1. Background
Osteoarthritis (OA) is the most prevalent joint disease. It is so common that almost 4 million people experience OA, and it is the cause of 50% total disability in Spain (1, 2). The economic impact is such that the direct cost of OA in Spain is 4738 million Euros per year. Therefore, OA becomes an important problem of public health (3). Moreover, OA produces pain, decreases function, and consumes a great amount of limited health resources. The emotional, social, and physical aspects are affected in patients, impairing their quality of life (QoL) (4).
Osteoarthritis influences cartilage at the involved joint; as a result, articular space narrows, and bone sclerosis, subchondral cysts, and osteophytes appear (4-7). Therefore, diagnosis is based on clinical and radiological signs and symptoms (8, 9). Knee OA is a multifactorial disease (4, 5). Risk factors include trauma, obesity, and recently, low-grade chronic inflammation (5-7, 10, 11).
The future challenge in the management of knee OA is to discover early tools for diagnosis, progression and monitoring of the disease, and to find effective therapeutic interventions. Biomarkers are among possible tools (12). Since OA is related to inflammation, inflammation biomarkers, such as C-reactive protein (CRP), Erythrocyte Sedimentation Rate (ESR), and pro-inflammatory cytokines (IL-1β and IL-6) have been used to determine such relationship (8, 13-16).
In knee OA, the treatment goals in the short term are to ameliorate symptoms by symptomatic slow action drugs for OA (SYSADOA), and on the long term to diminish/revert articular damage and joint destruction by disease modifying drugs for OA (DMDOA) (3). The osteoarthritis research society international has suggested non-pharmacological, pharmacological, and surgical recommendations for the treatment/management of knee OA (2). Total knee arthroplasty is the last alternative in advanced knee OA patients, and although it is an invasive and expensive procedure with a 95% rate of survival at 10 years, it might have complications (4, 17, 18).
Several researchers worldwide and many years of clinical experience have indicated the fact that Ozone is capable to modulate inflammation (1, 19). In case of knee OA, several studies state that Ozone is capable of ameliorating pain and improving function and quality of life (SYSADOA effect) (2, 3, 5). One recent study by Fernandez-Cuadros et al., even stated that Ozone was capable of slowing/reverting knee OA progression in a 2-year follow-up study (DMDOA effect) (3). However, to the best of the author’s knowledge, there is no study that has evaluated the effectiveness of ozone on biomarkers of inflammation, such as CRP and ESR on knee OA human subjects. There is only one report by Chang et al., who stated that Ozone could inhibit pro-inflammatory cytokines (IL1 and TNF-α) in an animal model (20).
The objective of this study was to evaluate if Ozone is capable of decreasing biomarkers of inflammation (CRP/ESR), ameliorating pain, and improving function and quality of life in knee OA patients.
2. Methods
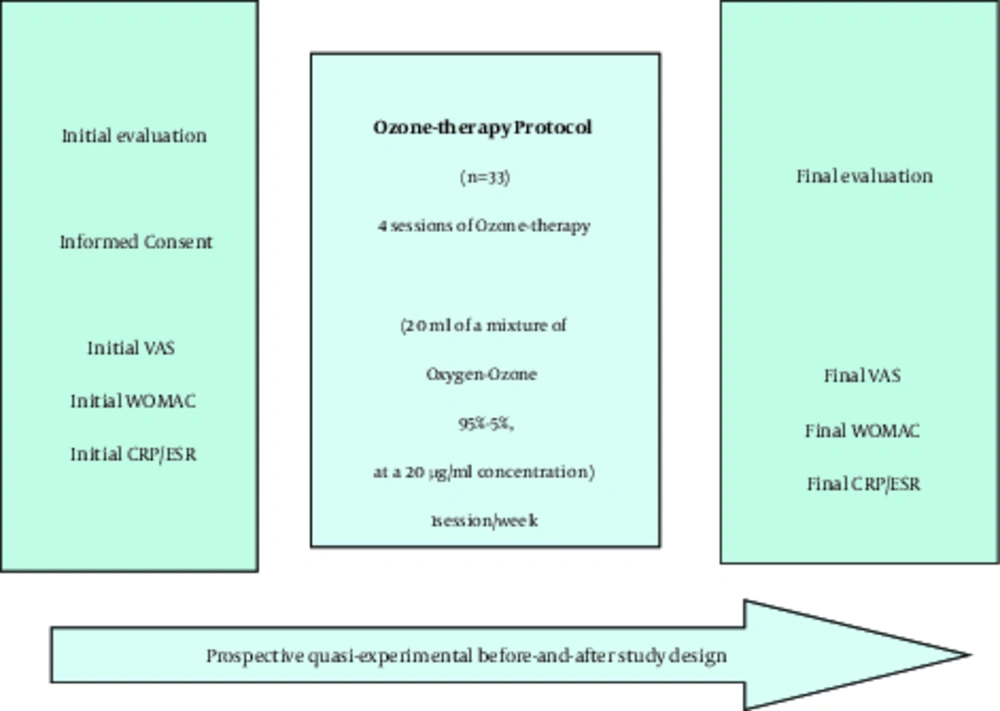
A total of 33 patients were enrolled in a prospective quasi-experimental before-and-after study. Knee OA patients with a Kellgren-Lawrence (KL) grade of 2 or more, who attended the Santa Cristina’s University hospital, with clinical symptoms (pain, stiffness, and loss of function), demanding conservative treatment, and in whom previous symptomatic treatment had failed, were included in the study. The study was conducted from January to November 2017, and it was authorized by the ethical committee of Santa Cristina’s University hospital (Figure 1).
