1. Background
Different studies show that left hemisphere brain damage often leads to aphasia associated with phonological, syntactic, and semantic defects (1). Soltani et al. (2), demonstrated that the prevalence of post-stroke aphasia among Iranian patients in Tehran was 22.7%. In a dual classification system and based on the spontaneous speech features, aphasia is divided into fluent and non-fluent types (1). One of the symptoms relatively common in non-fluent aphasia is agrammatism with an ungrammatical and telegraphic speech and elimination of function words. Individuals with agrammatism show more difficulty in producing verbs than nouns, especially in verb morphemes (1). A number of studies showed that the tense marker is damaged more than other inflectional morphemes and the application of past-tense marker is significantly impaired more than the other verb-tense markers (3, 4).
Persian verbs have two main structures including a root and inflectional morphemes (5). There are two kinds of the past and the present roots (6). The inflectional structure of verbs in Persian is comprised of several patterns namely those of participle (one term), voice (two terms), infinitive (one term), tense (three terms: past, present, and future), mood (three terms: indicative, subjunctive, and imperative), aspect (four terms: simple/continuous, perfective/imperfective), and person plus number (six terms: three persons each singular or plural) (7). Some of these patterns function together such as tense, mood and aspect, then there are nine grammatical tenses in Persian including five in the past (simple past, past continuous, past perfect, present perfect, and past subjunctive), three in the present (present indicative, present subjunctive, and present continuous) and one in the future (6).
Verbs play the main role in the sentence production and comprehension; therefore, any deficit in the verb processing can have serious impacts on the patients' language content (8). Any therapeutic approaches related to the verb inflection in Persian patients with agrammatism could have positive effects on the process of message delivery.
In line with the purpose of the current study, several studies with different therapeutic approaches are conducted in the field of verb inflection deficits in patients with aphasia and agrammatism, which show improvement in the inflection of regular and irregular verbs in three tenses (9-12). For example, Mitchum demonstrated improvement in the inflection of regular and irregular verbs in three tenses in sentence structure and narrative speech levels following a treatment based on the Garrete model (9).
Faroqi-Shah compared two morphophonological and morphosemantic methods to treat patients' deficits with English tense markers of regular and irregular verbs in past, present, and future tenses. The results indicated improvement in the severity of aphasia and training and untraining verb inflection, with a little generalization to the past tense of the irregular verbs in patients with aphasia receiving morphosemantic treatment (13, 14).
Few studies are conducted in the field of verb inflection treatment in English (9-11, 13-15), and in Persian no study was found in this field. The current study aimed at investigating the effect of morphosemantic treatment on the expression of the tense markers in Persian-speaking patients with aphasia and agrammatism, evaluating the generalization to the expansion verbs, and probing maintenance of the effects.
2. Methods
2.1. Participants
The current case report was conducted on two monolingual Persian-speaking males with moderate chronic non-fluent aphasia and agrammatism due to left hemisphere ischemia. Both participants could read and write and their mean length of utterances (MLU) were three morphemes/utterance. The participants had only one stroke, without any history of severe apraxia, dysarthria, psychiatric or neurodegenerative disorders, hearing or visual impairments, right hemisphere damage, severe reading problems, comprehension disorder, and naming disorder (Table 1). Written informed consent form was signed by the subjects or their families.
