variables. The level of statistical significance was 99% (P < 0.01).
4. Results
The mean age of the patients was 66.29 ± 12.77 years. The studied women constituted 70.5% (n = 84) and men 29.5% (n = 35) of the sample (Table 1). As for laterality, the most participants had affected knee on the right side (n = 71, 59.6%), while the rate of affected left knee was about 40.4% (n = 48) (Table 1).
| Variable | Value |
|---|---|
| Age (mean ± SD) | 66.29 ± 12.77 |
| Female frequency; (%) | 84 (70.5) |
| Male frequency; (%) | 35 (29.5) |
| Laterality: right knee; frequency (%) | 71 (59.6) |
| Laterality: left knee; frequency (%) | 48 (40.4) |
| Kellgren-Lawrence 2°, frequency (%) | 25 (21) |
| Kellgren-Lawrence 3°, frequency (%) | 75 (63) |
| Kellgren-Lawrence 4°, frequency (%) | 19 (16) |
| Initial VAS (0 - 10) mean ± SD | 7.89 ± 1.41 |
| Initial WOMAC pain (0 - 20), mean ± SD | 15.9 ± 2.94 |
| Initial WOMAC stiffness (0 - 8), mean ± SD | 3.5 ± 2.62 |
| Initial WOMAC function (0 - 68), mean ± SD | 49.5 ± 13.68 |
| Global WOMAC (0 - 96), mean ± SD | 68.9 ± 17.09 |
Abbreviations: SD, standard deviation; VAS, visual analogical scale; WOMAC, western Ontario and Mc master Universities index for osteoarthritis.
The most frequent Kellgren-Lawrence radiological OA grade was 3rd degree (n = 75, 63%), followed by 2nd (n = 25, 21%), and 4th (n = 19, 16%). The average severity of OA in the sample according to the Kellgren-Lawrence scale was 2.94° (Table 1).
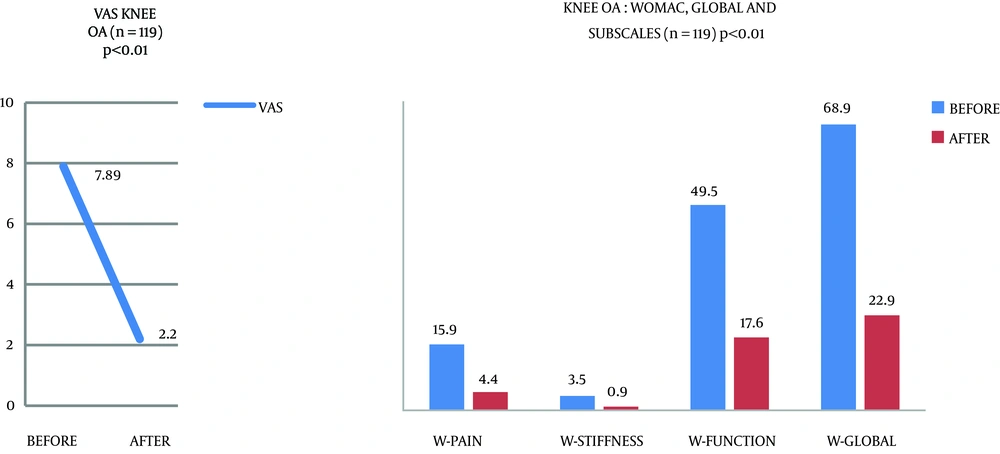
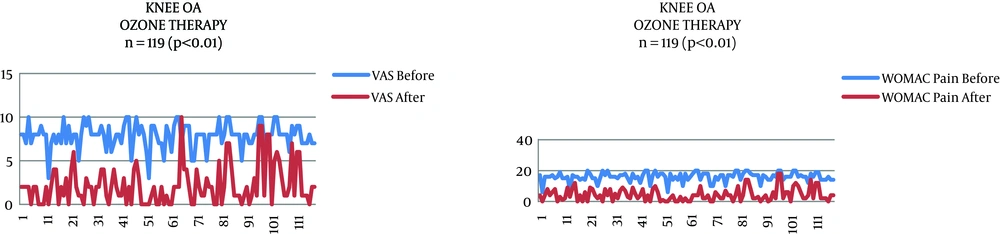
Before treatment, the score of pain measured by VAS was 7.89 that significantly (P < 0.0001) decreased to 2.1 after treatment (Table 2, Figures 3 and 4).
