1. Background
Osteoarthritis (OA) is the most common joint disease (1) and it mainly influences knee and/or hip joints (2). It is so prevalent that almost four million people are affected by this illness, and it represents almost 50% of the total disability in Spain. Osteoarthritis represents a major problem for public health and in Spain the direct cost is 4378 million euros per year, which is 0.5% of the gross domestic product (1, 2).
Osteoarthritis causes pain, disability, and impaired quality of life (QoL) (2). Osteoarthritis of the hip and knee is considered as the 11th contributor to global disability and 38th cause of years lived with disability (3). It is so common that two thirds of people older than 50 years old show radiological signs in at least one joint and its clinical presentation in Spain in people over 70 years old is almost one third of the population (4). It is multifactorial and is related to aging, more frequent in obese patients with comorbidities and in women (2, 5-7). As OA is a degenerative disease, it is expected that the economic impact of the disease will improve in western societies, such as Spain (1, 2).
Furthermore, OA pathogenesis is complex and related to the poor ability of cartilage healing because of its avascular and a lymphatic nature (8). Typical clinical symptoms include pain and stiffness, particularly after prolonged activity, and loss of function is a consequence (9). Osteoarthritis of the joints includes cartilage degradation, subchondral bone thickening, osteophyte formation, synovium inflammation, and ligament degeneration (9). As a result of these changes, joint space narrows, sclerosis and osteophytes show up, and subluxation and joint deformity are observed (9). Therefore, OA diagnosis is clinical and radiological (1, 2). To date, the management of OA subsides on pain relief, function recovery, and QoL improvement (10). Many pharmacological and non-pharmacological treatments have been proposed (1, 2, 8). Most of these approaches are effective in the short-term (11), however, there is no known cure for OA (12). For advanced OA stages, surgery is the definitive solution (1, 2, 11).
From the multiple factors involved in the pathogenesis of OA, such as biomechanical factors, trauma, and obesity, inflammation is believed to play an important role in knee OA (1, 2, 13). Recently, intra-articular infiltrations are postulated in the management of knee OA based on its anti-inflammatory effect. Infiltrations include corticosteroids and hyaluronic acid (HA) (12), platelet-rich plasma (PRP) (11-13), and even ozone (O2-O3) (14-17). In case of PRP, catabolism and inflammation are reverted and anabolism is stimulated by the release of cytokines and growth factors (12) In case of ozone (O2-O3), years of experience have demonstrated that ozone (O2-O3) is capable of modulating inflammation (1, 4). A very recent study published by the researchers’ study group demonstrated that ozone (O2-O3) decreases inflammation biomarkers (C-reactive protein and erythrocyte sedimentation rate). Moreover, ozone (O2-O3) improves pain, function, and QoL in OA of the knee (17).
As far as the authors are concerned, literature reports only one study, which compares ozone (O2-O3) to PRP for knee OA management (Duymus’ et al. study) (18). On the contrary, there are several studies that compare PRP to corticosteroids, hyaluronic acid (HA), and placebo with superiority of PRP over other treatments. Since a previous study by the current research group recently compared ozone (O2-O3) versus PRP in the management of Chondromalacia, considered as a pre-stage of OA, and the results were very promising, the researchers pursued to compare both treatments on established knee OA (that is mild, moderate and severe grades), because the hypothesis is that ozone (O2-O3) would be as effective as PRP, due to the fact that both treatments may modulate inflammation.
2. Objectives
The objective of the current study was to compare ozone (O2-O3) versus PRP in the management of knee OA in mild, moderate, and severe grades by the evolution of pain, stiffness, function, and QoL in such patients.
3. Methods
3.1. Trial Design
This study was a prospective randomized controlled trial, which compared two treatment protocols (ozone versus PRP) in a parallel design. The study was performed at the Rehabilitation Department of Hospital Universitario Santa Cristina, Madrid, Spain. Outcome measures were evaluated at baseline and at mid-term (two months follow-up period) (Figure 1). The study was in accordance with Helsinki’s Ethical Principles (19).
