1. Background
The world is aging rapidly and it is expected that, by 2050, the worldwide population of older adults may reach almost 2 billion, 80% of them living in developing countries (1). Currently, over half of the world’s older adults live in Asia (2). India is facing challenges also owing to the steady pace of demographic transition (3). In India, ‘older adult’ is defined as a person aged 60 years and above. It is projected that the proportion of older people in the population will increase to 11% by 2025 and 19% by 2050 (4).
Falls are very common in older adults (5). The prevalence of falls among older adults in the Indian population is reported to be between 14% and 53% (6, 7). Falls can affect psychological functioning, which may lead to a fear of falling (FOF). This is a major health problem among older people living in communities, both among those who have experienced a fall and those who have never done so (8). FOF is defined as “low perceived self-efficacy at avoiding falls during essential, non-hazardous activities of daily living” (9). A common means to measure fear of falling is to assess self-efficacy related to falls. This essentially involves assessing a person’s perception of his or her capabilities to perform specific activities without falling.
The activities-specific balance confidence (ABC) scale is an instrument to measure fear of falling, developed and published in English by Powell and Myers in 1995 for the Canadian population (10). It is a subjective measure of balance confidence in performing various ambulatory activities without falling or experiencing a sense of unsteadiness. The activities-specific balance confidence scale is a 16-item, self-reporting measure, in which patients rate their confidence of balance in performing certain activities. The items are rated on a scale that ranges from 0 to 100. A score of 0 represents no confidence and a score of 100 represents complete confidence. The overall score is calculated by adding individual item scores and then dividing by the total number of items (10). It is recommended that a self-reported measure be translated and adapted to the appropriate culture before it is used with subjects whose first language is not English (11). Apart from the English version (10), this scale has been translated and adapted into French-Canadian (12), Chinese (13), German (14), Turkish (15), British English (16), and Brazilian Portuguese (17).
Hindi is the fourth most commonly spoken language globally, spoken by more than 260 million people all over the world (18). Hindi is the official language of India, the country with the second largest population in the world (19). Currently, no measure is available for assessing balance confidence in older adults whose primary language is Hindi. When the self-administered scales are not available in the native language of the patient, the therapist may be forced to self-translate or interpret the scale to the patient, which may affect the essential construct of the measurement. A Hindi version of the ABC scale would provide Hindi-speakers with the opportunity to communicate more effectively with their therapist. The availability of a self-administered scale in their native language will make clinical management and research more effective.
2. Objectives
The purpose of this study was to perform and evaluate the translation and cross-cultural adaptation of the ABC scale into Hindi (ABC-H). We aimed to obtain semantic, conceptual, and cultural equivalence between the original and ABC-H. Test-retest reliability (ICC2, 1), internal consistency (Cronbach’s α), concurrent validity, standard error of measurement (SEM), and minimum detectable change (MDC) were determined to check the psychometric properties and to establish the reference value of the ABC-H scores as a measure of balance confidence in community-dwelling Indian older adults.
3. Materials and Methods
One hundred and three subjects, aged 60 to 86 years, who were able to read and speak Hindi, were approached. Two refused and one failed to complete the scale. Thus, a sample of 100 subjects was used for analysis. Subjects were university employees, older people living in the vicinity, and individuals accompanying patients attending the outpatient physiotherapy facility at Jamia Millia Islamia university, New Delhi, India. Patients who received physiotherapy treatment or those with cognitive and psychotic problems were excluded. All subjects gave their written consent. The institutional human ethical committee of the Jamia Millia Islamia university, New Delhi, India, approved the study.
This study involved three phases: 1) translation and cross-cultural adaptation of the original English version of the ABC scale into Hindi; 2) psychometric testing in a sub-sample of 50 older adults; and 3) a cross-sectional study to determine the level of balance confidence in older adults.
