1. Introduction
Crossed aphasia in dextrals (CAD) refers to the aphasia occurring after right hemisphere damage in dextral people. The term “crossed aphasia (CA)” was introduced by Bramwell (1899) to indicate aphasia caused by a cerebral lesion ipsilateral to the dominant hand regardless of handedness. Currently, CA only refers to right-handed individuals and its frequency is rare (1% - 3%) among stroke survivors (1, 2). In most people, the left cerebral hemisphere subserves language processing. However, studies show that the right hemisphere can understand single written and spoken words and that it is prosody and discourse (3). It contributes to many neurocognitive functions that may be fundamental to communication, as well as visuospatial processing, attention, memory, spatial reasoning, problem-solving, and the processing of emotional stimuli and music (4, 5).
In some exceptional right-handers, variably estimated 1% - 3% of the dextral population, the right hemisphere is dominant for language processing. Following neurological damage to the right hemisphere, this group of patients might develop any difficulties in expression and comprehension of spoken and written language. The extra-linguistic deficits that such patients might present with include literal interpretations, difficulty in identifying relevant information, topic maintenance, inability to interpret the whole message of non-literal language (such as metaphoric language, dysprosody, distorted facial expressions and body language, flat affect, problems with conversational rules, impulsivity, and confabulation), deficits in comprehension/expression of prosody, facial expressions, and body language, flat affect, problems with conversational rules, impulsivity, and confabulation (6, 7).
Besides, nonlinguistic deficits after right hemisphere damage might comprise disorientation in time, anosognosia, prosopagnosia, left visuospatial neglect, and other visuospatial deficits (8). Deficits of attention, problem-solving, memory, reasoning, organizing, and awareness of own deficit and planning are examples of cognitive problems due to the right hemisphere damage (3). The current case report used the following criteria to define CAD: (A) the absence of left-handedness or ambidexterity in the individual; (B) clear documentation of the size and location of the lesion in the right hemisphere; (C) the absence of any previous neurological lesions; and (D) sufficiently documented aphasic symptomatology (1). The study reported a case of CAD that presented with aphasia and typical neuropsychological deficits following right hemisphere brain damage. To the best of the authors’ knowledge, it is the first Persian language case of CAD reported internationally.
2. Case Presentation
2.1. Case History
In the previous section, four criteria were mentioned to define CAD. In this part, it is tried to show the patient had all the first three criteria: (1) the absence of left-handedness or ambidexterity in the individual;, (2) clear documentation of the size and location of the lesion in the right hemisphere; and (3) the absence of any previous neurological lesions.
The patient was a 59-year-old right-handed female and her right-handedness was measured by the Edinburgh right-handedness inventory (score +1.0) (9). In her reported history, there was no evidence of left-handedness or ambidexterity in her family (parents and siblings). Speech and language development were reported normal and no developmental disorders were present. No evidence of previous neurological diseases or psychiatric disorders was observed. In March 2014, she experienced ischemic stroke following cardiovascular problems (mitral regurgitation). She was treated with warfarin and aspirin and she was also taking Metoral for her high blood pressure. Magnetic resonance imaging (MRI) of the brain performed two months after the onset of neurological symptoms revealed the presence of signal abnormalities in the right frontotemporal lobe, associated with the effacement of cortical sulci (Figure 1). She did not receive any speech therapy when she was in the hospital but underwent physiotherapy for her left-side hemiparesis.
2.2. Medical History
One-month post-stroke, she was discharged from the hospital and referred to our clinic to start speech and language therapy as a home visit. She had a residual left hemiparesis but could use her right hand for eating and writing. She communicated with others by saying and writing down a few words. Her writing was superior to oral expression and she expressed her needs by writing. She only had correct syntax in sentences consisting of a subject and a verb that was rare in her writing sample. She often produced only one single word, which was her name. When asking her “what did you do today?”, she only answered with the question word “chera?” (“why?”).
Her comprehension seemed to be at a low level. Due to her attention deficits, she did not comprehend completely. According to the relatives, she presented with attention deficits and did not pay attention to their requests (e.g., “mom, look at me”, “mom, give me your hand”). Attention problems interfered with her performance in the task.
