1. Introduction
Musculoskeletal (MSK) disorders are very prevalent in the general population, regardless of sports and work activities. There subsides the need to determine the most accurate diagnostic technique for such entities (1).
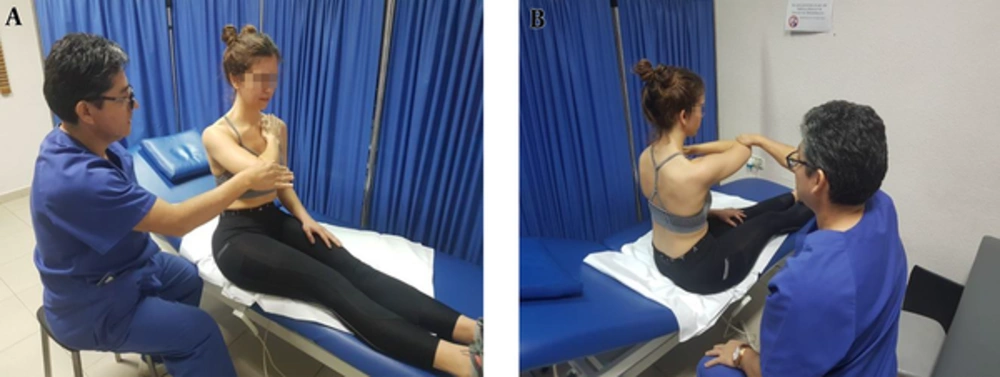
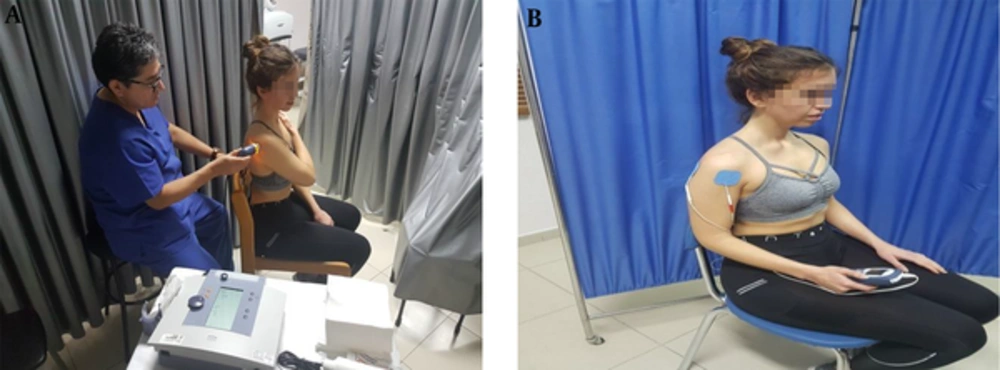
Patients are usually treated based on clinical signs and symptoms as well as on clinical evolution (Figure 1). Treatment usually includes rest, ice, compression, and elevation in the short term, with physical therapies (thermotherapy, electrotherapy, physiotherapy, magnetotherapy, and ultrasound therapy) in the long term (Figure 2). When there is no positive response to treatment, or a more complex or severe disease is suspected, a more accurate diagnosis is needed (1, 2).
This review article will propose different diagnostic techniques (radiography, magnetic resonance imaging and ultrasound). Due to the versatile properties of US, we propose US as the first diagnostic, prognostic, and evolution tool in the rehabilitation specialist’s setting.
2. Review of the Literature
2.1. Imaging Techniques
In the last century, radiography, arthrography, and computed tomography were the most important techniques for diagnosis of the MSK system. MRI constituted a break point for the diagnosis of MSK disorders. The main advantages are based on the multiplane capacity, discrimination between different tissues, and because it is not operator dependent. MRI is very objective and images obtained may be evaluated by different specialists (radiologists, traumatologists and rehabilitation specialists).