3.1. Phase 1: Translation and Cross-Cultural Adaptation
The translation and cross-cultural adaptation process was done according to the guidelines for the process of cross-cultural adaptation of self-reporting measures by Beaton et al. (20). In the first step, the original scale was forward-translated to Hindi with the purpose of retaining the meaning of the questions in the original questionnaire. The first translations were independently done by two different native-speaking Hindi translators. One translator (the “native” translator) was not familiar with the topic. In the second step, synthesis of the translations was done by the two translators and a recording observer. The translators assessed the discrepancies in the translations and came up with a consolidated Hindi version; when a concept had no equivalent in the Indian culture or language, it was modified to suit the cultural context. In the third step, a back translation was carried out by two independent bilingual English language expert translators of the synthesized version of ABC-H. Back translation was done to verify whether the Hindi version adhered to the sense of the original version as closely as it should. The two translators were neither informed of the concepts being explored nor aware of the original version, and they did not have any medical background. In the fourth step, both the forward and the back translations were submitted to a seven-member bilingual expert committee consisting of two physiotherapists, a linguist, and four translators. To identify difficulties and correct mistakes, the committee discussed various options for items and responses with respect to semantic, idiomatic, experiential, and conceptual equivalence, based on the original version. None of the items was omitted. This step ended when a satisfactory formulation of the beta version was obtained. At the end, the pilot testing of the final version of the ABC-H scale was done with five older adults to ascertain its fluency and clarity and to check whether responses were understood correctly. They found that the instructions and items were easy to read and understand. None of them recommended any modifications in the final version of the scale.
3.2. Phase 2: Analysis of Psychometric Properties of the ABC-H Scale
One hundred subjects were assessed using the ABC-H scale in an individual face to-face interview. Out of these 100 subjects, a sub-sample of 50 subjects (n = 50) was randomly selected by drawing lots for reassessment on the same instrument after two weeks, to establish test-retest reliability. A two-week interval was chosen to minimize chances of subjects’ recall of the contents from the previous assessment. This period was also considered optimal for avoiding the potential occurrence of significant events or changes in their life circumstances that could also impact on their self-perceived balance confidence ratings.
The falls efficacy scale international (FES-I) is a widely accepted tool for assessing balance confidence, developed and validated by the prevention of falls network Europe (ProFaNE). FES-I has excellent reliability and validity (21, 22) across different cultures and languages (23). The Hindi version of FES-I was used to establish the concurrent validity of ABC-H.
3.3. Phase 3: Normative Value of ABC-H Scale
The purpose of this phase of the study was to obtain normative values for the ABC-H scale in Indian community-dwelling older adults. The normative values (n = 100) were determined in the context of balance confidence to be predictive for older adults of both genders, aged between 60 and 86 years.
3.4. Data Analysis
Statistical analysis was carried out using SPSS version 21.0 for Microsoft Windows. Mean ± SD for age and BMI was calculated for all subjects. Frequency was calculated for the gender distribution of the sample. The Kolmogorov-Smirnov test was conducted to check for normal distribution of data and a parametric test was applied for further analysis. Systematic error (the mean of differences of scores of the test and retest) was calculated by paired t-test with a significance level of P ≤ 0.05.
Acceptability of the scale was assessed by calculating the percentage of refusals, completed questionnaires, missing items, and time taken to complete the scale. Willingness to fill in the scale a second time was used to assess its acceptability.
The internal consistency of the 16-item ABC-H scale was determined using Cronbach’s α. George and Mallery (24) provided the following rules of thumb for the interpretation of Cronbach’s α coefficient value: ≥ 0.9, excellent; ≥ 0.8, good; ≥ 0.7, acceptable; ≥ 0.6, questionable; ≥ 0.5, poor; and ≤ 0.5, unacceptable.
Test-retest reliability was established using the intra-class correlation coefficient; two-way random effects model (ICC2, 1). ICC > 0.90 indicated excellent stability and repeatability of the scale items (25). Pearson’s correlation coefficient was also used to evaluate the relationship between initial and final total scores of the ABC-H scale.