| Characteristic | PM | MM |
|---|---|---|
| Age (y) | 37 | 49 |
| Marital status | Single | Married |
| Education (y) | 16 | 12 |
| Handedness | Right | Right |
| CVAa passed time (y) | 4 | 1 |
| Damaged area | Left parietal lobe | Left frontoparietal and parietal lobe |
| Medical history | - | Left lower limb amputation (below the knee) and kidney transplant due to chronic diabetes |
| Rehabilitation history | 4 years of speech therapy | - |
| Memory digit span | 4 | 4 |
| Mini-cog test | Nearly normal | Nearly normal |
| Right hemiplegia | Mild | Not seen |
| Dysarthria | Mild | Not seen |
| Verbal apraxiab | Not seen, 22 | Not seen, 19 |
| BDAEb,c | ||
| Comprehension | 88 | 94 |
| Oral expression | 71 | 78 |
| Repetition | 60 | 80 |
| Vocabulary amount | 86 | 89 |
| Writing | 77 | 58 |
| Reading | 33 | 61 |
| P-WAB-1 (AQ)b,d | 70 | 80 |
| Speech content | 90 | 60 |
| Verbal fluency | 30 | 40 |
| Auditory comprehension | 70 | 100 |
| Comprehension of continuous orders | 100 | 80 |
| Repetition | 30 | 100 |
| Naming | 100 | 100 |
| Persian naming aphasia testsb | ||
| Nouns | 98 | 72 |
| Verbs | 88 | 56 |
| Verb inflection testb | 20, 95 | 30, 100 |
a Cerebrovascular attack.
b Data are expressed as No. (%).
c Persian version of Boston diagnostic aphasia examination.
d Bedside version of Persian Western aphasia battery (aphasia quotient).
2.2. Experimental Stimuli and Material
In the current study, a comprehensive set of tools was used to evaluate different aspects of the patients' problems. A researcher-made demographic questionnaire, the Persian version of the Western aphasia battery (internal consistency (IC) = 0.71, test-retest reliability = 0.65, content validity ratio (CVR) = 0.78, and significant differential validity (P < 0.001) (16), Persian aphasia battery test (IC = 0.93 and significant differential validity (P < 0.001) (17, 18), Persian aphasia naming test (IC = 0.96, test-retest reliability = 0.87, and convergent validity = 0.58) (19, 20), picture verb naming test for patients with aphasia (a common-clinical tool) (21), verbal apraxia test (IC = 0.96, split-half reliability = 0.94, inter-rater reliability = 0.83, high CVR, and significant criterion validity = 0.90 (P < 0.001) (22, 23), the oro-motor control assessment form (a common-clinical tool), the Edinburgh handedness scale (IC = 0.97, split-half reliability = 0.92, and convergent validity = 0.75) (24), a researcher-made verb inflection test and elder mini-cog cognitive screening test (IC = 0.83, inter-rater reliability = 0.76, test-retest reliability = 0.86, convergent validity = 0.39), and significant differential validity (25).
The verb-tense marker test, similar to that of Faroqi-Shah (13) included 10 correct sentences. For example: “pesare Ɂalân (/Ɂ/ representing a glottal stopin IPA, /â/ is equivalent to/a:/ in IPA, /š/ is equivalent to /ʃ/ in IPA, /a/ is equivalent to /æ/ in IPA, /e/ is equivalent to /e/ in IPA and /i/ is equivalent to/I/) dâre tuppo šut mizane.”; pesar (subject), -e (Ezafe marker) (26), Ɂalân (present time adverb), dâre (present continuous auxiliary verb), tupp (object), -o (objective marker), šut mizane (compound verb, /mi/ as the marker of the present continuous tense + present root of /zan/ + /e/ as the marker of singular third person): “the boy is shooting the ball, now.” The verb-tense marker test included 10 incorrect sentences too. For example, a sentence like “pesare diruz dâre tuppo šut mizane.” has a wrong time adverb "diruz (yesterday)" and there is disagreement between verb-tense and temporal adverb. The researcher used tense markers of simple past and present continuous verbs with temporal adverbs of diruz (past tense adverb: yesterday) and Ɂalân (present tense adverb: now). The participants answered less than 30% of the items correctly, which meant their functions were below average and could be interpreted as verb inflection deficit.
In order to provide treatment material, first, 60 black and white line-drawing pictures related to 30 verbs from Persian verbs naming test (21) were drawn in 30 separate pages by a graphic designer. Each page contained two pictures related to the past and present tenses of a single verb (Figure 1). Then, 46 pictures (23 verbs) with a name agreement of 100% (investigated on 20 males and females) were selected. All pictures were depicted in third-person singular. These 23 verbs included three examples, 10 training, and 10 expansion verbs matched together in terms of frequency (27), verb structure, regularity and argument structure (5, 28).