2.3. Assessment (Tools and Procedures)
2.3.1. Speech and Language Functions
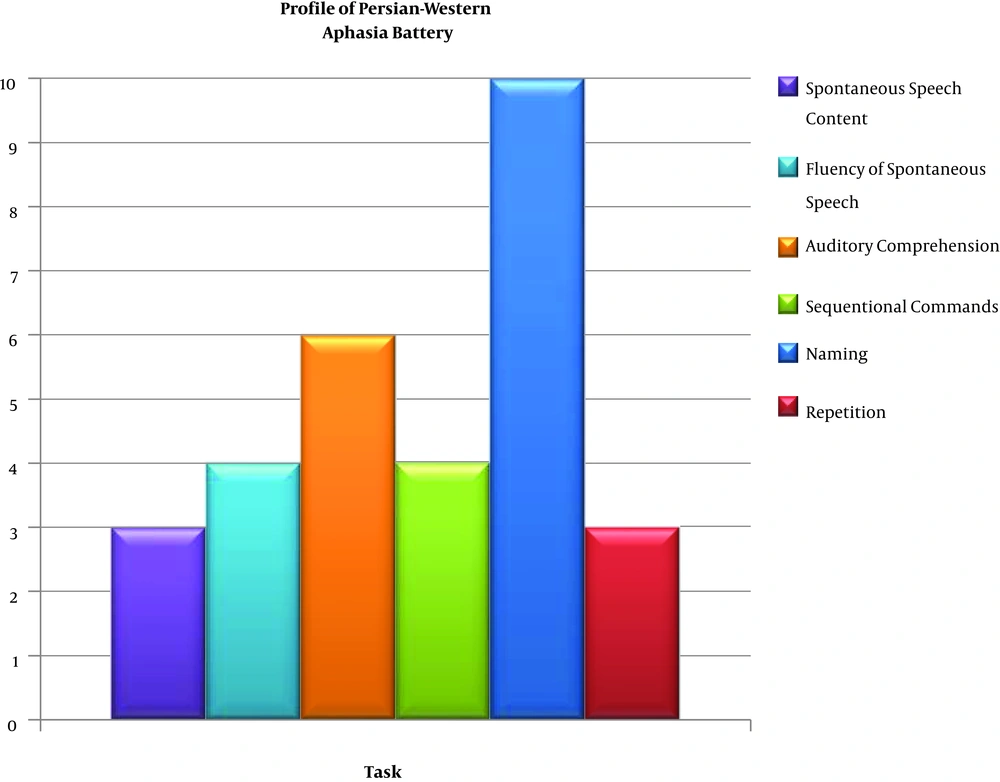
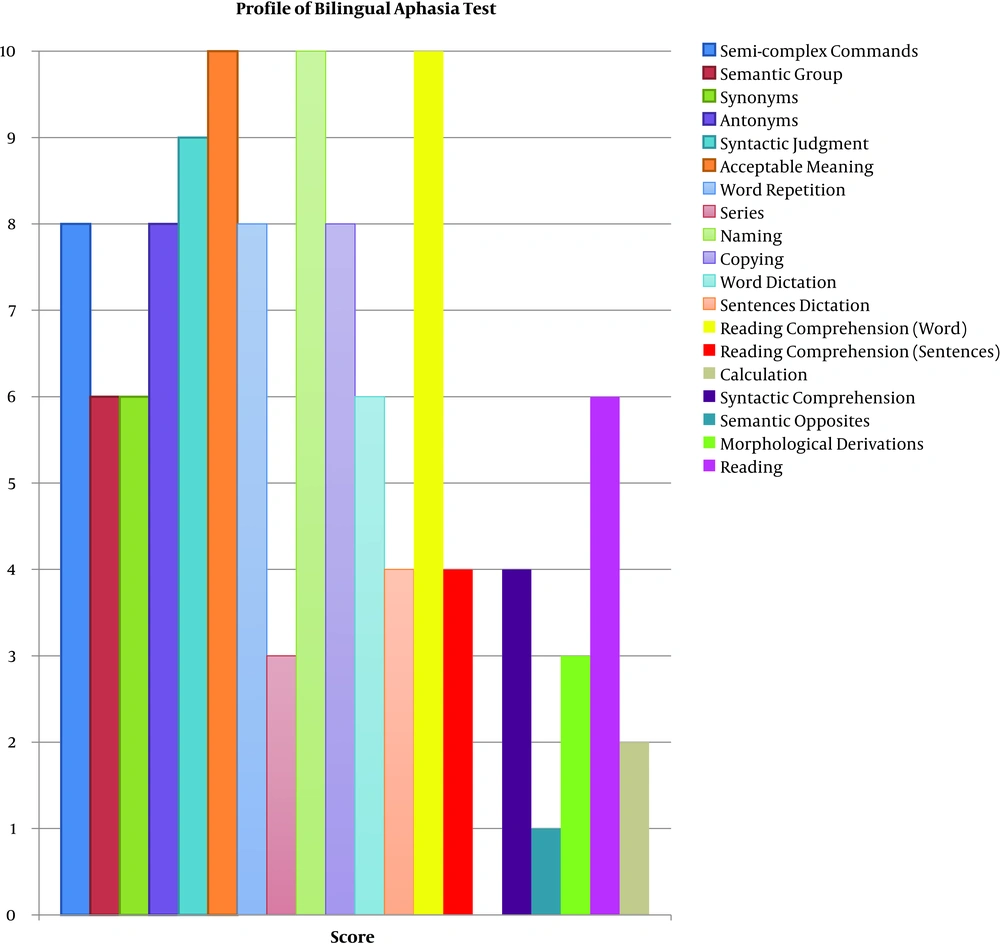
In the following part, we show the evidence of the final criterion of CAD: sufficiently documented aphasic symptomatology. Speech and language functions were measured by the Persian Aphasia Battery (P-WAB) (10) and the Bilingual Aphasia test (BAT) (11). In the current study, the Farsi version of BAT was employed consisting of spontaneous speech, pointing, simple and semi-complex commands, verbal auditory discrimination, syntactic comprehension, synonyms, antonyms, words, and sentence repetition, series, naming, sentence construction, semantic opposites, listening comprehension, and reading tasks. The bedside version of Persian WAB (P-WAB-1) (11) was used, as well. It includes the following sections: content, fluency, auditory comprehension, command comprehension, naming, and repetition. The auditory comprehension task had two levels: semi-complex and complex commands. If the patient did all of them in the correct order, she was scored +; if all the tasks were done but in another order, she scored 3; if only two tasks were done, the score was 2; if only one task was done, the score was 1, and if none of the tasks was done, the score was 0. The results of P-WAB are shown in Figure 2. The cutoff point in this test is 91 and the current study patient scored 55, which was moderate in the severity of aphasia according to P-WAB. She passed only one of the six skills. Based on the BAT, shown in Figure 3, she passed three skills (acceptable meaning, naming, and reading comprehension skills with score 10) and failed one skill (calculation skill, with score 0). Other skills were below normal. She had problems in the morphological derivation. In this task, if she could produce the word or if it was semantically related, she scored +, and if she could not produce the main word, she scored 0; for instance, she was asked to state powerful for power, but she could not. Here are other examples of the task: “young for youth”, “tired for tiredness”, “good for goodness”, and “eatable for eating”.