Standard error of measurement (SEM), as an indicator of absolute reliability, was calculated for the ABC-H total score and each item score, using the following Equation (26):

Minimum detectable change (MDC95) is a statistical estimate of the smallest amount of change that can be detected by a measure that corresponds to a noticeable change in ability. The MDC is the minimum amount of change in a patient’s score that ensures the change is not the result of measurement error. MDC95 was calculated using the following Equation (27):

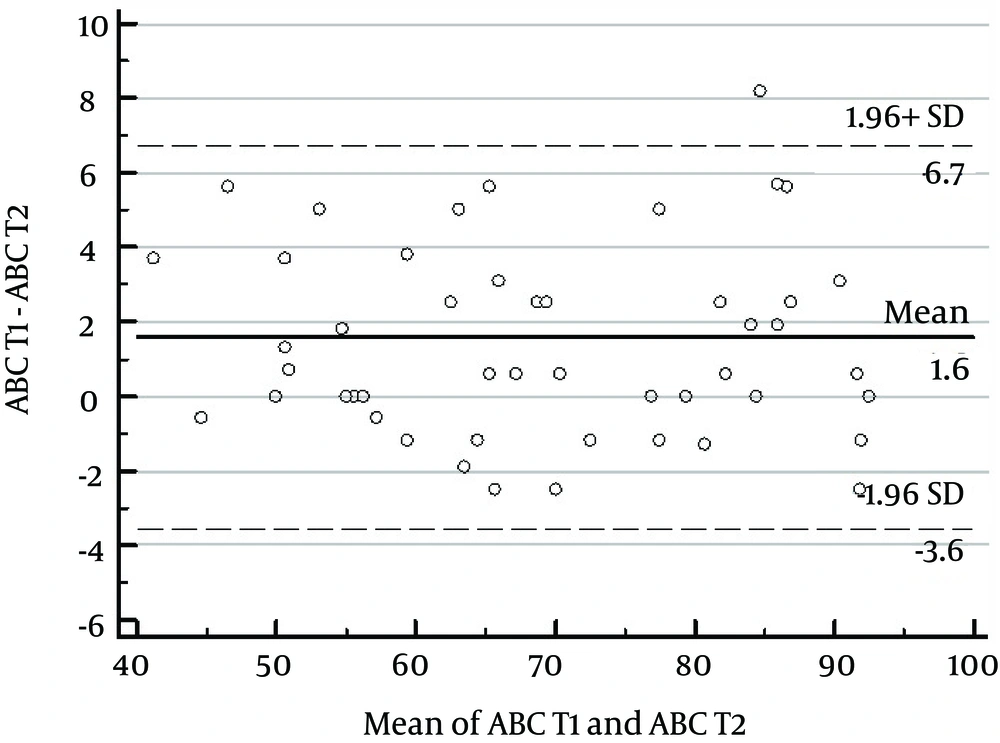
Bland-Altman plots were used to compare measurements of the ABC-H total score between initial test and retest (28).
Concurrent validity was established by correlating the total score of ABC-H with the total score of FES-I using Pearson’s correlation coefficient. Coefficient value > 0.90 to 1 was interpreted as very strong correlation (29, 30).
Floor/ceiling effects were considered present if more than 15% of the participants achieved either the lowest-possible or highest-possible score of the scale. If floor or ceiling effects are present, it is likely that extreme items are missing in the lower or upper end of the scale, indicating limited content validity (31).
4. Results
4.1. Subject Characteristics
Age mean (range) and BMI (mean ± SD) of the subjects in the main study (n = 100) and in the psychometric study (n = 50) were 70.4 (60 - 86) years, 23.65 ± 2.91 kg/m2 and 70.16 (59 - 83) years, 23.63 ± 3.48 kg/m2, respectively. Their socio-demographic characteristics are summarized in Table 1.
| Variable | Main Study (n = 100) | Psychometric Study (n = 50) |
|---|---|---|
| Gender | ||
| Male | 70 | 38 (76) |
| Female | 30 | 12 (24) |
| Age, y | ||
| 60 - 69 | 42 | 25 (50) |
| 70 - 79 | 48 | 21 (42) |
| 80 - 86 | 10 | 4 (8) |
| Marital status | ||
| Single | 2 | 2 (4) |
| Married | 90 | 44 (88) |
| Widowed | 6 | 3 (6) |
| Divorced | 2 | 1 (2) |
| Occupationally active | ||
| Yes | 17 | 9 (18) |
| No | 59 | 34 (68) |
| Retired | 24 | 7 (14) |
| Educational level | ||
| Elementary | 41 | 19 (38) |
| Middle school | 23 | 16 (32) |
| High school | 28 | 15 (30) |
| University | 8 | 4 (8) |
| Use of walking aids | ||
| Yes | 16 | 6 (12) |
| No | 84 | 44 (88) |
| History of fallsb | ||
| Yes | 17 | 8 (16) |
| No | 83 | 42 (84) |
| Habit of regular exercise, times/wkc | ||
| > 3 | 42 | 18 (36) |
| < 3 | 58 | 32 (64) |
Characteristics of the Subjectsa
4.2. Translation and Cross-Cultural Adaptation
Out of the 16 original items in the ABC original scale, 8 items were considered to be culturally, semantically, or regionally unsuitable and were modified (Table 2). Item 3 was found traditionally “inapt” and was modified because most Indians do not have closets in their homes in which to keep their slippers. The inclusion of such details as, specifically, “…front of a closet” would also add complexity and detract attention from the main purpose hence, the phrase was deleted. In item 4, “can off” was replaced with “container,” because the word “can” was unfamiliar.