| Variable | Before | After | Statistical Significancea |
|---|---|---|---|
| VAS (0 - 10), mean ± SD | 7.89 ± 1.41 | 2.2 ± 2.26 | P < 0.0001 |
| WOMAC pain (0 - 20), mean ± SD | 15.9 ± 2.94 | 4.4 ± 4.09 | P < 0.0001 |
| WOMAC stiffness (0 - 8), mean ± SD | 3.5 ± 2.62 | 0.9 ± 1.26 | P < 0.0001 |
| WOMAC function (0 - 68), mean ± SD | 49.5 ± 13.68 | 17.6 ± 14.80 | P < 0.0001 |
| Global WOMAC (0 - 96), mean ± SD | 68.9 ± 17.09 | 22.9 ± 13.11 | P < 0.0001 |
Abbreviations: SD, standard deviation; VAS, visual analogical scale; WOMAC, western Ontario and Mc master Universities index for osteoarthritis.
aT-Student test for paired samples.
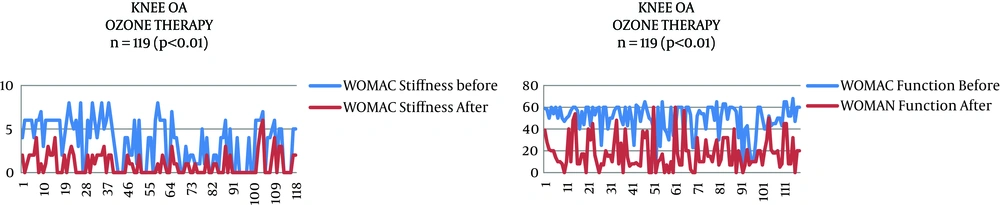
Prior to treatment, the WOMAC-pain subscale scored 15.9, the WOMAC-stiffness subscale 3.5, and the WOMAC-function subscale 49.5. All these values significantly decreased in post-treatment to the scores of 4.4, 0.9, and 17.6, respectively (P < 0.0001). The total WOMAC score after treatment decreased from 68.9 to 22.9 (Table 2, Figures 3, 4 and 5).
A significant difference was observed in pain scores measured by VAS before and after treatment and also an improvement in both total WOMAC, and its subscales, with P < 0.0001 (Table 2).
After the infiltration, a mild pain accompanied by erythema in 8.4% of cases (10 patients) was observed as complication; the same disappeared in a few minutes.
5. Discussion
Currently, the intraarticular administration of Ozone in the treatment of knee OA is not recommended in the European clinical practice guidelines (10, 14, 15). Moreover, in 2008, the recommendations of the osteoarthritis research society international (OARSI) proposed 25 recommendations, from which, 12 are non-pharmacological, 8 are pharmacological, and 5 are surgical; none of them includes Ozone (10).
The current guidelines state that the goals of OA treatment in short-term are to decrease pain and inflammation, and improve function; while in long-term, the objectives are set to stop joint and subchondral bone damage (2).
There is limited evidence on the effectiveness of Ozone therapy in patients with knee OA and its mechanism is also unknown. In Ozone therapy, various biological effects are suggested. Increased tissue oxygenation and anti-inflammatory and analgesic effects through stimulation of nociceptive system could explain the therapeutic effects of Ozone in musculoskeletal diseases (16).
Despite limited evidence and a few published studies, some authors like Fahmy, Riva-Sanseverino, Escarpenter, Milanes, Cabot, Samper-Bernal, among others, have demonstrated the effectiveness of Ozone in reducing pain and stiffness and improving function in knee OA (10); hence, the importance of our study is revealed.
It must be emphasized that in terms of methodology, the aim of our study was to provide a prospective quasi-experimental before-after trial, which has a level of Evidence 2B and an Strength of Recommendation B (3, 15, 17), allowing us to postulate Ozone as a conservative therapy for the treatment of knee OA, with a level of demonstrable scientific evidence.