3.2. Participants
Prior to starting the patient’s enrollment, the Ethical Committee of the Hospital Universitario Santa Cristina approved the study. The study period ran from January 2014 to December 2017. All consecutive patients from the Rehabilitation and Physical Medicine Department were screened for inclusion.
Inclusion criteria:
• Knee OA graded two to four according to Kellgren-Lawrence grading system (20).
• Age older than 18 years.
• No previous intra-articular infiltrations (HA or corticosteroids).
• Patients, who failed at least six months of previous non-surgical treatment (analgesics, NSAIDs, viscosupplementation and/or physical medicine).
• No allergy to ozone (O2-O3).
• No ongoing pregnancy.
• Ability to understand and complete clinical and functional scale.
Exclusion criteria:
• Infection at/or near knee site of infiltration.
• Any severe coagulopathy and/or thrombocytopenia.
• Patients, who failed to compliment clinical/functional scales.
• Patients, who failed to finished proposed treatment protocols.
3.3. Treatment Allocation
Patients were distributed randomly (by using random numbers table) to one of the treatment groups (whether ozone or PRP). In case the patient had both knees affected, the most symptomatic knee was the knee infiltrated. The patient allocation ratio was 1:1.
3.4. Baseline Evaluation
At baseline, significant clinical and demographical data were recorded (age, gender, occupation, and comorbidities). Information of treatment protocols, benefits, and adverse reactions were explained. Informed consent was obtained and signed, clinical, and functional scales were filled prior to treatment. The same scales were evaluated at two-month follow-up after treatment.
3.5. Ozone Treatment
Ozone (O2-O3) protocol consisted of four sessions (at weekly intervals) of an intra-articular infiltration of a medical mixture of oxygen-ozone (95% - 5%), 20 mL at a 20 µg/mL concentration. To obtain such a medical mixture, the medical ozone generator Ozonosan α-plus® was used. To deliver the oxygen-ozone mixture, a 27-G, 4 cm-long Quincke needle was used (14, 15).
3.6. PRP Treatment
The PRP protocol consisted of three sessions (at weekly intervals) of autologous platelet-rich plasma, 3 mL of PRP, infiltrated intra-articularly, after PRP processing. Briefly, at rehabilitation consultation, 27 mL of autologous whole blood was sampled from patient’s arm, and 3 mL of anticoagulant sodium citrate solution was added to complete 30 mL total volume, and transferred to accelerate II platelet concentrating system PRP-S 30 mL® (EXACTECH INC). This kit was gently centrifuged at 2400 rpm for 12 minutes. After that, using the aspirating accessory, plasma was aspirated in order to trap the platelet buffy coat. By doing this, a final 3-mL volume of PRP concentrate was obtained. This technique has been explained earlier by the study group (21, 22).
3.7. Infiltration Technique
For treatment delivery, infiltration of the knee by superolateral approach was the technique performed. After 1% chlorhexidine disinfection, a 27-G needle was used for the ozone (O2-O3) protocol and an 18-G needle was used for the PRP protocol. With the patient lying on the bed, with the knee semi flexed (by the use of a thin towel beneath the knee to increase knee relaxation) and with mild patella subluxation, ozone/PRP was delivered slowly on the lateral and superior edge of the patella. After infiltration, active flexion and extension of the knee were recommended in order to distribute ozone/PRP all over the articulation (Perez-Moro maneuver) (1, 14, 15). The patient remained in supine position for 10 to 15 minutes, if no adverse events were observed; the patient was discharged without further limitations or recommendations. In case of pain, patients were allowed to take analgesics yet not NSAIDs (especially if allocated to PRP protocol).
3.8. Outcome Measures
Symptoms of severity (pain, stiffness, and function) were rated by clinical and functional scales. Visual analogue scale (VAS) is the preferred instrument to evaluate pain in clinical studies because of its sensitivity, reproducibility, and simplicity. This scale is graded from 0 to 10, where 0 means “without pain” and 10 means “unbearable pain” (23).