| Item | Original Items | Modified Items |
|---|---|---|
| 3 | Bend over and pick up a slipper from the front of a closet floor | Bend over and pick up a slipper from the floor |
| 4 | Reach for a small can off a shelf at eye level | Reach for a small container from a shelf at eye level |
| 8 | Walk outside the house to a car parked in the driveway | Walk outside the house to a standing vehicle in front |
| 9 | Get into or out of a car | Get into or out of a vehicle |
| 10 | Walk across a parking lot to the mall | Walk across a parking lot to the shops |
| 12 | Walk in a crowded mall where people rapidly walk past you | Walk in a crowded shopping center where people quickly walk past you |
| 13 | Are bumped into by people as you walk through the mall | Are bumped into by people as you walk through the shopping center |
| 16 | Walk outside on icy sidewalks | Walk outside on slippery pavements |
Original and Modified Items in the Cross-Cultural Adaptation of the ABC Scale
In items 8 and 9, “car” was replaced with the generic word “vehicle”, since the car is not a common mode of transportation among older adults in India, most of whom use public transport of various kinds. In addition, in item 8, “car parked in driveway” was replaced with “standing vehicle in front,” as a driveway means a private road for vehicles connecting a house with a public road, and many Indian houses do not have driveways.
The word “mall” was replaced with “shops” or “shopping center,” to match for demographical differences in items 10, 12, and 13, because shops and shopping centers are more common in India than malls. Finally, for item 16, which is concerned with perceived balance confidence in negotiating slippery outdoor surfaces, the original words “icy sidewalks” were replaced with “slippery pavement,” because these conditions do not apply in the Indian climate (Table 2).
4.3. Acceptability
The ABC-H scale was completed by 99% of cases. Of all the participants approached (n = 101), only 0.99% (1 person) did not complete the questionnaire, indicating that the scale had good acceptability. Completing the questionnaire typically took 7 - 15 minutes. None of the items was considered to be confusing. All respondents from the subsample (n = 50) were willing to fill out the questionnaire for a second time, and completed it.
