1. Context
The use of ultrasound (US) as an imaging modality for the evaluation of the musculoskeletal system in the rehabilitation settings has expanded dramatically in the last decade (1). The resolution of US has improved thanks to the technological advancements, and access is easier due to the lower cost of equipment (2). US in the rehabilitation setting adds accuracy on diagnosis and security in dynamic guidance for interventional procedures (2). These benefits have increased the US use in musculoskeletal clinics and rehabilitation settings, providing clinical, anatomical, and technical integration all in a one-day-evaluation (2).
Despite its obvious benefits, US is an operator-dependent technique that requires a long-term training course to develop accuracy on musculoskeletal diagnosis (3, 4).
The aim of this review is to instruct beginners in the recognition of different musculoskeletal tissues, commonly seen artifacts, and understanding the basics of musculoskeletal ultrasound.
2. Review of the Literature
2.1. Physical Properties of Ultrasound
US images are created by reflected waves that return to the transducer. The nature of the image is based on the properties of different tissues in the body, namely bones, muscles, tendons, or ligaments. A number of factors influence this process such as reflection, refraction, absorption, and attenuation (1).
Acoustic impedance: US is propagated on several tissues as pressure waves. The resistance offered by tissues to propagate sound waves is called acoustic impedance (4).
Attenuation: Attenuation is the progressive reduction in the intensity of the wave as the sound waves travel through the tissue (1).
Reflection: Reflection in US refers to the return of the sound wave energy back to the transducer. This principle will allow the image to be generated by the US machine. Generally, more reflection results in a more hyperechoic (brighter) image. Tissues with greater impedance (resistance) like bones will produce more reflection (1, 4).
Angle of incidence: Angle of incidence is critical to the amount of reflection back to the transducer. The ideal angle of sound waves should be perpendicular to the probe. If the angle is not vertical, fewer sound waves are reflected back to the transducer, resulting in a more hypoechoic (darker) image with less clarity. This phenomenon is known as anisotropy (Figure 1) (1, 4).
Refraction: Refraction occurs when the incident sound waves contact the boundary of tissues at an oblique angle. This causes the reflected sound beam to travel in a direction away from the transducer. Then, refraction results in a loss of propagated signal (1, 4).
Absorption: Absorption is the propagation of the sound beam in the form of heat. As a result of absorption, none of this energy returns to the transducer to contribute to the creation of image (1, 4).
Scatter: Scatter refers to the propagation of incident sound waves in an oblique direction. This phenomenon occurs when the tissue analyzed is not completely homogeneous or has rough edges. As a result, sound beam changes on different directions (1, 4).
2.2. Artifacts in Ultrasound
Artifacts in US imaging are defined as any variation not generated by tissue under evaluation. An artifact is an image not related to real anatomical structures (5). Artifacts can provide clinical clues for underlying pathology (1).
Anisotropy: Anisotropy is the artifact that results from the angle of incidence, making structures look as hyperechoic or hypoechoic (Figure 1). This is very common in well-structured tissues such as tendons, nerves, and muscles (5).