In the 1970s, US were used to diagnose shoulder pathology (3). From that time, US advanced mainly because new high frequency linear probes, capable of determining the spatial resolution of 150 - 200 μm, were designed, while MRI could only discriminate at 450 μm (4-7). High resolution of US is based on the acoustic impedance of several tissues. US can diagnose small tissue defects, tiny calcifications, and small foreign bodies. These properties exceed by far the resolution of MRI.
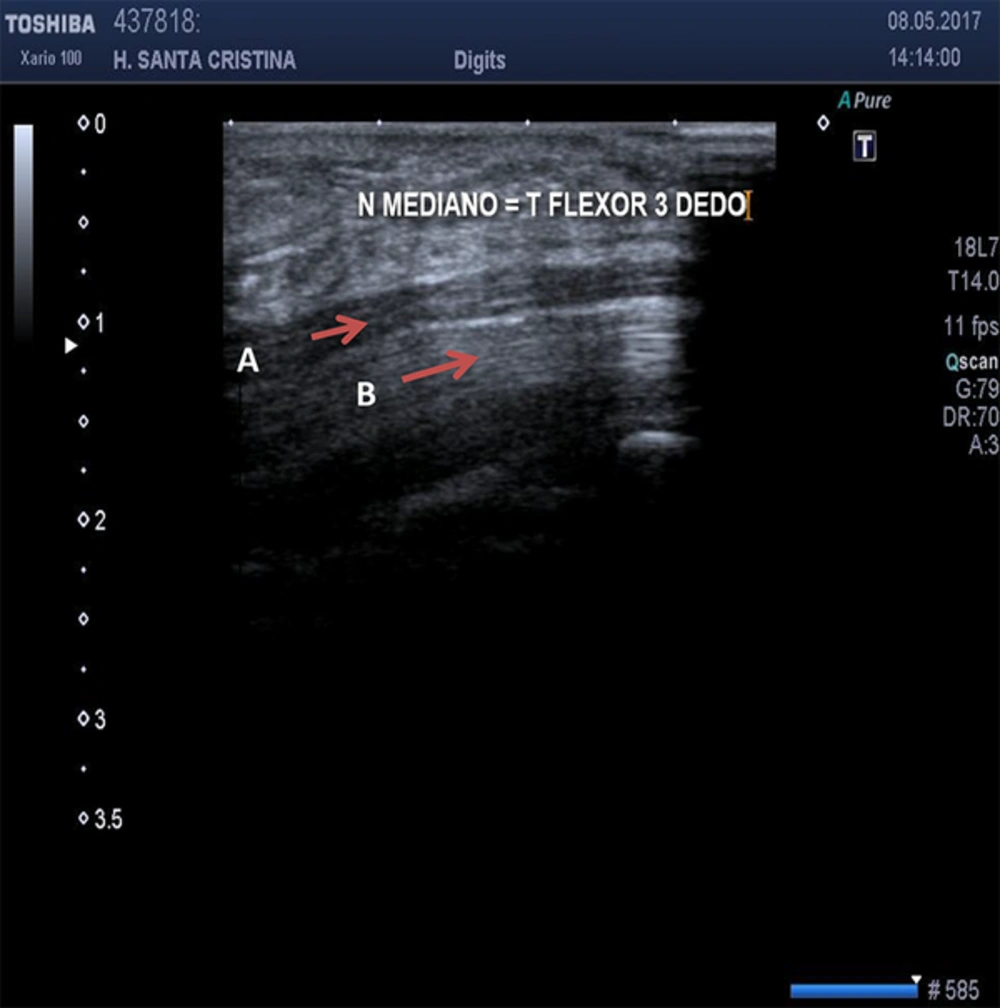
US can properly evaluate structures of the locomotor system such as tendons, muscles, and ligaments. It can differentiate the fascicular pattern of nerves if compared to the fibrilar pattern of tendons, because of anechoic lines observed due to the connective tissue that encircles such structures (8, 9). In superficial structures such as the median nerve at the wrist, the differences can be observed in much more detail if compared to flexor tendons of the wrist (Figure 3). Muscles can be visualized as “feathers of a bird” in its longitudinal view or as “sky with stars” on its transversal view.