2.3. Overall Design
The current case report investigated the effectiveness, generalization, and maintenance of morphosemantic treatment on the training and expansion verb inflections in three baseline (A1), treatment (B), and withdrawal (A2) phases (29). The participants were assessed over three sessions in order to define each aspect of their problems. Based on the study by Faroqi-Shah and considering the Persian language characteristics, in the baseline phase (A1), the inflection of 10 training and 10 expansion verbs was assessed in two tenses using 40 researcher-made pictures in a confrontation naming task during three consecutive days in a week. In the treatment phase (B), 15 treatment sessions (nearly 30 to 45 minutes each) were held in the participants' house within a month. Each session was started with the evaluation of the patients' functions in the tense inflection of 10 training verbs. In the 5th, 10th, and 15th sessions, the therapist evaluated the patients' functions in the tense inflection of 10 expansion verbs, too. In the withdrawal phase (A2), tense inflection was evaluated in all training and expansion verbs three times in three consecutive weeks. In the final examination phase (E), verb inflection test was administered again.
2.4. Intervention Method
First, the subjects were familiarized with treatment method using three exemplar verbs via naming (for example: šut zadan (infinitive verb): to shoot) and inflection of them in the two tenses (for example: “pesare dâre tuppo šut mizane. pesare tuppo šut zad.”; (compound verb, past root of /zad/ for the inflection of the simple past tense + /ϕ/ as the marker of singular third person): “The boy is shooting the ball. The boy shot the ball.”). The morphosemantic treatment according to Faroqi-Shah includes five stages as follows (14): 1. Confrontation naming: The participant should name the action related to 10 training verbs; 2. Anomaly judgment: Using 10 training verbs, 10 correct or incorrect sentences in terms of agreement between temporal adverb and verb-tense are auditorily presented to the participant and they should diagnose them; 3. Auditory comprehension: 10 sentences containing training verbs were expressed and the participant should point to the temporally consistent picture from two pictures; 4. Sentence completion: The participant should complete (write or express) 10 verb-free sentences related to 10 training verbs by the correct form of the relevant verbs regarding the adverb of time (for example: pesare diruz tuppo …. [šut zadan]: the boy … the ball yesterday [shoot]); 5. Sentence construction: The participants should select cards and arrange them to form a sentence that corresponds to a given picture in one of the two tenses (for example: “dâre-pesare-šut zad-šut mizane-tuppo”: “Is-the boy-shot-shooting-the ball” for the picture of present tense). In all treatment stages, the therapist gave patients proper verbal feedback about the accuracy of the verb tense markers.
2.5. Scoring
The correct answer was given 1 score and the incorrect one was given 0, based on the accuracy of the verb-tense, not the verb aspect and mood.
2.6. Reliability
Inter-rater reliability was obtained for 20% of randomly selected data from two dependent measures of training and expansion verbs by two experienced speech and language pathologists blinded to the study. The calculated reliability via Spearman correlation coefficient was 0.95.
2.7. Data Analysis
Data were analyzed with SPSS version 21 and Microsoft Office Excel version 2010 software. Changes from baseline to treatment phase were statistically analyzed via level, trend, and slope analysis (30), Two-standard-deviation band (2-SD Band) (30), C statistics (30, 31) and effect size analysis by percent of non-overlapping data (PND) (31, 32). To examine the lasting of the treatment effects, and generalization to the expansion verbs, the percentage of the correctly named items, and the effect sizes via d1 and d2 statistics (33) were calculated. The criteria to interpret the effect sizes was the following benchmarks: 4.0, 7.0, and 10.1 for small, medium, and large, respectively (34).