4.4. Reliability
4.4.1. Internal Consistency
Cronbach’s α of each item in the ABC-H scale ranged from 0.88 to 0.97; thus, all 16 items exhibited excellent to good internal consistency. Cronbach’s α of the total score for the scale was 0.99, and 0.95 for each item if deleted, which again indicates excellent internal consistency. Pearson correlation between total score and each item score was calculated to assess the homogeneity of the scale, which was found to have high to moderate positive correlation (r = 0.57 to 0.80), as shown in Table 3.
| ABC-H Item | Initial Test (n = 50)a | Retest (n = 50)a | P Valueb | ICC2, 1 | 95% CI | SEM | Cronbach’s α | MDC95 | |
|---|---|---|---|---|---|---|---|---|---|
| LB | UB | ||||||||
| 1 | 92.80 (11.4) | 91.60 (11.3) | 0.083 | 0.90 | 0.84 | 0.95 | 3.60 | 0.95 | 10.1 |
| 2 | 79.8 (19) | 77.49 (18.9) | 0.083 | 0.86 | 0.78 | 0.92 | 7.10 | 0.93 | 19.9 |
| 3 | 75.8 (21.9) | 74 (23.2) | 0.202 | 0.90 | 0.83 | 0.94 | 6.92 | 0.95 | 19.4 |
| 4 | 78.6 (20.7) | 79.4 (21.1) | 0.789 | 0.91 | 0.85 | 0.95 | 6.21 | 0.95 | 17.4 |
| 5 | 62 (25.1) | 61.3 (24.7) | 0.789 | 0.78 | 0.66 | 0.88 | 11.7 | 0.88 | 32.8 |
| 6 | 55 (25.2) | 56 (25.7) | 0.481 | 0.92 | 0.87 | 0.96 | 7.12 | 0.95 | 19.9 |
| 7 | 73.6 (23.8) | 67.8 (23.5) | < 0.001 | 0.92 | 0.73 | 0.96 | 6.73 | 0.97 | 18.8 |
| 8 | 86 (14.2) | 84 (13.2) | 0.335 | 0.80 | 0.67 | 0.88 | 6.35 | 0.88 | 17.8 |
| 9 | 84.6 (14.4) | 81.2 (15.33) | 0.010 | 0.80 | 0.65 | 0.88 | 6.46 | 0.90 | 18.1 |
| 10 | 75 (15.1) | 72.8 (16.29) | 0.132 | 0.79 | 0.65 | 0.87 | 6.94 | 0.88 | 19.4 |
| 11 | 75.4 (15.4) | 71.40 (18.4) | 0.002 | 0.84 | 0.70 | 0.91 | 6.16 | 0.92 | 17.2 |
| 12 | 65 (21.3) | 65 (23.05) | 1.0 | 0.90 | 0.83 | 0.94 | 6.73 | 0.94 | 18.8 |
| 13 | 59.6 (26.7) | 58.6 (26.65) | 0.417 | 0.94 | 0.91 | 0.97 | 6.56 | 0.97 | 18.4 |
| 14 | 77.6 (22.9) | 74.6 (22.5) | 0.018 | 0.92 | 0.86 | 0.96 | 6.47 | 0.96 | 18.1 |
| 15 | 46.2 (24.8) | 46.8 (24.83) | 0.595 | 0.95 | 0.91 | 0.97 | 5.54 | 0.97 | 15.5 |
| 16 | 42.4 (14.50) | 37.8 (14.03) | 0.001 | 0.75 | 0.54 | 0.86 | 7.25 | 0.88 | 20.3 |