2.1. Inclusion Criteria
1, knee OA KL patients graded 2 or more; 2, pain greater than 3 on visual analogical scale (VAS), who had failed any other conservative treatments (NAIDs, rehabilitation or physical therapy); 4, willingness to participate and not being a candidate for knee arthroplasty replacement.
2.2. Exclusion Criteria
1, allergy to Ozone (2, 3, 5); 2, incomplete biochemical analysis (CRP/ESR); 3, incomplete ozone therapy treatment protocol; and 4, absence from any of the questionnaires applied (VAS or WOMAC).
In the initial evaluation, the goals of treatment, procedure, indications and contraindications were explained, while initial biochemical evaluation (CRP and ESR analysis) was performed, informed consent was signed and outcome scales (VAS and WOMAC) were provided before the protocol (Figure 1).
The Ozone protocol consisted of 4 sessions (1 session/week) of an intra articular infiltration of a medical mixture of Oxygen-Ozone (95% to 5%) at a 20-ug/mL concentration. The skin area was cleaned with 1% chlorhexidine and anesthetized with ethyl chloride spray. The medical generator used was Ozonosan α-plus®. This equipment provided a 20-mL volume of 95% to 5% Oxygen-Ozone mixture that was introduced to a 20-mL silicone-coated syringe of 3 bodies. A Quincke needle of 27G, 4 cm was used to deliver Ozone to the joint.
Once the patient lied on the bed, the medical Ozone mixture was infiltrated on the knee on the superior and lateral side of the patella. If the infiltration is not performed in the joint, redness and pain appears after infiltration, however, these complaints disappear in a few minutes. The infiltration of Ozone treatment protocol on patient’s knees was applied by the authors of the study.
After 4 sessions of ozone protocol, the final evaluation was accomplished, biomarker analysis, VAS and WOMAC Scales were applied, and adverse effects (if any) were registered. Serum levels of CRP and ESR were measured at baseline and at the end of the protocol treatment. The minimal measurable concentration of CRP is approximately 0.2 mg/dL and its coefficient of variation in expert technicians is 5.8% to 6.3% (21).
To perform the analysis of biochemical markers of inflammation, about 8 mL of venous blood was taken by arm venipuncture in a sterile vial. Five milliliters of blood was collected in a tube without anticoagulant, and serum was separated by centrifugation at 3500 rpm for 20 minutes. The level of CRP on serum was determined by the MULTIGENT CRP Vario assay (CRP Va), which is a latex immunoassay developed to measure accurately and reproducibly blood CRP levels in serum and plasma (CRP VARIO, Italy). The rest of the blood sample (3 mL) was collected in another sterile tube containing potassium EDTA anticoagulant for measurement of ESR by an automated system. The Ves-Matic Cube 30 (Diese, Italy) determines ESR, directly in closed tubes with EDTA blood samples using an infrared sensor to measure the level of opacity of the column of blood in the vertical position. The results obtained after 33 minutes of analysis corresponded to the Westergren method results after 60 minutes of sedimentation (Westergren method was the reference method).
The symptoms severity was measured by VAS and WOMAC scales. The VAS is a pain score graded from 0 to 10. A greater value is related to greater pain and vice versa (22). The WOMAC Index is a scale that evaluates pain, stiffness, and function, all in 24 questions. Each answer has 5 possible options: none, mild, moderately severe, and extreme. Pain includes 5 items (graded from 0 to 20), stiffness 2 items (graded from 0 to 8), and function 17 items (graded from 0 to 68) (22). Any change in the scores of the WOMAC index greater than 6% was considered as being clinically important. These changes represent, for WOMAC-pain subscale 1.2 points, for WOMAC-stiffness subscale 0.5 points, and for WOMAC-function subscale 4.1 points (23).