3. Results
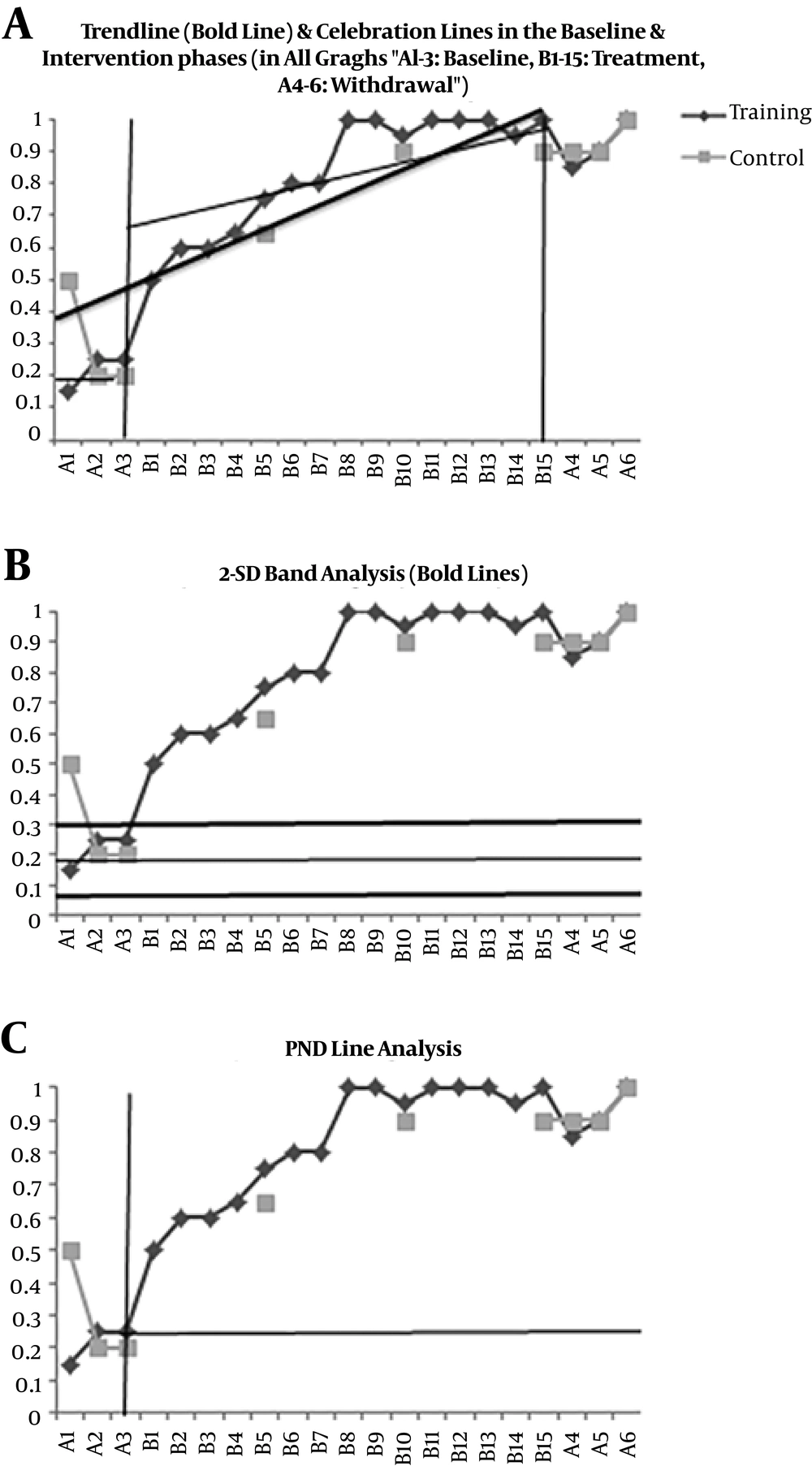
Participant 1 (PM) showed a significant increase in the use of the inflection for the training verbs during treatment phase from 50% to 100% accuracy (C = 0.93, Z = 3.44). According to Figure 2A, PM showed an upward trend with the slope of 0.03 over the course of treatment for training verbs and an increase from baseline level (19%) to the treatment level (68%). In addition, Figure 2B shows that more than 2 successive intervention points (15 points) were located out of +2-SD band, indicating a significant increase from the baseline to treatment phase (30). In Figure 2C, the treatment was completely effective in verb-tense inflection (100%) and all treatment points were above the PND line. PM could generalize the tense markers to the expansion verbs from 20% to 100% (Figure 2A). The effect size of the generalization was small (d1 = 3.74) (34). During the withdrawal phase, the PM showed 15% decrease in the accuracy of the use of the tense markers in the training verbs (Figure 2A). The maintenance effect yielded large effect size (d2 = 36).