2.2. Disadvantages of US
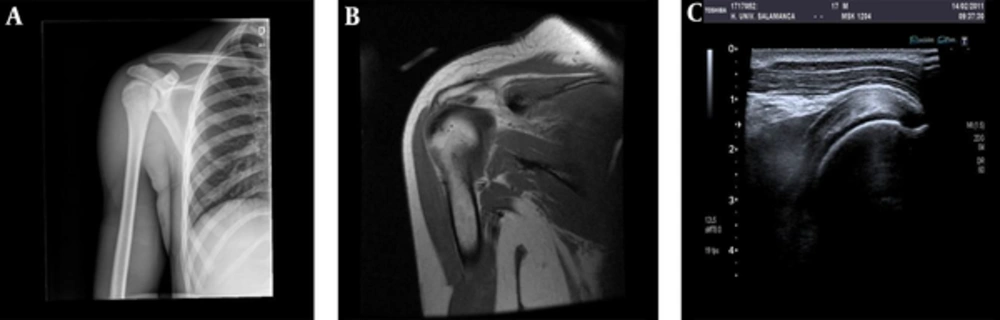
The main disadvantage of US imaging is the operator dependent property. It is required a long-term training course to develop accuracy on diagnosis (9, 10). It is very difficult to evaluate imagens obtained by linear probes, due to the fact that they do not look as clear on an MRI. The sonoanatomy of MSK structures differs a lot from MRI. MRI images have an anatomic representation; however, on US, images are harder to understand (Figure 4). This characteristic makes the technique underestimated due to ignorance (1).
2.3. Advantages of US
US evaluation can be dynamic, helping to determine disorder and extent of the alteration (11). It is interactive; the patient can explain where and when evaluation elicits pain (by sonopalpation) in order to examine more thoroughly the region under evaluation. If sonopalpation produces compression on anatomical structures, its changes may differentiate solid to cystic masses.
No formal contraindication to US is observed, if compared to a MRI (12, 13). Doppler on US might help us diagnose inflammation, degeneration, and to follow-up the evolution of such processes (4, 14). This differentiation is very relevant, due to the fact that the goal of treatment and the prognosis changes substantially. If during evaluation there are anatomical variations, a contralateral comparison can help us in the confirmation of the diagnosis (9).
Ultrasounds can be diagnostic (due to all previous properties) and therapeutic. US can guide on interventional procedures (9). Availability and accessibility are other characteristics present in US evaluation if performed by Rehabilitation specialists. US are cheaper in terms of time and money and faster in performance, if compared to a MRI, by 25% - 30% (6).
Rehabilitation specialists diagnose MSK pathologies based on clinical signs and symptoms. US, in the hands of a rehabilitation specialist, would provide clinical, anatomical, and technical integration to the evaluation, making the process faster and more efficient. The use of clinical guides on the evaluation of different locomotor structures will add accuracy on the diagnostic-prognostic and therapeutic process, better if performed by the rehabilitation specialist (9, 12, 13, 15).
2.4. US Indications on MSK Pathologies
Shoulder: An US is the preferred technique in the evaluation of a painful shoulder. It might diagnose subacromial impingement, rotator cuff pathology, and tendonitis or partial rupture (2, 16-18) (Figure 5). It might diagnose compression of the supraescapular nerve due to ganglions or cysts. US is not useful for the diagnosis of labrum lesions.
