1. Background
One of the most common health problems and the topic of many studies is mechanical low back pain (1). The prevalence of back pain has been increasing not only in adults but also in adolescents (2). Paravertebral muscular atrophy, changes in lumbar lordosis, disc degeneration, as well as end-plate edema, severe facet joint degeneration, scoliosis, spondylolisthesis, spinal masses are etiological factors of low back pain. Age-related increasing spinal degeneration and muscular atrophy cause low back pain. The etiology of low back pain is determined not only biologically, but also socially and psychologically, and is called as ‘nonspecific nature of back pain’ (3). The negative influence of work stress on low back pain is also known (4). In this study, our aim is to investigate the most common causes of low back pain with magnetic resonance imaging (MRI) in young people under the age of 40 and to determine gender differences if any.
2. Methods
Ethics committee approval was obtained from GOP Taksim Training and Education Hospital before the retrospective study was conducted. The consent form was signed by all authors. 200 consecutive patients between the ages of 17 - 39 who had a lumbar MRI between September - October 2017 were included in the study. Neurosurgery outpatient clinic records confirmed that all patients had chronic or recurrent low back pain. Exclusion criteria were performed due to the trauma and to the history of spinal surgery.
Lumbar MRI examinations of 200 patients were retrospectively evaluated. Spinal mass, spondylolisthesis, disc degeneration, multifidus muscular atrophy and congenital anomalies were investigated. Studied parameters were compared in male and female patients.
2.1. MRI Parameters
In this study, 1.5 T MR Unit (Signa HDxt; GE, USA) and body surface coil were used. Sagittal T1-W FSE, T2-W FSE, and axial T2-W FSE (320 × 256 matrix, 4-mm section thickness, NEX 3) were imaged.
2.2. Visual Evaluation
The evaluation was performed by a single radiologist having 12 years of experience in musculoskeletal radiology. In each patient, vertebra, spinal canal assessment, and the disc levels between the first lumbarvertebra (L1) and the first sacralvertebra (S1) were evaluated separately. Miyazaki classification was used for intervertebral disc degeneration (5). The visual evaluation method applied by Ekin et al. was used for the evaluation of multifidus muscular atrophy (6). Widely accepted Meyerding method was used in the evaluation of spondylolisthesis (7). For lumbar lordosis angle, the angle between the line passing through the upper plate of the L1 vertebra and the line passing through the upper plate of the S1 vertebra in the mid-sagittal MRI was used. Angles below 40 degrees were considered as a decrease and angles above 50 degrees were considered as an increase (8).
2.3. Statistical Analysis
Normality was checked by single sample Kolmogorov Smirnov test, drawing Histogram, Q-Q plot, and box plot charts. The data was presented in the form of mean, standard deviation, minimum, maximum, frequency, and percentage. Age variable between the genders was analyzed by the t-test in independent groups. Nominal variables were assessed by Chi-Square and Fisher exact probability tests. Significance limit was set at P < 0.05 and taken as bidirectional. Analyses were performed by using the NCSS 10 software program (2015; Kaysville, Utah, USA).
3. Results
In this study, 106 female (53%) and 94 male (47%) patients were examined. The mean age of all patients was 30.18 ± 6.12 years (min 17-max 39), the mean age of females was 30.75 ± 6.12 years (min 18-max 39), and the mean age of males was 29.53 ± 6.09 years (min 17-max 39). There was no significant difference between the genders (P = 0.162).
Disc degeneration was observed in 132 patients (66%), whereas it was not found in 68 patients (34%).
3.1. In the Assessment Made According to the Disc Levels (Table 1)
| Variables | L1 - L2 | L2 - L3 | L3 - L4 | L4 - L5 | L5 - S1 |
|---|---|---|---|---|---|
| Normal | 183 (91.5) | 184 (92) | 170 ((85) | 114 (57) | 101 (50.5) |
| Disc bulge | 15 (7.5) | 15 (7.5) | 20 (10) | 59 (29.5) | 63 (31.5) |
| Disc protrusion | 2 (1) | 1 (0.5) | 9 (4.5) | 21 (10.5) | 24 (12) |
| Disc extrusion | 0 | 0 | 1 (0.5) | 5 (2.5) | 11 (5.5) |
| Disc sequestration | 0 | 0 | 0 | 1 (0.5) | 1 (0.5) |
| Total | 200 | 200 | 200 | 200 | 200 |
aL1, first lumbar vertebra; S1, first sacral vertebra.
bValues are expressed as No. (%).
In the L1 - L2 intervertebral disc; 183 (91.5%) patients were normal, 15 (7.5%) patients had degenerative signal loss, and 2 (1%) patients had disc protrusion.
In the L2 - L3 intervertebral disc; 184 (92%) patients were normal, 15 (7.5%) patients had degenerative signal loss, and 1 (0.5%) patient had disc protrusion.
At the L3 - L4 level, 170 (85%) patients were normal, 9 (4.5%) patients had disc protrusion, and 1 (0.5%) patient had extruded hernia.