Semantic Opposite, Syntactic Comprehension Tasks: The syntactic comprehension tasks were characterized by a deficient comprehension of complex syntactic sentences. We read the sentence and she showed us the correct picture indicating the sentence. If she did not answer after five seconds, she scored 0 and if she did, we marked the picture.
Sentence construction, series, reading comprehension of sentences, and dictation of sentence tasks: If she wrote correctly, she scored + and if she did not, she scored 0. Finally, the total score was calculated.
2.3.2. Visuoperceptual Skills
Visuospatial functions were investigated by line bisection, painting, and cancellation tasks (12). In the painting task, she was asked to draw a person and a flower. In the cancellation task, she had to mark the stars, which were distributed in a box.
2.3.3. Language
Performances on the P-WAB and BAT confirmed the presence of language disorder, typologically consistent with Broca’s aphasia.
2.4. Analysis of Utterances
She showed no syntactic complexity and little variation in her elicited output, which consisted of 41 nouns and only four verbs. The utterances varied from two to four words long without any phonological and semantic paraphasia. She frequently used a limited range of single content words (e.g., names of her family members). She only sporadically used verbs and function words (conjunctions, adverbs, etc.). A spontaneous three-minute speech sample, in which the patient talked about her family, contained 54 words of which 47 were content words (87%) (Appendixes A and B in Supplementary File). According to the analysis, the mean length of utterances (MLU) of the case was 2.90. She also had a sample of storytelling based on the bird’s nest storytelling task (Appendixes A and B in Supplementary File).