The Western Ontario and Mac Master index for osteoarthritis (WOMAC) is a scale that evaluates pain, function, and stiffness in knee OA patients. The WOMAC is a scale of the Likert type, ranging from zero (no pain/restriction) to four (severe pain/restriction) on each item: The scale contains 24 items. The maximum score for stiffness, pain, and physical function are 8, 20, and 68, respectively. Lower scores mean fewer symptoms and better function (24).
3.9. Sample Size and Statistical Analysis
The a priori power calculation was inferred from WOMAC physical function subscale, with an expected size effect of 0.4 between both groups at two months follow-up, two time-point measurements (pretest-posttest), a 0.05-level of significance and a 0.8 desired power. A sample of 48 patients were calculated, yet considering a 10% dropout rate at intervention, 54 patients were finally included (27 patients in each group).
The SPSS 20.0® software was used for statistical analysis. In the descriptive analysis at baseline, mean and standard deviation in case of quantitative variables, while frequencies and percentages in case of quantitative variables, were analyzed. Wilcoxon test was performed to assess normality between ozone/PRP groups. Therefore, considering a normal distribution and homogeneity of the variances, for the comparison of the two treatment groups in similar time periods, the Student’ t-test was used. Specifically, for the evaluation of quantitative variables between different treatment protocols, the Student-t test was used, while, for the evaluation of similar treatment protocols, paired t-test was employed. Statistical significance was set at the 0.05 level (P < 0.05).
4. Results
From a total of 66 eligible knee OA patients, a total of 54 patients, 27 allocated randomly to each treatment group, were analyzed in the study. The ratio of allocation was 1:1 (Figure 1).
At baseline, demographic, clinical, and outcome variables were similar between both groups, therefore, the comparison between protocols was suitable (Table 1).
| Demographic | PRP | Ozone |
|---|---|---|
| Age, y | 58.03 ± 10.31 | 65.36 ± 11.02 |
| Gender | ||
| Female | 14 (51.8) | 20 (74) |
| Male | 13 (48.2) | 7 (26) |
| Ratio, female:male | 1:1 | 3:1 |
| Clinical | ||
| OA KL 2º | 4 (14.8) | 3 (11.1) |
| OA KL 3º | 16 (59.2) | 17 (62.9) |
| OA KL 4º | 7 (26) | 7 (26) |
| Outcome variables | ||
| VAS pain | 8.14 ± 1.03 | 8 ± 1.46 |
| WOMAC pain | 14.88 ± 2.65 | 15.59 ± 3.46 |
| WOMAC stiffness | 2.44 ± 1.82 | 4.33 ± 2.41 |
| WOMAC function | 44.48 ± 12.27 | 48.92 ± 16.71 |
Baseline Characteristics of Patients Enrolled in the Study (N = 27)a
In both groups, OA KL 3º was the most frequent radiographic grade, followed by OA KL 4º and OA KL 2º grades (Table 1). Symptoms of severity is dependent on knee OA severity (Table 2).
| OA Grade | VAS | WOMAC Pain | WOMAC Stiffness | WOMAC Function |
|---|---|---|---|---|
| OA KL 2º, n = 8 | 7.75 ± 1.75 | 15 ± 3.33 | 1.87 ± 2.23 | 31.25 ± 16.25 |
| OA KL 3º, n = 32 | 8.09 ± 0.99 | 15.09 ± 2.85 | 4.15 ± 2.14 | 49.18 ± 1.55 |
| OA KL 4º, n = 14 | 8.21 ± 1.62 | 15.71 ± 3.58 | 2.5 ± 2.17 | 49.87 ± 17.32 |
Symptom Severity in Accordance with Different Knee OA Grades, Based on Kellgren-Lawrence Scale, in an Overall Basis (N = 54)a
Before treatment, symptoms severity, such as pain and function, measured by VAS and WOMAC subscales, were similar between both groups. Patients on the ozone (O2-O3) group presented more stiffness than the ones in the PRP group (WOMAC stiffness 4.33 points versus 2.44 points) (Table 1).