| Total | 70.58 (14.18) | 68.71 (14.35) | 0.000 | 0.97 | 0.90 | 0.99 | 2.45 | 0.99 | 6.9 |
Results of t-Test, Test-Retest Reliability ICC2, 1 (95% CI), Standard Error of Measurement (SEM), Internal Consistency (Cronbach’s α), and Minimum Detectable Change (MDC) of ABC-H Scale
4.4.2. Test-Retest Reliability
The test-retest reliability (ICC2, 1), with 95% CI, SEM, and MDC results of the scale, are given in Table 3. The ICC2, 1 for total score was 0.97 (0.90 - 0.99), which indicates excellent test-retest reliability. All the items had excellent scores, ranging between ICC = 0.78 and 0.95. Item 15 (escalator not holding railing) had maximum ICC of 0.95 (0.91 - 0.97), while item 5 (reach on tiptoes) had the least ICC, at 0.78 (0.66 - 0.88) (Table 3).
Paired t-tests showed predominantly non-significant differences between the means of the two sessions across all items and the total score of the ABC-H scale. However, a significant but small difference in item 7 (5.8, P < 0.05), item 9 (3.4, P < 0.05), item 11 (4.0, P < 0.05), item 14 (3.0, P < 0.05), item 16 (5.0, P < 0.05), and total ABC-H score (0.88, P < 0.05) was observed between initial and retest scores.
4.4.3. SEM and MDC
SEM and MDC for the ABC-H total score was 2.45 and 6.7, respectively (Table 3).
4.4.4. Bland-Altman Plot
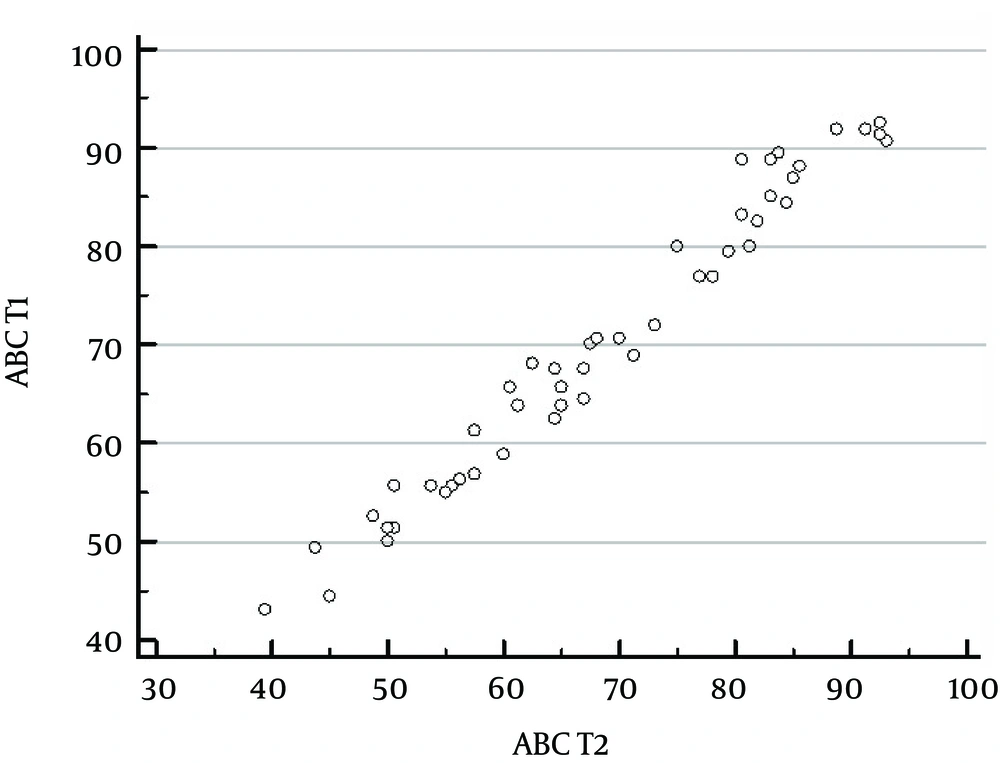
The Bland-Altman plot for ABC-H total score, shown in Figure 1, illustrates that all data points were within the 95% limits of agreement (LOA). Only one out of 50 data points of the ABC-H total score lay outside. A scatter plot was created for the initial and retest ABC-H total score. Perfect linear correlation was observed between them (r = 0.98, P < 0.0001; Figure 2).
4.5. Concurrent Validity
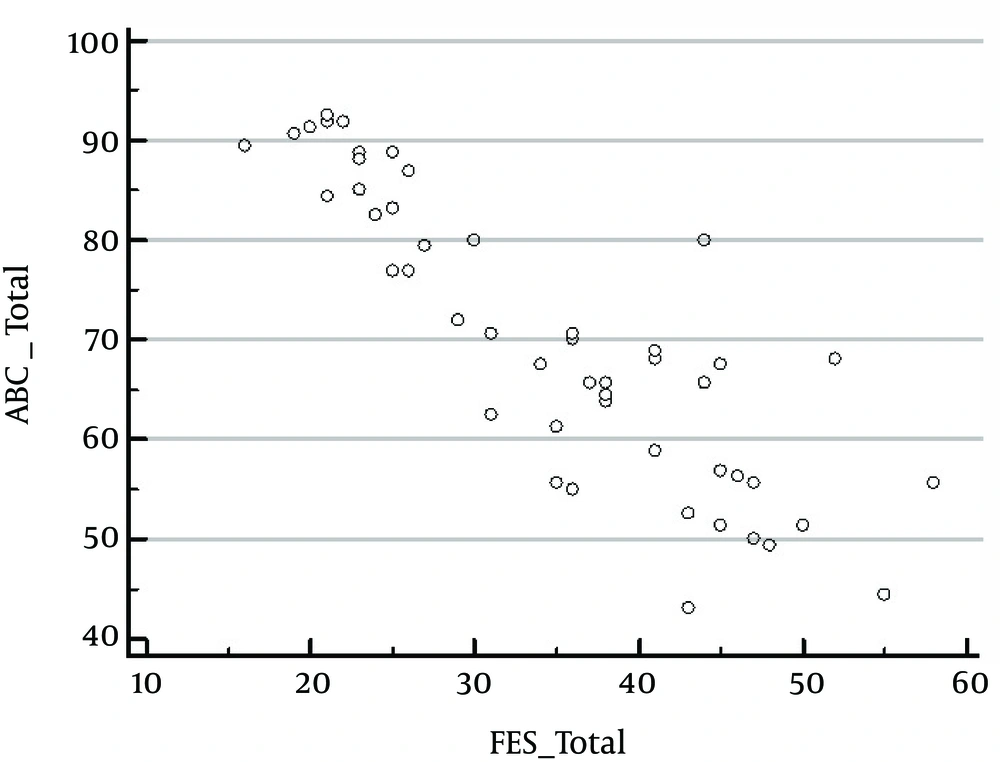
Concurrent validity of the ABC-H, as calculated by Pearson’s correlation coefficient, demonstrated a negative correlation between ABC-H and FES-I total scores (r = -0.85, P < 0.0001), as shown in Figure 3.
4.6. Ceiling and Floor Effect
Only one subject (1%) scored the highest value on the ABC-H scale and no subject (0%) achieved the worst possible score. Overall, no floor or ceiling effect was observed in the ABC-H scale, as these values were found to be less than 15% (31).