In the task of series counting from 1 to 10 and telling the names of seasons, the patient could not say them in the correct order (e.g., “1, 2, 4, 5, 5, and 7” and “summer, spring, fall, winter”). She also had problems with a sentence construction task. She also had problems in the section of fluency of spontaneous speech of BAT; her score in sentence construction was 2, which was moderate (Box 1).
| Sentence Construction Tasks |
|---|
| 1. Task: “sandali, doktor, visit” (chair, Dr., visit); answer: “sandali[N]visit[N]” (chair visit). |
| 2. Task: “xodkar, nevestan, abi, kaqaz” (pencil, write, blue, paper); answer: “man [PREP]xodkar[N]naqashi[V]” (I pencil painted). |
| 3. Task: “miz, bazkardan, komod” (table, opening, drawer); answer: “miz[N]miz[N]” (table table). |
In the morphological derivation task, she could not produce any correct responses (BAT score 0). In this task, she repeated the stimulus or stated: “I don’t know” (Box 2).
| Morphological Derivation Tasks |
|---|
| 1. Task: “xubi” (goodness); answer: “nemidunam[V]” (I don’t know) |
| 2. Task: “javani” (youth); answer: “javani[N]” (youth) |
Copying numbers and single letters: The BAT score was 6; it was superior to the copying of sentences. In a word dictation task, her BAT score was 6 and the sentence dictation score was 4. She deleted parts of the sentence and often substituted the verb or subject by words of the previous task sentence in the current task sentence. Therefore, there was a strong tendency toward perseverate and the patient also showed agrammatism in spelling (Box 3).
| Copying Numbers and Single Letters Tasks |
|---|
| 1. Task: “doxtarpesarrabusid” (the girl kissed the boy); answer: “doxtar[N]bus[N]” (the girl kiss). |
| 2. Task: “kamiyonmashinramikeshad” (truck is pulling the car); answer: “kamiyun[N]mashin[N]-o[POSP]zad[V]” (truck hit the car). |
| 3. Task: “ZanMardraholmidahad” (woman was pulling man); answer: “kamiyon[N]mard[N]-aro[POSP]hol[ADJ]dad[V]” (truck pulled that man). |
The syntactic structures of utterances were very simple. No compound or complex sentence was observed. The noun phrase structure was simple at the syntactic level.
What she wrote spontaneously was semantically unintelligible. Another characteristic of the case’s handwriting was that she did not write on the writing line and had the inclination to downward.
2.5. Comprehension
2.5.1. Auditory Comprehension
Her auditory comprehension was impaired at the level of semi-complex and complex commands (BAT score 4); for example, she could not follow two-step commands. When asked to “close your eyes and then show me your hand”, she only performed the last part of the task. However, the ability to point to one-step commands was intact and she pointed correctly to what we asked (e.g., show me the glass). In the syntactic comprehension tasks, she could not discriminate syntactic differences between active and passive sentences “the dog bites the cat” and “the cat was bitten by the dog”. Her repetition ability was intact at the level of word (16 correct words out of 20 words) and nonword (four correct nonwords out of 10 nonwords; e.g., she correctly repeated “yal”, “par”, “qaz”, “fag”, “gak”, and “zar” after the examiner, etc., but she had problems with the repetition of sentences (one correct sentence out of seven sentences) (Box 4).
| Auditory Comprehension Tasks |
|---|
| 1. Task: “madarbace-as rabusid” (the mother kissed her baby); answer: “madar[N]bace[N] rabusid [V]” (mother kissed baby). |
| 2. Task: “barg-ha-ye deraxtrixt” (leaf of plane trees fell); answer: “barg[N]-ha[PL]-ye[LINK]deraxt[N]rixt[N]”(leaf of plane fell). |
| 3. Task: “pesarharruz be madresemiravad” (boy goes to school every morning); answer: “harruz[N] sob[N]pesar[N]miravad[N]” (every morning the boy goes). |
2.5.2. Written Comprehension
She displayed left neglect dyslexia. For example, she only read the words of sentences positioned at the right side of the page; however, sometimes she read the whole sentence, but changed the verb tense; in this section, she should read the words or sentences voiceless and then point to the picture (score 2 out of 10 tasks) (Box 5).
| Written Comprehension Tasks |
|---|
| Task: “doxtarpesarraholmidahad” (the girl is pushing the boy); answer: “doxtar[N]pesar[N]rahol dad[V]” (Girl pushed boy). |
| Task: “kamiyonmasinranemikesad” (the truck does not pull car); answer: “kamiyonmasinrakesid” (the truck pulled car). |
| Task: “kamiyonmasinramikesad” (the truck is the pulling car); answer: “kamiyon[N]masin[N]rakesid[V]” (the truck pulled car). |
Her reading comprehension was intact at the word level but impaired at the sentence level.