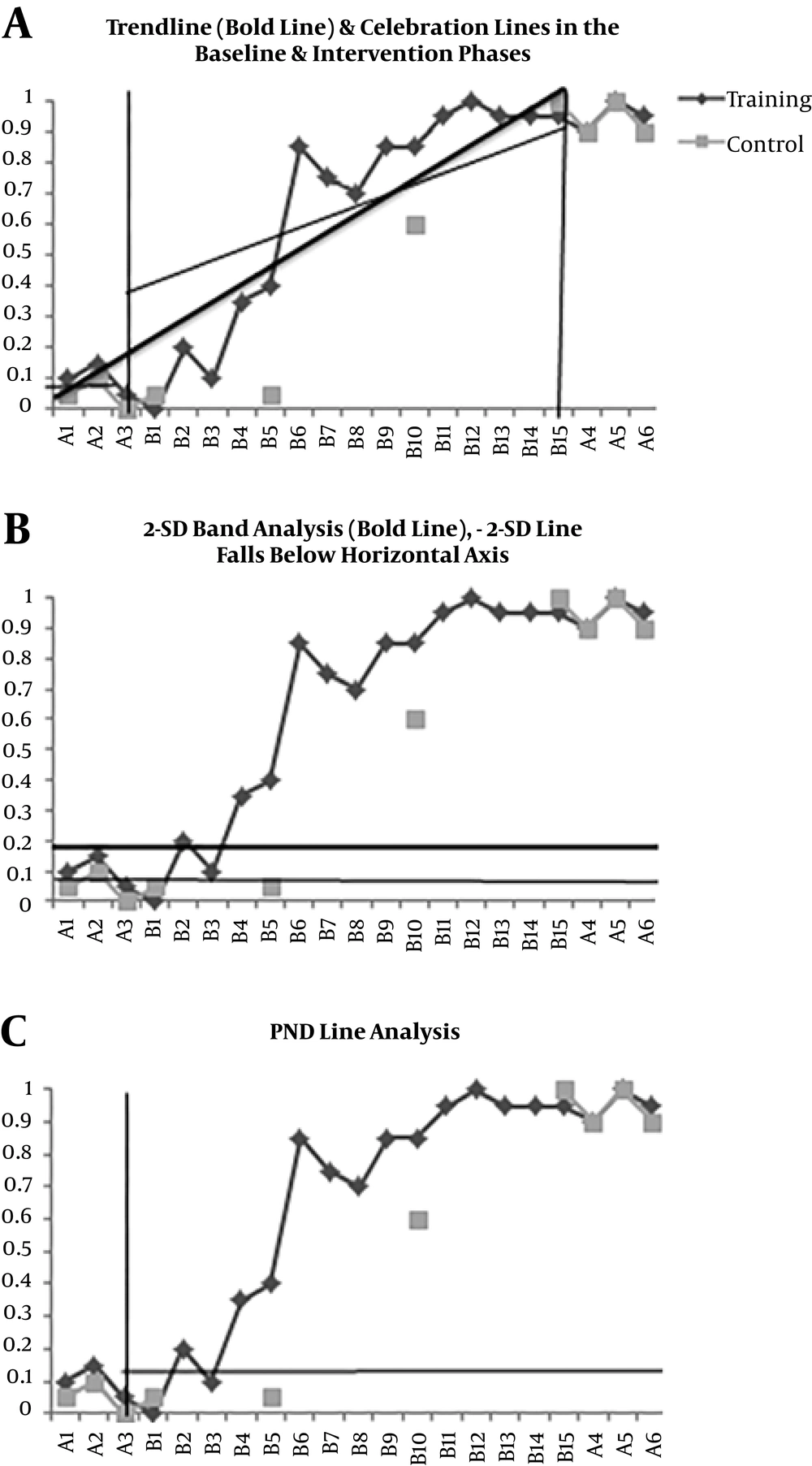
Participant 2 (MM) showed a significant increase in the use of the inflection for the training verbs during treatment phase from 0.00% to 95% accuracy (C = 0.99, Z = 3.66). According to Figure 3A, MM showed an upward trend with the slope of 0.05 over the course of treatment for training verbs and an increase from baseline level (7%) to the treatment level (38%). In addition, Figure 3B shows that more than two successive intervention points (12 points) were located out of +2-SD band, indicating a significant increase from the baseline to treatment phase. In Figure 3C, the treatment was completely effective in verb-tense inflection (80%) and 14 treatment points were above the PND line. MM was able to generalize the tense markers to the expansion verbs from 0.00% to 90.00% (Figure 3A). The effect size of the generalization was large (d2 = 44) (34). In the withdrawal phase, the MM showed no decrease in the accuracy of the use of the tense markers in the training verbs (Figure 3A). The maintenance effect yielded large effect size (d2 = 44).
4. Discussion
The current study results showed that the morphosemantic treatment was an effective therapeutic approach to help patients with aphasia to produce the Persian tense markers correctly. The participants showed a significant increase in the use of the tense makers in the intervention phase. The current study findings were consistent with those of the Faroqi-Shah. Faroqi-Shah found that individuals with aphasia receiving morphosemantic treatment showed significant improvement in the accurate production of trained and untrained verb-tense inflections in sentence contexts (13-15). The small changes in patients' functions in the baseline, dramatic changes in the therapeutic phase, and a decrease in withdrawal phase, all were signs of the positive effect of the morphosemantic approach. This is again another evidence to claim that Faroqi-Shahs' findings can be generalized to the Persian-speaking patients.