If an individualized analysis on each treatment protocol was performed separately, both ozone (O2-O3) and PRP protocols were capable to relief pain and to improve function and QoL, significantly (P < 0.05) (Table 3).
| Variable | PRP Before | PRP After | P Value | O3 Before | O3 After | P Value |
|---|---|---|---|---|---|---|
| PAIN | 8.14 ± 1.09 | 2,96 ± 1.53 | 0.0000 | 8.0 ± 1.46 | 2.14 ± 2.07 | 0.0000 |
| WOMAC pain | 14.88 ± 2.65 | 5.55 ± 2.62 | 0.0000 | 15.59 ± 3.46 | 4.03 ± 3.97 | 0.0000 |
| WOMAC stiffness | 2.44 ± 1.82 | 0.4 ± 0.63 | 0.0000 | 4.33 ± 2.41 | 0.92 ± 0.99 | 0.0000 |
| WOMAC function | 44.48 ± 12.27 | 15.25 ± 12.38 | 0.0000 | 48.92 ± 16.67 | 16.4 ± 12.48 | 0.0000 |
The Effectiveness of PRP and Ozone (O3) on Knee OA (n = 27) in a Before-and-After Individualized Analysis (One-Sample t-Test Analysis)a
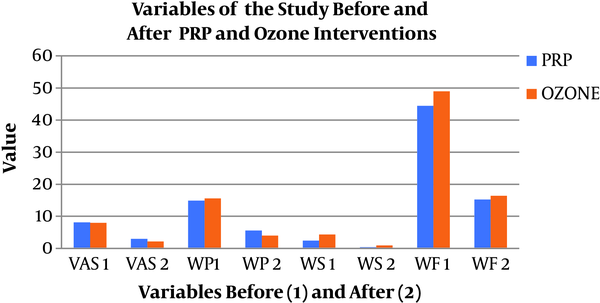
Before treatment, patients in both groups presented similar levels of pain and function, except for stiffness. After treatment, all variables (pain, stiffness, and function) improved in both treatment protocols and without statistically significant difference (P < 0.05) between them (ozone versus PRP) (Table 4 and Figure 2).
| Variable | PRP Before | O3 Before | P Value | PRP After | O3 After | P Value |
|---|---|---|---|---|---|---|
| Pain | 8.14 ± 1.09 | 8.0 ± 1.46 | 0.6765 | 2.96 ± 1.53 | 2.14 ± 2.07 | 0.1066 |
| WOMAC pain | 14.88 ± 2.65 | 15.59 ± 3.46 | 0.4062 | 5.55 ± 2.62 | 4.03 ± 3.97 | 0.1045 |
| WOMAC stiffness | 2.44 ± 1.82 | 4.33 ± 2.41 | 0.0022 | 0.4 ± 0.63 | 0.92 ± 0.99 | 0.0276 |
| WOMAC function | 44.48 ± 12.27 | 48.92 ± 16.67 | 0.2711 | 15.25 ± 12.38 | 16.4 ± 12.48 | 0.7358 |
The Effectiveness of PRP Versus Ozone (O3) by Comparing Both Groups in a Matched Simple Analysis (Paired t-Test Analysis) at the Beginning (Before) and at the End (After) of Intervention (N = 27)a
After ozone and PRP interventions, all of the variables showed a significant improvement (P < 0.01), without differences between groups of treatment. VAS, visual analogical scale; WP, WOMAC pain; WS, WOMAC stiffness; WF, WOMAC function; WOMAC, Western Ontario and Mac Master index for osteoarthritis; PRP, platelet-rich plasma.
The PRP and ozone (O2-O3) treatments are safe and no other adverse effects were reported in the study, except for mild pain after infiltration.