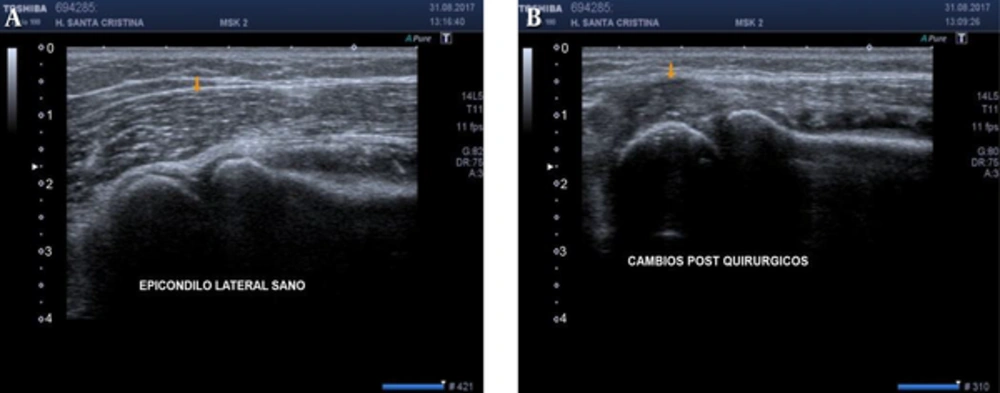
Elbow: US might diagnose overuse diseases such as medial or lateral epicondylitis (Figure 6). Other tendons such as biceps or triceps might also be evaluated.
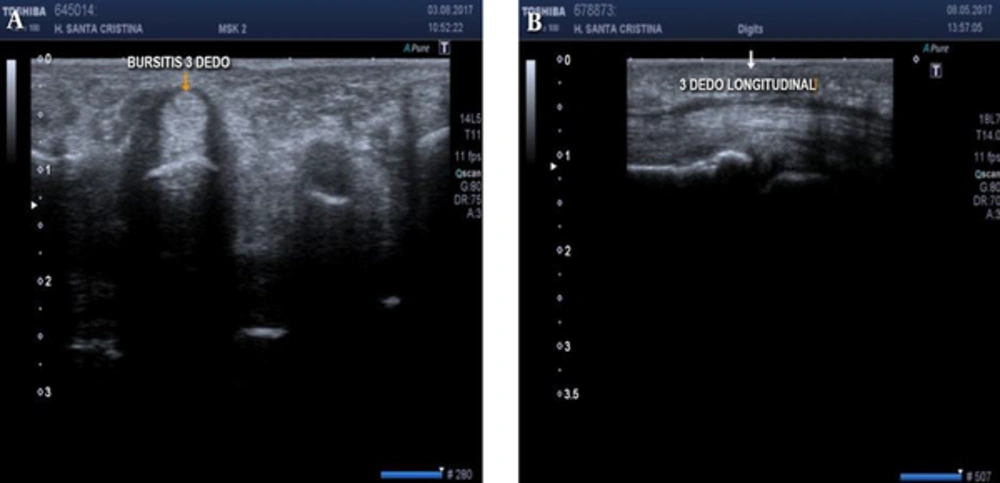
Wrist and hand: US might accurately evaluate de Quervain’s tendonitis. The friction of tendons in the first flexor compartment can be dynamically observed. Tenosynovitis (liquid around tendons) may be clearly observed (19) (Figure 7). On the evaluation of the median nerve at the wrist, signs of compression before the flexor retinaculum might be clearly observed.
Hip: US is the gold standard for the evaluation of dysplasia of the newborn. Synovitis, trigger hip, and sciatic and femorocutaneous nerves can also be evaluated.