4.7. Normative Values
The normative reference values of the ABC-H total score were calculated for mean ± SD and 95% CI of the participants (n = 100) and are presented according to their age category and gender in Table 4.
| Age Groups | N | Mean ± SD | 95% CI for ABC-H | |
|---|---|---|---|---|
| LB | UB | |||
| 60 - 69, y | ||||
| Males | 32 | 82.87 ± 10.38 | 79.12 | 86.61 |
| Females | 10 | 76.93 ± 14.61 | 66.48 | 87.38 |
| 70 - 79, y | ||||
| Males | 30 | 68.50 ± 10.37 | 64.62 | 72.37 |
| Females | 18 | 59.47 ± 12.83 | 53.09 | 65.86 |
| 80 - 86, y | ||||
| Males | 8 | 57.26 ± 7.21 | 51.23 | 63.30 |
| Females | 2 | 47.50 ± 8.83 | 41.25 | 53.75 |
| Total | ||||
| Males | 70 | 73.78 ± 13.45 | 70.57 | 76.99 |
| Females | 30 | 64.50 ± 15.94 | 58.54 | 70.45 |
Normative Data of ABC-H Total Score in Indian Community-Dwelling Older Adults
5. Discussion
Numerous studies in different populations have shown that older people have problems with their balance confidence (32-38), but we have been unable to obtain valid information from the Indian older population owing to a lack of reliable, translated, and culturally adapted tools. Since Hindi is one of the most widely spoken and understood languages in India and around the world (18), there is a need for balance confidence tools to be translated into Hindi. The present study was conducted to translate, cross-culturally adapt, and examine the psychometric properties of the ABC scale into a Hindi version and obtain the normative self-perceived balance confidence scores in the Indian older population. To our knowledge, this is the first published study of such an undertaking. Overall, the findings of the study suggest that the ABC-H scale provides adequate validity and reliability. Further, it helped ascertain the normative value of self-perceived balance confidence scores in Indian older adults.
5.1. Translation and Adaptation
In the present study, we used the translation process suggested by Beaton et al. (20), which is endorsed by the American association of orthopedic surgeons outcomes committee. The guidelines comprise well-defined steps (initial translation, synthesis/reconciliation of the translations, back translation, expert committee review, and pretesting). Eight items were modified, which predominantly involved changes in their wording to more commonly used phrases and to accommodate socio-cultural differences identified between India and Canada, where this scale was developed (10).
5.2. Normative Value
In the current study, the mean normative value of self-perceived balance confidence score was 71 (41.25 - 95.63) among all participants (n = 100), whereas individual item scores ranged from 42.40 to 92.80. Previously, the ABC score in the Canadian population has been reported as 59.6 ± 17.7 (10). In the Chinese population it was found to be 71.6 ± 13.7 (13); and in the Brazilian population it has been observed to be 81.7 ± 10.1 (17). Our results are in accordance with those observed in the Chinese population but are in contrast to the Canadian and Brazilian version. The difference may be explained by the fact that our participants had different physical activity status from the original study. Further, in the present study, 16% were using walking aids (Table 1), whereas most of the subjects in the original study were using walking aids either inside or outside the home. It is important to note that modified item 16 (“…walk outside on slippery pavements”) had the lowest score of 43.8 in the current study, which was higher than that observed (20.7) in the original study (10). The difference may be explained by perceived level of difficulty of walking on ice or on a slippery pavement. Both versions (original and present) recorded the lowest score on item 16, indicating that, in both scales, item 16 presented the most difficult level of self-perceived balance confidence among all the items.
5.3. Internal Consistency
In our study, we observed sufficiently high internal consistency for total score (α = 0.99) and Cronbach’s α = 0.95, if items were deleted. According to Andresen criteria for assessing the psychometric properties of tools of disability outcomes, α ≥ 0.80 means excellent reliability (39). Our findings are in accordance with the original study, in which the ABC scale showed higher internal consistency (Cronbach’s α = 0.96) in community-dwelling older individuals (10). When compared to other studies, our Cronbach’s α was also found to be similar to those observed in different populations, as reported by Steffen and Seney (α = 0.95) (40), Hsu and Miller (α = 0.98) (41), and Talley et al. (α = 0.95) (42). In the present study, Cronbach’s α coefficient for individual items ranged from 0.88 to 0.97, whereas, in the Chinese version, it ranged between 0.71 and 0.88, a range similar to our observations (13). Considering these findings, we can conclude that the ABC-H version has high internal consistency. The higher Cronbach’s α indicated that the items of the ABC-H scale measured a single, unidimensional construct, that is, self-perceived confidence in balance.