5. Discussion
To the best of author’s knowledge, this is the first randomized controlled trial (RCT), which states that ozone (O2-O3) is as effective as PRP in the management of knee OA, in mild, moderate, and severe grades. In this study, both treatments (PRP and ozone) were capable of decreasing stiffness and pain, and improving function and QoL without a statistical difference between them.
Several RCT have compared intra-articular PRP infiltrations to other modalities, such as hyaluronic acid, corticosteroids, ozone (O2-O3), hypertonic dextrose, and saline placebo. In all of them, as Shen et al.’s meta-analysis states, PRP showed superiority over all the aforementioned modalities (25). However, there is only one study that has compared PRP to ozone (O2-O3) in the management of mild and moderate knee OA; in this study, Duymus et al. showed that PRP was superior to ozone (O2-O3) (18).
Recently, a study compared ozone (O2-O3) to PRP in the management of chondromalacia, considered by many as a pre-stage of knee OA, and the results obtained were very promising (22). For this reason, the researchers hypothesized that ozone (O2-O3) could also be as effective as PRP in the management of established knee OA (from mild to moderate and even severe stages), a fact that has been clearly demonstrated in the present study.
The rationale to postulate PRP and ozone in the management of knee OA is that both modalities are capable of modulating inflammation, a recognized key factor in the pathogenesis of knee OA (1).
In the pathogenesis of knee OA, there is an imbalance between anabolic and catabolic factors (1, 2). Several catabolic cytokines released by chondrocytes are capable of degrading extracellular cartilage matrix, producing cartilage destruction (to date some, IL1, IL6, IL17, TNF-α, and IFN-γ) (4). In case of PRP treatment, PRP delivers growth factors (GFs) and bioactive proteins that inhibit inflammation and catabolic cytokines and stimulate angiogenesis and stem cells, for the healing of the damaged cartilage (26). The PRP inhibits the NF-κβ pathway, acting as an anti-inflammatory agent (27). Moreover, PRP stimulates the proliferation and differentiation of chondrocytes and enhances cartilage healing on in-vivo studies (27, 28). As Lisi et al. stated PRP may also modulate inflammation and analgesia (8).
Fernandez-Cuadros et al. recently reviewed that ozone (O2-O3) could act on key targets involved in the degradation of cartilage and bone (4). They state that ozone (O2-O3) inhibits mineral Metalloproteases (MMP), NO synthesis, PGE2, IL1, IL6, TNF-α, IFN-γ and IFN-β; ozone (O2-O3) stimulates IL4, IL10, IL13, TGF-β, IGF-1, stem cells and chondrocytes (4). Ozone (O2-O3) inhibits inflammatory mediators by down-regulation of TNF-α and TNF-R2 (11). The current study group has also recently published that ozone (O2-O3) is capable of decreasing biomarkers of inflammation in knee OA patients, namely C-reactive protein and erythrocyte sedimentation rate (17). These facts would help understand why PRP and ozone (O2-O3) were effective in the management of knee OA in the present study.
In the current study, PRP and ozone (O2-O3) showed a symptomatic effect on pain, function and QoL in a two-month follow-up period. However, the disease modifying effect is still to be determined. Lisi et al. stated that PRP may decrease articular damage, evaluated by MRI at six months follow-up, and PRP might delay arthroplasty replacement (8). Fernandez-Cuadros et al. showed that ozone increased joint space narrowing in knee OA patients at the two-year follow-up and this treatment also showed a delay in knee arthroplasty replacement (15). Both studies have postulated disease modifying effect of PRP/ozone on knee OA patients (8, 15).
There have been plenty of studies in the last 10 years on the treatment of knee OA by the use of PRP, although the biology is still not fully understood, protocols are controversial, the composition is variable and no consensus on preparation is already stated (29). On the contrary, there are scarce studies on the effectiveness of ozone (O2-O3) on the management of knee OA, and most of them are case reports (1, 2, 14, 15).