At the L4 - L5 level; 114 (57%) patients were normal, 59 (29.5%) patients had degenerative signal loss, 21 (10.5%) patients had protrusion, 5 (2.5%) patients had extrusion, and 1 (0.5%) patient had sequestration.
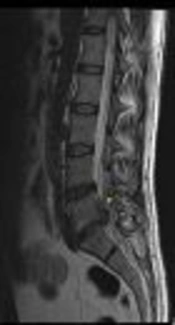
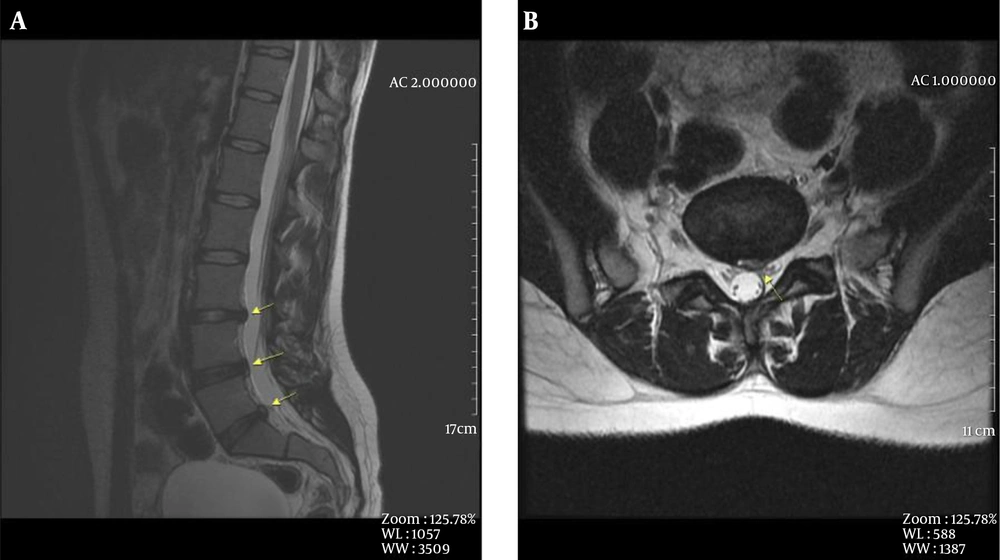
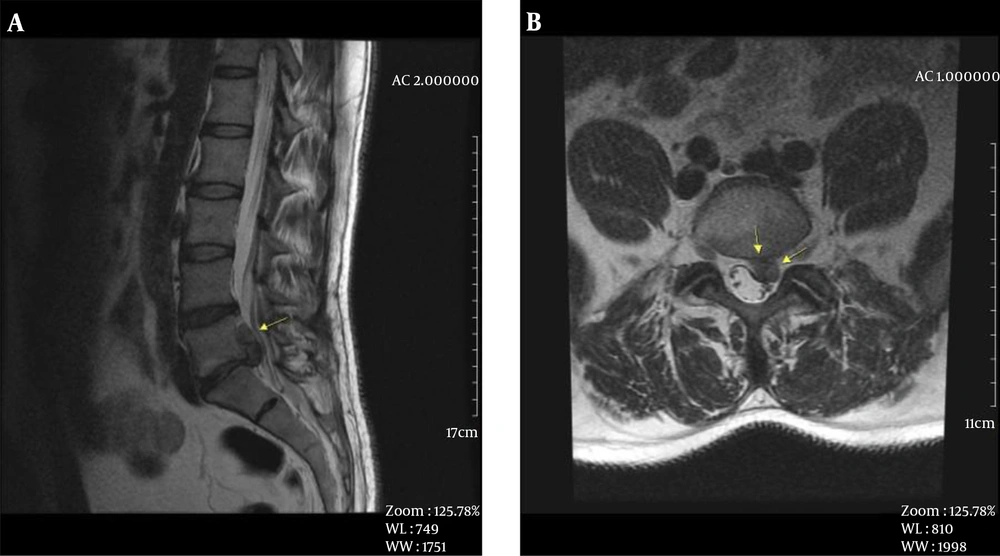
At the L5 - S1 level; 101 (50.5%) patients were normal, 63 (31.5%) patients had degenerative signal loss, 24 (12%) patients had protrusion, 11 (5.5%) patients had extrusion, and 1 (0.5%) patient had sequestration (Figures 1 and 2).
3.2. In the Assessment Made for Disc Hernia Based on Gender
A total of 67 disc degeneration-hernia cases were identified in 106 women (63.2%) an d 65 disc degeneration-hernia cases were identified in 94 men (69.1%). No gender difference was found for disc hernia (P = 0.376 Chi-Square test).
Spondylolisthesis was observed in 8 (4%) of the 200 patients. Of the 8 patients who had spondylolisthesis, 3 were female and 5 were male. There was no significant difference between genders for spondylolisthesis (P = 0.479).