To radiologically classify knee OA, the KL scale was used. The KL grades are defined as follows: 0º, no radiological changes; 1º, doubtful osteophytes; 2º, osteophytes are present; 3º, joint space narrowing is observed; 4º, impingement, subchondral sclerosis, subchondral geodes, and marginal osteophytes are present.
Statistical analysis was performed by the use of SPSS® version 20.0. Frequencies and percentages were used to evaluate qualitative variables; while for the evaluation of quantitative variables, means and standard deviation were employed. The t-student test was the tool used for the evaluation of change before-and-after the treatment of quantitative variables. The X2 test, if necessary, was employed to evaluate qualitative variables. The level of significance was 95% (P = 0.05).
3. Results
In this study, 33 patients were evaluated. Mean age of the patients was 68.18 ± 8.43 years. Female patients accounted for 75.7% (n = 25), while male patients corresponded to 24.3% (n = 8), with a female:male ratio of 3:1 (Table 1).
| Variables | Value |
|---|---|
| Age, y | 68.18 ± 8.43 |
| Female gender, n (%) | 25 (75.7) |
| Male gender, n (%) | 8 (24.3) |
| Female: Male ratio | 3:1 |
| OA KL 2º | 22 (66.7) |
| OA KL 3º | 8 (24.2) |
| OA KL 4º | 3 (9.1) |
| CRP, mg/dL | 0.33 ± 0.32 |
| ESR, mm/h | 15.06 ± 12.09 |
| Pain VAS | 7.33 ± 1.31 |
| WOMAC pain score | 14.84 ± 2.77 |
| WOMAC stiffness score | 3.06 ± 1.95 |
| WOMAC function score | 41.15 ± 12.58 |
The most frequent radiological KL grade was 2º (n = 22, 66.7%), followed by 3º grade (n = 8, 24.2%), and 4º grade (n = 3; 9.1%) (Table 1).
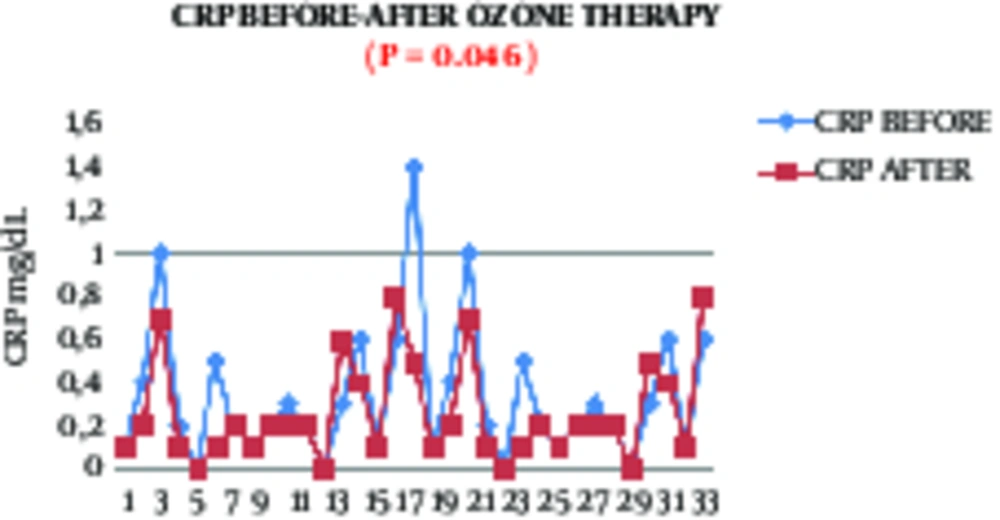
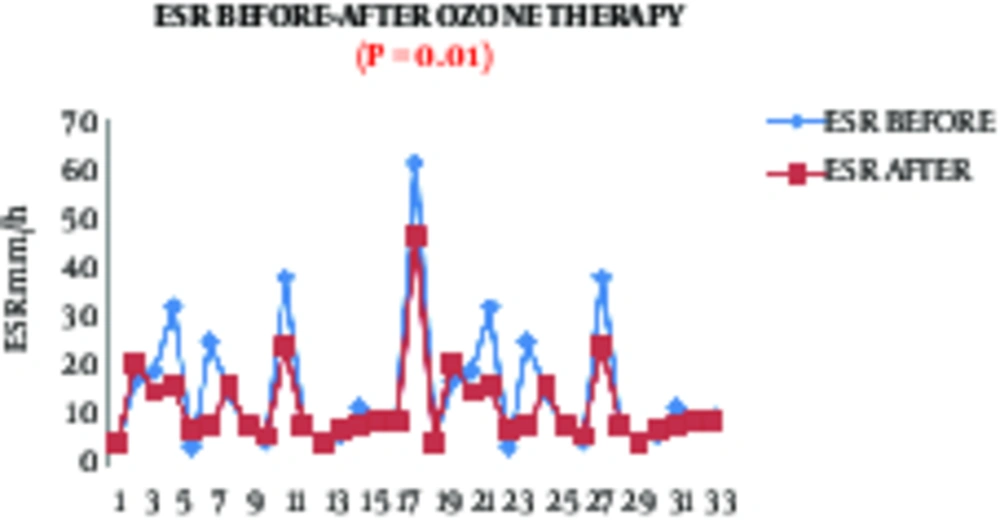
With respect to outcome variables, biomarkers of inflammation decreased significantly (P < 0.05) after Ozone therapy. The CRP diminished from 0.33 ± 0.32 mg/dL to 0.25 ± 0.23 mg/dL (P = 0.0456) (Table 2, Figure 2). The ESR decreased from 15.06 ± 12.09 mm/h to 11.81 ± 8.32 mm/h (P = 0.01) (Table 2, Figure 3).
| Outcome Variables | Before | After | P Valueb |
|---|---|---|---|
| CRP, mg/dL | 0.33 ± 0.32 | 0.25 ± 0.23 | 0.0456 |
| ESR, mm/h | 15.06 ± 12.09 | 11.81 ± 8.32 | 0.0100 |