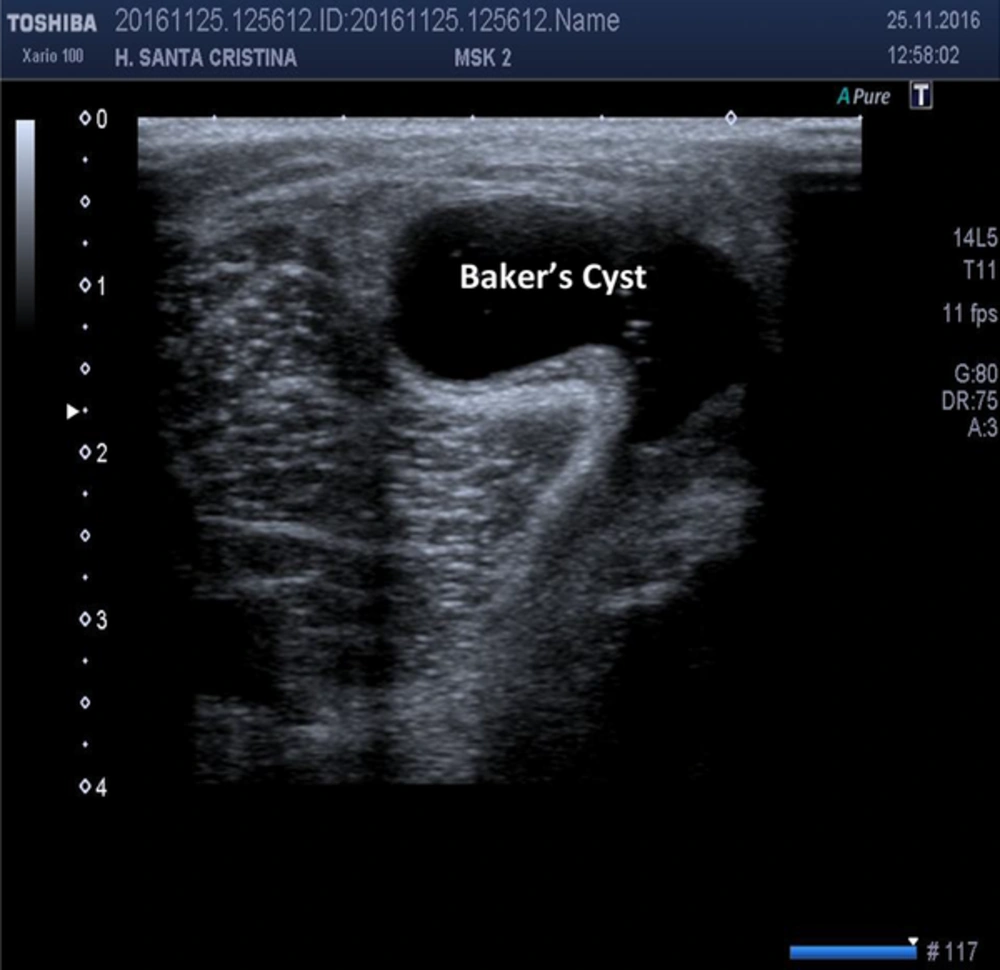
Knee: Bursitis, inflammation, and Baker´s cyst can be clearly evaluated by US scan. Baker’s cyst was the first indication for evaluation of US on MSK pathology in the later 1974 (20) in an attempt to differentiate from thrombophlebitis (Figure 8). Lateral ligaments and tendons might be clearly observed.
Ankle and foot: Instabilities due to a lesion of ligaments can be diagnosed by US evaluation. Plantar fasciitis and Morton Neuromas are observed by an US scan.
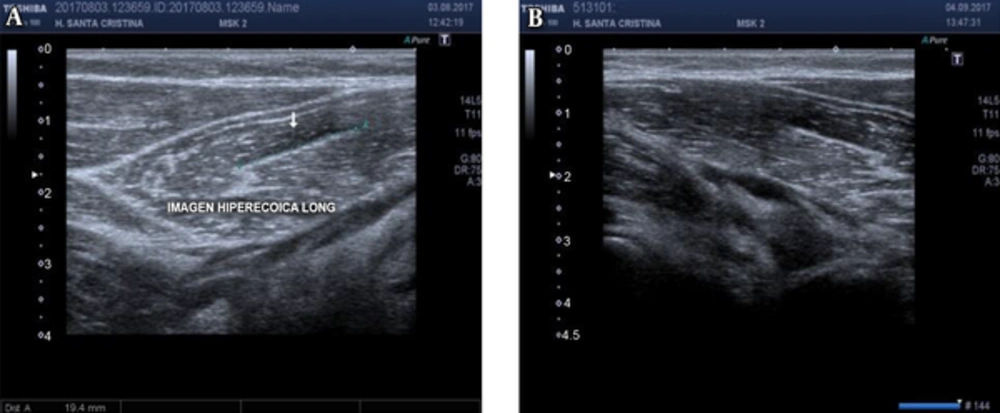
Muscle: US might at initial evaluation and in the follow-up of muscle lesion or partial ruptures (Figure 9). US is useful for the diagnosis, localization, prognosis, and sequels, if any (hematoma, ossificans myositis, scars, herniation, and so forth) (21).