As a state of the art in the management of hip and knee OA, some milestones have been observed. In 2008, PRP was injected intra-articularly for the first time. In 2012, the first RCT for the management of knee/hip OA was performed. To the present time, there are 15 RCT that evaluate PRP on knee OA, making comparisons with HA, corticosteroids, saline placebo, and prolotherapy (12, 25). It was not until 2016, that the first RCT between PRP and ozone (O2-O3) was published (18). All previous RCT stated that PRP is superior to different modalities, including ozone (O2-O3).
In case of ozone therapy, Mishra et al. reported that ozone (O2-O3) was more effective than corticosteroids in knee OA management at the six-month follow-up (30). Hashemi et al. described that ozone (O2-O3) was as effective as hypertonic dextrose in the management of knee OA symptoms (31). Momenzadeh et al. reported similar effectiveness of ozone (O2-O3) compared to HA, yet the combination of both was superior at the two-month follow-up (32). Finally, Raeissadat et al. published that ozone is not superior to HA at the six-month follow-up in the treatment of Knee OA (11).
In case of PRP treatment, Chang et al. established that PRP was superior to HA in patients with damaged articular cartilage. In fact, patients with mild Knee OA responded better to PRP than those with severe OA (33). Kim et al. observed that PRP was superior to corticosteroids on knee OA symptoms and had a long-lasting effect (34). Kanchanatawan et al. described better WOMAC scores in patients treated with PRP injections when compared to HA (35). Rahimzadeh et al. published that PRP intra-articular infiltration is more effective than 25% dextrose (prolotherapy) in knee OA management (36). A recent systematic review performed by Laudy concluded that PRP is more effective than HA and placebo in knee OA treatment (37). Jang et al. and Halpern et al. in different studies have reported effectiveness in mild and moderate knee OA in up to one year (38, 39). Patel et al. have stated that PRP is better than saline placebo at the six-month follow-up in knee OA, and one infiltration is as effective as two. On the contrary, Huang et al. stated that three infiltrations are better than one or two at 12 and 24 months follow-up (13). Finally, Raeissadat et al. described that plasma rich in growth factors is as effective as HA in Knee OA patients during the six-month follow-up (40).
The study showed that ozone (O2-O3) is as effective as PRP in knee OA treatment, contrary to the only study that compared both treatments (18), and comes in line with the researchers’ previous study, where PRP was as effective as ozone (O2-O3) in the management of Chondromalacia, a pre-stage of knee OA (22).
5.1. Strengths of the Study
This study highlights the importance of developing a clinical analysis and communication of new bioactive agents, such as PRP and ozone for the treatment of orthopedic conditions as in case of knee OA.
The researchers’ previous study described defined protocols for the preparation and infiltration of PRP and ozone (O2-O3), making them comparable and reproducible.
Treatment protocols were performed on a public institution, where public policies, both PRP and ozone protocols, were afforded by the hospital; there was neither restriction on costs, nor charges were transferred to patients.
5.2. Limitations of the Study
There is a paucity of studies that compare ozone (O2-O3) to PRP in knee OA management. An important limitation of the study was the sample size. Four years were needed to complete such a sample size. Another limitation was the short-term follow-up and the absence of structural evaluation whether by radiography or MRI in a longer follow-up period. Because of a different number of sessions (four sessions of ozone compared to three sessions of PRP) and different volumes infiltrated (20 mL for ozone and 3 mL for PRP) between protocols, there was neither blinding for patients nor for investigators. Despite the small size of the current study, the short-term follow-up and the absence of blinding due to the different protocols, these limitations did not influence the results observed in the current study.
5.3. Conclusions
Ozone (O2-O3) is as effective as PRP in the management of knee OA. Both treatment protocols decreased pain and stiffness and improved function and QoL in mild, moderate, and severe knee OA patients. Both treatment protocols are safe and no side-effects other than pain were observed in the study.