| Pain VAS (0 - 10) | 7.33 ± 1.31 | 2.84 ± 1.76 | 0.0000 |
| WOMAC pain (0 - 20) | 14.84 ± 2.77 | 5.69 ± 3.53 | 0.0000 |
| WOMAC stiffness (0 - 8) | 3.06 ± 1.95 | 1.15 ± 1.3 | 0.0000 |
| WOMAC function (0 - 68) | 41.15 ± 12.58 | 22.3 ± 11.64 | 0.0000 |
Effects of Ozone on biomarkers of Inflammation (CRP and ESR) and on Symptoms Severity (Measured by VAS and WOMAC Scales) in Knee OA Patients (n = 33)a
Regarding symptom severity in knee OA, measured by VAS and WOMAC scales, Ozone therapy significantly improved each and every variable (P < 0.0001). Before treatment, pain measured by VAS was 7.33 ± 1.31 points and significantly decreased to 2.84 ± 1.76 points (P < 0.0001) (Table 2). Before the intervention, WOMAC-pain subscale was 14.84 ± 2.77 points, and diminished to 5.96 ± 3.53 points (P < 0.0001), WOMAC-stiffness subscale was 3.06 ± 1.95 points and decreased to 1.15 ± 1.3 points (P < 0.0001), and WOMAC-function subscale was 41.15 ± 12.58 points and improved to 22.3 ± 11.64 points (P < 0.0001) (Table 2).
4. Discussion
To the best of the author’s knowledge, this is the first study that stated that Ozone decreases biomarkers of inflammation, namely CRP and ESR in human knee OA patients, and the diminishing comes in line with a clinical improvement on symptoms severity, such as pain, stiffness, function, and QoL.
In the current study, and because of economical limitations, the researchers intended to evaluate the effectiveness of Ozone on knee OA patients by the use of acute phase proteins/reactants of inflammation, a hallmark of knee OA (1, 5, 24-33). These biomarkers are cheap, easy to perform, and widely used in clinical practice. The objective of this study was to demonstrate that CRP/ESR biomarkers of inflammation decrease after Ozone treatment, since it was hypothesized that Ozone improves pain, function, stiffness and QoL, and many studies suggest that ozone is capable of ameliorating inflammation (5). The rationale to evaluate CRP/ESR is that inflammation biomarkers may predict outcomes in OA. Elevated hs-CRP predicts loss of cartilage in knee OA and poor results after total knee arthroplasty.