2.5.3. Pragmatics
The patient displayed some linguistic pragmatic impairment. She had difficulty in topic maintenance; for example, she described her activity during the last day: “sob bidar (awake morning); sobhane (breakfast); faqat-hamin (just that); man zang zadam (I called); un-ha qors-an (They are tabs); ziyad (lots of); xabdidam (I dreamed); mord-e (Is dead); man mord-am (I died); tarsidam (I afraid)”.
The sample of discourse showed that she was unable to adapt to the listener (e.g., changing the content or topic of a message depending on the listener, because when it was tried to give her some cue to explain about her dinner and other activities and tell the name of the movie that she watched last night, she continued telling about her dream. When she was listening to the speaker, she could not distinguish and interpret the jokes in discourse.
In the storytelling, the patient could not find the important elements of each picture (score four out of 10). For example, in the picture in which “the boy fell when the tree branch broke”, she did not pay attention to the branch and only stated: “the boy fell”.
2.5.4. Visuospatial
Visuospatial neglect is a common consequence of unilateral brain injury. It is most often associated with stroke and is more severe and persistent following right hemisphere damage, with reported frequencies in the acute stage of up to 80%. Neglect is primarily a disorder of attention whereby patients characteristically fail to orientate, report, or respond to stimuli located on the contralesional side (13). The case’s left visuospatial neglect was confirmed by cancellation, drawing, and line bisection tasks. While she was drawing a flower, she neglected the left side and while she was drawing a person, the drawing only included the right side of the body. In cancellation tasks, she only marked the items, which were on the right side of the screen. She showed visual neglect in the reading tasks, especially in the sentence reading tasks (e.g., she read “he saw himself” for “he saw himself in the mirror”).
3. Discussion
The present study revealed that the patient had crossed Broca’s aphasia according to the four previously mentioned criteria: (A) she was right-handed and also had no left-handed family members or relatives or with ambidexterity; (B) her MRI indicated damage to right frontotemporal and parasagittal frontal lobe; (C) she had no history of previous brain damage; and (D) the case showed symptoms of Broca’s aphasia such as telegraphic speech deficits in sentence construction and morphological comprehension. Consequently, the patient was diagnosed with crossed Broca’s aphasia. In the BAT profile, she showed deficits in the following tasks: sentence construction morphological derivations, semantic opposites, syntactic comprehension, series, synonyms, and comprehension of semi-complex commands. Naming, judgment about acceptable meaning, and word reading comprehension were normal. Besides, she presented some deficits consistent with non-dominant right hemisphere damage (impaired discourse, low level of attention, and left visuospatial neglect), which was the distinctive feature of this patient with CAD in the Farsi language (14).
To communicate, it was observed that the case relied on nouns and simplification of language output, as demonstrated in the speech sample. There was little variation in syntax and morphology in written and spoken language. She did not use any function words in speech, which resulted in a telegraphic style. She also used a simple grammatical sentence structure due to low access to morphosyntactic resources and poor lexical access (15). In the studies of conversational behavior, adults with right hemisphere damage talk more about themselves in their conversations; the current study patient also represented this feature. The present study results were in agreement with those of Coppens et al. (16).
She represented typical symptoms of language dominant left hemisphere damage (e.g., telegraphic speech, limited variety of syntax, morphology in both written and spoken languages, determiners, and adjectives that were very rare in the elicited data of the patient) and also a range of deficits indicating the right hemisphere pathology (16). One of the most commonly described right hemisphere damage deficits is in figurative/nonliteral language impairment (16, 17). The current study patient showed pragmatics (such as turn-taking problem, taking fewer turns, talking more about herself) and discourse problems (such as deficits in the ability to identify main ideas or themes and reduced cohesion of discourse production, not organized, disjointed discourse) (18). In her conversations about a specific topic, she produced some unnecessary and redundant details. This problem can be related to the inability to discriminate essential points to build-up discourse (19). Besides, she had significant left-sided visuospatial neglect as expected in the right hemisphere lesions.
In summary, the analysis of symptoms in the current study patient confirmed the right hemisphere dominance for language.
3.1. Conclusions
One of the interesting points found in the current study patient was a sign of right hemisphere damage, while linguistic processing was done in the left hemisphere. These symptoms consisted of mentioning unnecessary points and unimportant details. In other words, it can be interpreted that the right hemisphere of this patient also had some left hemisphere processing including the use of grammar rules and some right hemisphere processing such as preserving the subject and removing unnecessary details; therefore, the patient’s manifestations were a combination of both symptoms.