Multifidus muscular atrophy was identified in 54 (27%) patients, while 146 (73%) patients did not have multifidus muscular atrophy. A total of 40 (37.7%) muscular atrophy cases were observed in 106 female patients and 14 (14.9%) muscular atrophies were identified in 94 male patients. Multifidus muscle atrophy was higher in women (P < 0.001, Chi-Square test). The multifidus muscle atrophy was 3.46 more in women (95% CI, OR = 3.46 (1.74 - 6.89).
End-plate edema associated with disc protrusion at L4 - L5 level was observed in a 34-year-old female patient.
Increase in lumbar lordosis: Lordosis increased in 3 female, 2 male, and a total of 5 patients.
Decrease in lumbar lordosis: Lordosis increased in 2 female, 3 male, and a total of 5 patients.
Congenital anomalies: Congenital anomaly was observed in 6 patients, consisting of 3 male and 3 female patients. A 28-year-old female patient had scoliosis and a L4 - L5 congenital block vertebra. Fusion defect in S1 posterior elements was observed in a 24-year-old male and a 20-year-old female patient. Scoliosis and coccyx aplasia were identified in a 25-year-old male patient. Scoliosis was observed in a 39-year-old female patient. In a 19-year-old male patient, segmental anomaly, scoliosis, and tethered cord were identified in the lumbar vertebrae. No spinal mass was observed.
4. Discussion
It is known that 80% of adults have mechanical low back pain at least once in their lifetime (9). Low back pain is also a common health problem in the young population under the age of 40 years. Previous studies in the literature have shown that the age of 40 is a significant turning point. It has been shown that after the age of 40, atrophy significantly increases in paravertebral muscles that provide spine stabilization (6), and lumbar lordosis that is preserved until 40 years of age also increases (8). Disc degeneration also increases after the age of 40 in parallel with muscle atrophy and an increase in lordosis. As a result of all these, low back pain may occur. Well then, what is the most common cause of low back pain in the population under the age of 40 years?
We found that the frequency of low back pain did not change according to the gender in 200 young adults who were consecutively studied. In our study, increase and decrease in lumbar lordosis were statistically negligible. It was found that lumbar lordosis was preserved even in patients under 40 years with low back pain. Multifidus muscle atrophy was only identified in 27% of the patients. Based on the statistical comparison between genders, muscular atrophy was found to be more frequent in females and it was consistent with the literature (6). In our study, the only finding where a significant difference between genders which was found for the young population with low back pain with multifidus muscle atrophy.
In the general population, the incidence of isthmic spondylolisthesis is 4% - 8%, and the incidence of pars defects is 20% (10). The incidence of spondylolisthesis increased after the 5th decade (10). In our study, spondylolisthesis was detected in 4% of the patients and all of these cases were of the isthmic type, Grade 1.
In the assessment in terms of congenital anomalies; segmentation anomaly, scoliosis accompanied by congenital block vertebra, was observed in 4 patients. Fusion anomaly in posterior elements of S1 vertebra not accompanied by neural defects was observed in 2 patients, and this was not associated with low back pain.
The most frequent pathology detected in the lumbar MRI on 200 patients with low back pain was intervertebral disc degeneration and disc hernia. Disc degeneration was observed in 66% of all patients. There was no significant difference between genders in terms of disc degeneration frequency. The pathology is similarly frequent between men and women. In the evaluation based on intervertebral disc level, the most frequent disc degeneration was observed at L5 - S1 and L4 - L5, while the least frequent disc degeneration was observed at L2 - L3 and L1 - L2 levels, respectively. Similarly, extruded and sequestered disc herniation causing narrow channel was most frequently detected at L5 - S1 and L4 - L5 levels. Only 1 patient had an end-plate edema accompanying L4 - L5 disc hernia. End-plate edema is associated with pain (11-13), however, it was detected only in one level in our study.
In the young population, lumbar lordosis was mostly preserved and multifidus muscular atrophy was observed relatively less frequently. On the other hand, disc degeneration or hernia was detected in 66% of patients. These findings suggest that disc hernia is the first occurring and most frequent detected cause of low back pain. The most mobile L4 - L5 and L5 - S1 levels have been affected. Based on these observations, it can be concluded that as a result of wrong or overstrained movements due to the living conditions, working conditions and individual habits, intervertebral discs are the first and most frequently affected body parts. Living conditions related to the occupational groups or regional factors may be effective in this respect. Numerous studies have been published investigating occupational groups and geographical regional characteristics that may be associated with low back pain (10).
The limitations of this retrospective study include lack of clear information regarding the occupations of the patients. However, our patients live in the same region and have similar socioeconomic conditions. Secondly, we didn’t know how long the patients had low back pain duration. This point may change the results. To optimize, we tried to choose only chronic and recurrent pain, however, it is based on patient records. Finally, the results of this study involving the young patient group cannot be generalized for all ages. New studies can be conducted to include information regarding occupations, working conditions, and daily activities of the patients.
4.1. Conclusion
In conclusion, intervertebral disc herniation can be shown as the most common reason for low back pain in women and men in the young population under the age of 40. Lumbar lordosis is preserved in the young population. Although its frequency is lower compared to elderly, multifidus muscular atrophy is more frequent in women.