Biomarkers of inflammation used in the study were CRP and ESR. These biomarkers are recognized as acute phase reactants or proteins. They indicate an inflammatory state, as in the case of rheumatic diseases. Erythrocyte Sedimentation Rate is cheap and commonly used in clinical practice. It mainly reflects fibrinogen concentration. Furthermore, CRP shows no variation with age, neither with erythrocytes morphology, nor with other protein variations. During inflammation, CRP concentration increases by 1000 folds; on the contrary, ESR increases by 2 to 5 folds. In an inflammatory process, such as orthopedic surgery, CRP reaches its maximum level at 24 to 48 hours and normalizes by the next week. On the contrary, ESR value is elevated after a week, and normalizes in the next 6 weeks (13).
The current findings and several other facts suggest that the development of OA is usually accompanied by inflammation (16). Epidemiological studies suggest that the severity and progression of tibiofemoral cartilage loss are more frequent and severe in patients with inflamed synovial fluid (34). Higher levels of IL-1β and TNF-α, which are mediators of inflammation, are found in the progression of the disease (16). Several studies have observed that increased CRP levels are related to prevalence and progression of the knee or hip OA (16). With respect to OA, elevated CRP levels are related to synovial fluid IL-6 levels and to synovial infiltration, as well as with symptoms of pain and stiffness, radiographic grading, and disease progression (35).
Many researchers worldwide have suggested that not only IL-6, yet CRP and ESR are closely related to radiographic knee OA, symptoms severity, and the progression of the disease (8, 36-44). These biomarkers suggest that low-grade inflammation might be a direct pathway in structural and symptomatic changes on knee OA (21).
All the presented data suggest that inflammatory biomarkers, such as CRP and ESR, might be a key factor in knee OA pathogenesis; they could serve as OA predictors and as outcome variables. Their change may indicate the effectiveness of the current intervention (Ozone treatment). With this in mind, it could be understood why in the present study CRP and ESR were slightly elevated; and how Ozone was capable of diminishing such biochemical levels, together with symptom relief. This observation also comes in line with previous studies (Fernandez-Cuadros et al), in which important and significant amelioration of pain, rigidity; and improvement on QoL was observed after Ozone treatment. Indeed, for the first time, the findings correlate clinical improvement with biochemical improvement in knee OA patients. The current study is in accordance with that of Zhu et al., who stated that hs-CRP was significantly associated with WOMAC knee pain and its changes (21).
From the previous discussion, it can be inferred that the decrease of CRP and ESR as markers of inflammation, reflect the effectiveness of Ozone treatment on knee OA management. Therefore, in the current study it was observed that Ozone ameliorates pain and stiffness, improves pain and function, and decreases CRP and ESR values. This study also showed a direct relationship between inflammation and symptom severity in knee OA. Before treatment, patients presented a high score on VAS and WOMAC scales, and high values of serum CRP and ESR. After the intervention (Ozone treatment), lower scores on VAS and WOMAC scales were observed, which correspond to symptoms alleviation, and were related to lower CRP and ESR values.
An important limitation of the study was the absence of a control group. The small sample size (n = 33) limited the establishment of a control group. Indeed, because of ethical considerations, the researchers pursued to treat all patients with the treatment protocol, based on decades of clinical experience in the management of Ozone for pain and inflammation. This quasi-experimental before-and-after study intended to add clinical-based evidence and solve the lack of control group. That is the main reason why this kind of study was designed. In the before-and-after evaluation, a change after the intervention was expected to be the direct effect of Ozone on the treatment group.
Another important limitation subsides in the fact that the specificity of biomarkers of inflammation on knee OA was limited, because they are compromised in several inflammatory disorders. Despite much active research on biomarkers in OA, no single biomarker has been found to be the gold standard or sufficiently well validated and recognized as a valuable tool for diagnosis, prognosis, investigation and/or evaluation of effectiveness on knee OA (8).
Economic constraints limited the use/evaluation of CRP/ESR as general markers of inflammation. Despite the sample size, biomarker specificity of CRP and ESR, and the economic limitations of this study, such limitations do not affect the observations obtained from this study. The reduction of inflammation biomarkers means that inflammation might constitute an important factor in the progression of knee OA, although further research on this issue must be accomplished. Future studies should be performed on the effectiveness of Ozone to reduce specific inflammatory cytokines in serum or synovial fluid, such as Interleukin (IL)-1, IL-6, Tumor Necrosis Factor (TNF)-α, and Interferon (IFN)-Υ.
4.1. Conclusion
In the light of the current results, it could concluded that Ozone is capable not only of decreasing pain and stiffness and improving function and quality of life in knee OA patients, yet it could also decrease biomarkers of inflammation such as CRP and ESR.