Osteoarthritis is a degenerative joint disease that causes pain, decreases function, and affects the personal, social, family, and labor aspects of patients (16).
In knee osteoarthritis, major pathological changes are the progressive loss of cartilage, meniscus and articular capsule (7). Although the exact etiology of osteoarthritis is not entirely understood, the main feature is the slow and progressive articular hyaline cartilage degradation (18).
The chondrocyte is responsible for the maintenance of joint cartilage. In the arthritic joint, there is an imbalance between catabolic factors (with release of mediators / pro-inflammatory cytokines) and decreased compensatory anabolic factors (cytokines / anti-inflammatory mediators, growth factors, etc.) (18). Cytokines released by chondrocytes involved in the catabolic process of extracellular matrix are IL1, IL6, IL8, IL17, LIF, TNF-α, IFN-γ, NO, and MMP 6. Therefore, the proteolytic degradation of extracellular matrix is an important mechanism of joint degradation 6. In this regard, future OA therapy should produce an inhibition of proteolytic enzymes (mineral metal proteases or MMP), an inhibition of NO synthesis, as well as pro-inflammatory cytokines (IL1, IL6, TNF-α) and apoptosis through caspase. Moreover, OA treatment should stimulate anti-inflammatory cytokines (IL9, IL0, IL13) and growth factors (TGF-β, IGF-1) (6). That is, the future of OA is to apply trophic factors that could incline the balance in favor of the synthesis of the extracellular matrix (19). In a recent review article, Fernández-Cuadros et al. have stated that Ozone could act as a therapeutic agent in both catabolic factors (pro-inflammatory cytokines) and anabolic factors (anti-inflammatory cytokines, growth factors, among others) (12). These properties would explain the effectiveness of Ozone in the treatment of knee OA, which has been clinically demonstrated in this study.
European clinical guidelines suggest that for OA treatment, experimental studies should include pain, function, and quality of life as object in the effectiveness of the proposed treatments (15). That is why VAS and WOMAC scales included in our study. WOMAC scale is a specific quality-of-life scale for knee which evaluates pain, stiffness, and function (13).
The application of our treatment protocol (4 weekly intra-articular injections of 20 mL of Oxygen-Ozone 95% - 5% mixture at a concentration of 20 ug / mL) has reduced pain measured by VAS from the score of 7.9 to 2.2. It also has improved the quality-of-life measured by the total WOMAC Scale (scored from 68.9 to 22.9), and its subscales, such as WOMAC-pain (15.9 to 4.4), WOMAC-stiffness (3.5 to 0.9), and WOMAC-function (49.5 to 17.6), demonstrating the effectiveness of our protocol in reducing pain, and improving function and quality of life among these patients. These findings allow us to apply Ozone as a promising treatment for knee OA.
Our results are in accordance with those of Samper-Bernal, who after five weekly injections of 10 mL at a 25ug / mL ozone concentration, achieved a decrease in pain measured by VAS from 6.88 to 3.98, and decreased scores on the subscales of WOMAC-pain from 8.12 to 4.2, WOMAC-stiffness from 3.39 to 2.1, and WOMAC-function from 29.1 17.5 (10). The age of our sample was 66.29 years and in Samper-Bernal’s study was 69.9 years, which makes the results comparable.
Also, our study results comply with Moreti ones, which after 3 infiltrations (1 per week) of 5 mL Ozone at a concentration of 15ug / mL followed by hyaluronic acid, could decrease pain measured by VAS from 7.9 to 2.8; an effect that was maintained during 3 months (20).
Our findings are also consistent with Mishra results, indicating after 3 sessions of injection (1 per week) of 10 mL Ozone at a concentration of 30 ug / mL, a success rate of 80% in pain and stiffness reduction, and functional capacity improvement measured by the WOMAC scale during 3 months of treatment was achieved; the result that was maintained up to 6 months (7).