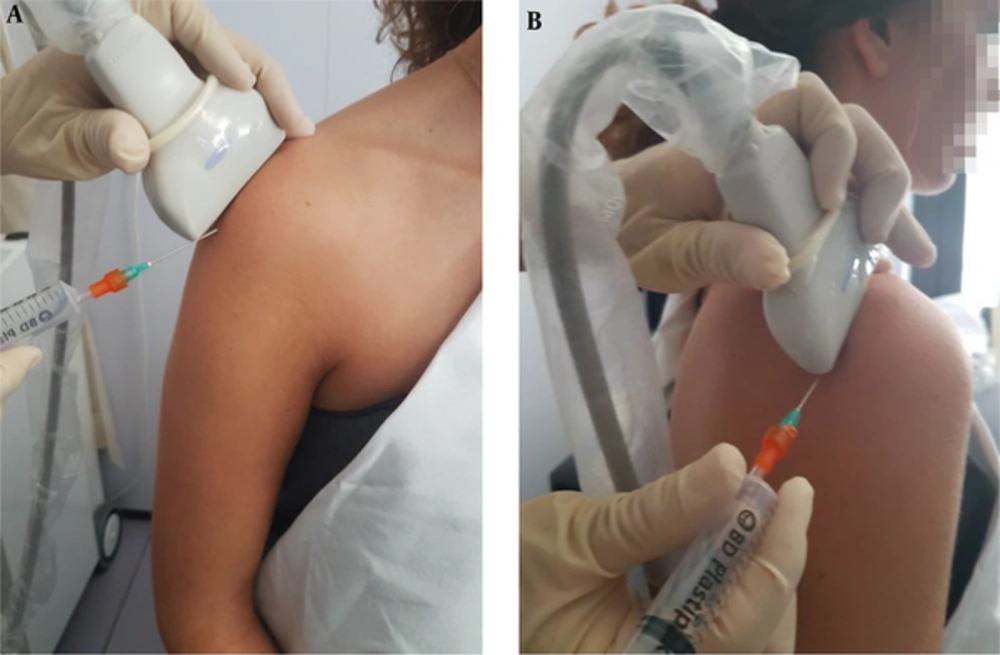
Guided US: Several procedures can be performed by the use of US: biopsies, infiltrations (Figure 10), arthrocentesis, tenotomies, prolotherapy (Ozone, dextrose), visco supplementation (hyaluronic acid), barbotagge (calcifying tendonitis), extraction of foreign bodies, ganglion sclerosis, and the like (22).
3. Discussion
US is a technique useful for the evaluation of muscle and tendons. US accuracy is similar or superior to MRI. US has no formal contraindication. US are efficient and in constant advance. US is accessible, cheap, dynamic, and interactive. US may guide invasive procedures.
Although the learning curve is long and it is operator dependent, protocol guides may improve US accuracy in MSK diagnosis.
A clinical evaluation and an US evaluation increase the diagnosis, prognosis, and follow-up on MSK disorders. US in the hands of a Rehabilitation specialist would provide clinical, anatomical, and technical integration to the evaluation, making the process faster, and more efficient.
As a resume, the use of US in the hands of a Rehabilitation specialist may provide an integral management that includes diagnosis and treatment all in one single visit. US is a fast, non-invasive and cost-effective technique if executed after a proper learning curve.