5.4. Test-Retest Reliability
The result of this study also showed that ICC of ABC-H was 0.97 for total score, whereas, for individual item scores, ICC ranged from 0.75 to 0.94. In the original version, the test-retest reliability of the ABC scale in community-dwelling older people was reported to be excellent (ICC = 0.92) (10). Similarly, the ICC value of the items in Chinese (13), German (14), British (16), Turkish (15) and Brazilian Portuguese (17) translations of the scale performed on community-dwelling older adults ranged from 0.67 to 0.99. Our results are consistent with these studies, which confirm that it has excellent test-retest reliability.
5.5. SEM and MDC
The standard error of measurement (SEM) provides a value for measurement error in the same units as the measurement itself; thus, it is an indication of absolute reliability. This type of reliability is applicable clinically on a day-to-day basis (27). The SEM observed for the total score in the current study is 2.45, whereas for individual item scores it ranges from 3.60 to 11.7. A study conducted by Nemmers and Miller (43) in community-dwelling elderly people computed SEM as 1.19; whereas in those with Parkinson’s disease, SEM of 4.01 was reported (44). In another study, Botner et al. (45) reported SEM of 6.81 in stroke patients. In the present study, our SEM was slightly higher (1.25 points) than that observed by Nemmers and Miller (43), but lower than that observed in Parkinson’s and stroke populations (44, 45). This difference appears attributable to differences in population and disease severity. Since our results are in agreement with those conducted in community-dwelling elderly subjects but in contrast to those conducted with Parkinson’s and stroke patients, this suggests that error of measurement increases with disease severity and has multi-domain influence.
Minimal detectable change (MDC) is an estimate of the smallest change in score that can be detected objectively by an individual, i.e., the amount by which a patient’s score needs to change to be sure the change is greater than measurement error. MDC can be calculated to varying degrees of confidence, e.g., MDC95 (95% confidence) or MDC90 (90% confidence) (27). MDC95 observed in the current study for the total score was 6.9, whereas, for individual item scores, it ranged from 10.1 to 20.3. Powell and Myers have reported MDC of 21.7 in community-dwelling older adults (10), whereas, in those with Parkinson’s disease, SEM of 11.2 (44) and 13.0 (40) has been reported. Our MDC value was much lower than that observed by Powell and Myers (10), suggesting there could be a demographic difference in the population assessed. The variation of the MDC value in a population with known disease could be attributable to a decrease in individual performance. Because MDC is population- and disease-specific, it will be useful to replicate this study in disease-specific conditions.
5.6. Concurrent Validity
Concurrent validity is the degree to which a test corresponds to an external criterion that is known concurrently (i.e., occurring at the same time). In the present study, a strong negative relationship between the ABC-H and FES-I (r = -0.85; P < 0.0001) was observed. Although both scales are used to measure balance confidence, their scores denote opposite meanings. In ABC-H, a higher score indicates better confidence, whereas, in FES-I, a lower score indicates the same. Owing to this inverse relationship, a strong negative correlation represents excellent concurrent validity. Our results are in accordance with the study done in individuals with dizziness and balance problems, where excellent correlation between ABC and FES-I (r = -0.84) was observed (35).
5.7. Ceiling and Floor Effect
Ceiling and floor effect occurs when a measure’s highest or lowest score is unable to respectively assess a patient’s level of ability. These effects were evaluated by determining the proportion of subjects scoring the maximum or minimum total score of each ABC-H scale. If 15% or more of a group’s scores are extreme (100% or 0%), this represents the ceiling or floor effect. No ceiling or floor effect was observed in the current study, which shows that ABC-H is an appropriate measurement tool.
The study has limited generalizability, in the sense that the sample was collected from one Indian state only, so a more representative sample from different regions should be selected in future studies. Since we have not included older adults (> 86 years) or a diseased population, future study is warranted to determine psychometric properties in different clinical cohorts and to verify the cut-off score of fall prediction in Indian older adults using the ABC-H.
5.8. Conclusions
The findings of this study confirm that the translated and culturally adapted ABC-H scale is culturally relevant and has good internal consistency, absolute reliability, and concurrent validity in older adults. This study provides sufficient evidence to recommend the use of the ABC-H scale in Hindi-speaking older adults to assess their self-perceived level balance confidence.