The current study showed that the morphosemantic approach had further generalization to the untrained regular and irregular Persian verbs in the present and past tenses compared with those of the other languages. In fact, this finding was the only difference between the current study and other studies (e g, Faroghi-Shah). The participants in the study by Faroghi-Shah had a relatively small generalization to the irregular past tense (9-11, 13-15), but participants of the current study had almost perfect generalization to the regular and irregular past tense. This difference may be a result of the language differences. Irregular verbs in the English language change completely in the past (its root and its inflection), while in Persian the verb root is almost similar for different tense concepts only inflections can change. Both participants maintained their performance above the baseline in the withdrawal phase, which was consistent with the results of Faroqi-Shah (13, 14).
Further studies could be administered with larger sample sizes, less inclusion criteria, and multi-handicapped Persian-speaking patients with aphasia. Some patients do not have literacy skills or completely lose their ability to read and write due to language impairment or severe right hemiplegia (not able to write with their left), then they may be deprived from treatment; therefore, in the future studies, the literacy criterion can be ignored, and gestures or other kinds of communication could be replaced for the writing parts. It can be an ideal plan for the future studies to include this therapeutic approach with other approaches and compare the results. In addition, the morphosemantic treatment can be taught to the patients, while regarding the variables of connected speech, its effects can be observed in the spontaneous speech.
4.1. Conclusion
The morphosemantic approach can be considered as an effective intervention for the Persian-speaking patients with agrammatism. This therapeutic approach has high potential to generalize the improvement to the non-therapeutic targets in Persian patients due to the unique features of the Persian language.