Hashemi found that the application of 3 sessions (1 per week) of 5 to 7 mL of ozone at a concentration of 15 ug / mL decreased pain measured by VAS from 7.6 to 2.8, and improved the overall WOMAC by giving a score decreased from 81.6 to 56.3, in patients with knee OA Kellgren-Lawrence 1st - 2nd grade; heir obtained results are in agreement with ours (16).
Ciobutaru conducted a study on100 patients with knee OA in which, the results have shown that Ozone, peri-articularly applied, in 5 mL volume, concentration of 2 - 5ug / mL per injection, and a total Ozone injection of 40 - 50 mL per session for up to 12 sessions per patient, was able to decrease the WOMAC-pain score from 9.8 to 5, the WOMAC-stiffness score from 3.2 to 1, and the WOMAC-function score from 22.6 16.5 (21). This explains why, even if there was a suspicion that the infiltration was not performed as intra-articular injection, the expected clinical improvement was achieved.
The method of intra-articular infiltration that is applied in our department has no serious complications, except mild pain and erythema following infiltration (occurred in only 8.4% of patients, n = 10), which subsides in 10 - 15 minutes. This confirms the fact that Ozone treatment has mild complications, it is easy to perform, and it provides reproducible and sustainable results, as claimed by several authors (22).
Most of our patients appreciate the effect of Ozone after the 1st-2nd infiltration (1 - 2 weeks of post-treatment); however, the proposed treatment protocol (4 infiltrations once a week) was completed, and patients came back to be followed up a month after treatment. By that time, the maximum benefit was confirmed, and final evaluation surveys were conducted. This rapid analgesic effect (1 - 2 weeks post treatment) comply with that reported by Cardelli, who claims that ozone causes a rapid pain relief, and 30% recovery of function in OA, one month after treatment (23). This is in accordance with the findings of Gallucci and Bocci (24, 25), who stated that Ozone produces rapid pain relief, reduces inflammation, and allows early mobilization. Samper-Bernal findings show that Ozone provides analgesia in knee OA with a rapid onset and sustained effect for 3 - 6 months (10), an assertion that is consistent with the results of our research.
These results confirm that the effect of Ozone is faster even than SYSADOA drugs (Symptomatic Slow Acting Drugs for Osteoarthritis), approved for knee OA treatment. SYSADOA needs at least 3 to 6 months of continuous treatment (such as glucosamine or chondroitin sulfate) to reach symptomatic pain relief (2). This analysis is important because the cost for annual treatment per patient with OA in Spain is 1503 Euros (including doctor visits, hospital admissions, and drugs). These would favor the balance towards Ozone, a drug that is safe, cheap, and effective (i.e. it is cost-effective). In fact, Alexandre argues that Ozone is cheap and safe, so their cost / effectiveness could excel the systemic drug therapies currently recommended (26). For these reasons, we agree with Moreti to consider that Ozone should be included in clinical guidelines as an effective conservative treatment for knee OA (20).
As a limitation of this study, we can point out to lack of a control group. However, as several studies support the effectiveness of Ozone in pain, function, and inflammation in patients with knee OA (12), including patients who were referred to rehabilitation department for this specific intervention; it is not ethical to deny such a treatment on these patients. Therefore, a quasi-experimental before-after study is suggested to solve such an ethical problem, as well as the abscence of a control group, and give clinical base evidence.
Besides, it is difficult to collect patients in prospective studies because the treatments are long (4 weekly sessions) and follow-up is made one-two months later. Indeed, most of the patients are treated privately. However, we believe that the use of Ozone in a public hospital like ours, and the study of the pathophysiology of OA, will benefit our patients, especially when health resources are limited and the demand for health care grows exponentially, and the expectancy of life increases in western populations like in Spain. The private pharmaceutical industry is not interested in the study of the efficiency of Ozone on pain in osteoarthritis of the knee due to various economic interests.
5.1. Conclusions
Ozone is a safe, cheap, and effective treatment able to reduce pain significantly and stiffness, and to improve function, as measured by VAS/WOMAC scales, in patients with knee osteoarthritis.
The results of this study show a good level of evidence as well as a good grade of recommendation, which allows us to use Ozone as a conservative therapeutic option in the treatment of osteoarthritis of the knee.