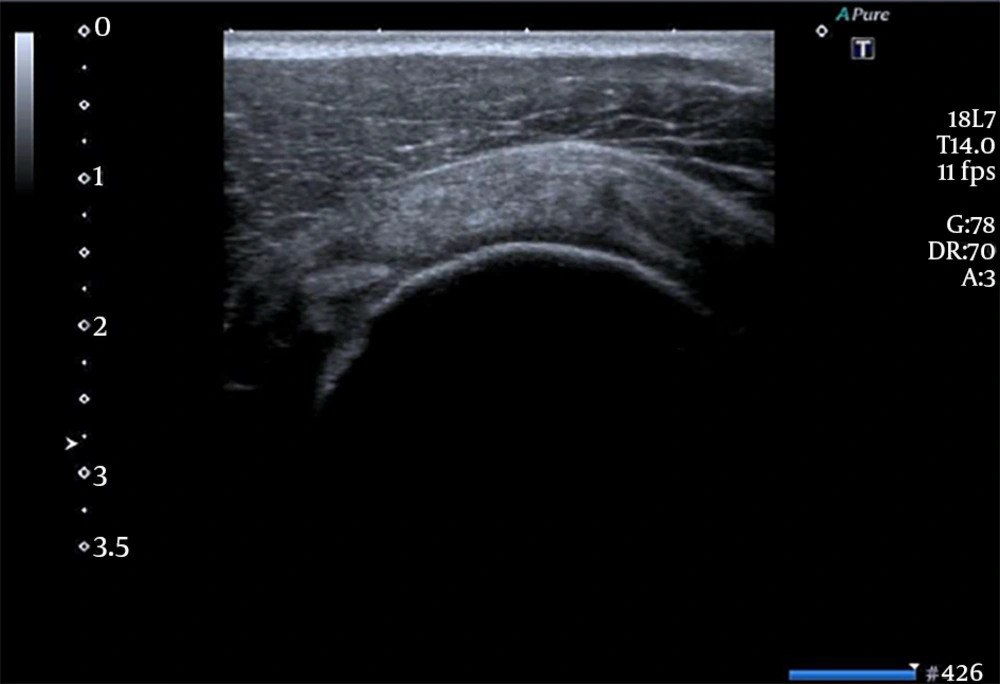
Acoustic shadow or bone shadow: US does not penetrate bone because of the densely calcified cortex, and virtually all of the sound reflects back to the transducer. This is very common in tissues with bone, calcium, metallic implants, or air within the tissues. The appearance of the image beneath the cortex is often referred to as a bone shadow. This term is used for the acoustic artifact deep in the hyperechoic bone outline that is the result of the sound wave attenuation (Figure 2) (1, 5).
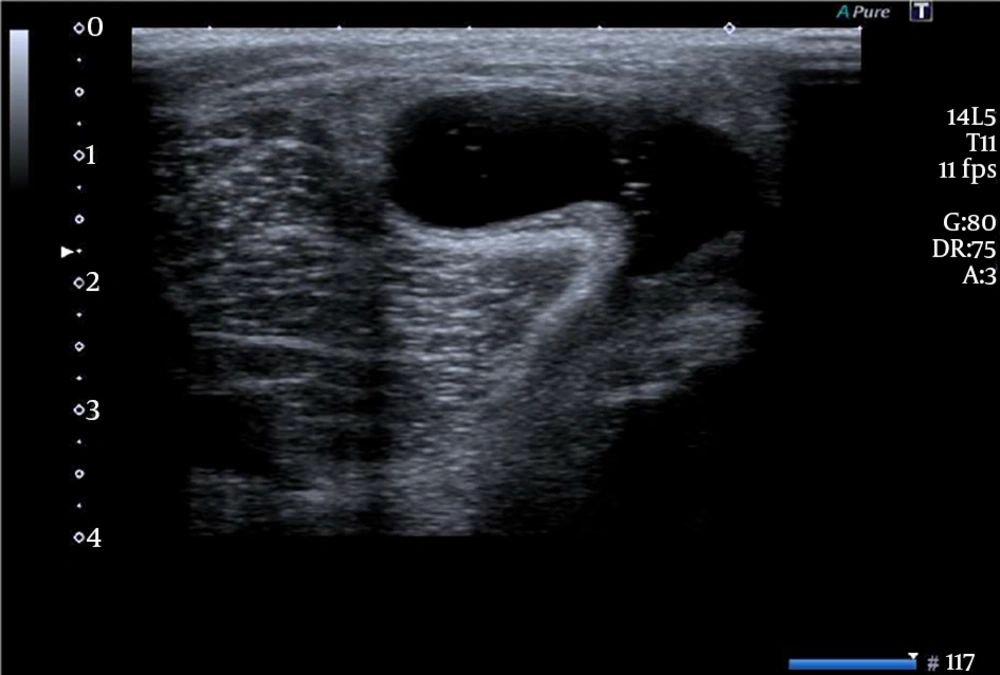
Posterior acoustic enhancement: Posterior acoustic enhancement results from the focal area of decreased impedance that leads to an increased transmission of sound waves to the tissue immediately below it. It is very common to observe this phenomenon in veins and cysts (Figure 3) (1, 5).
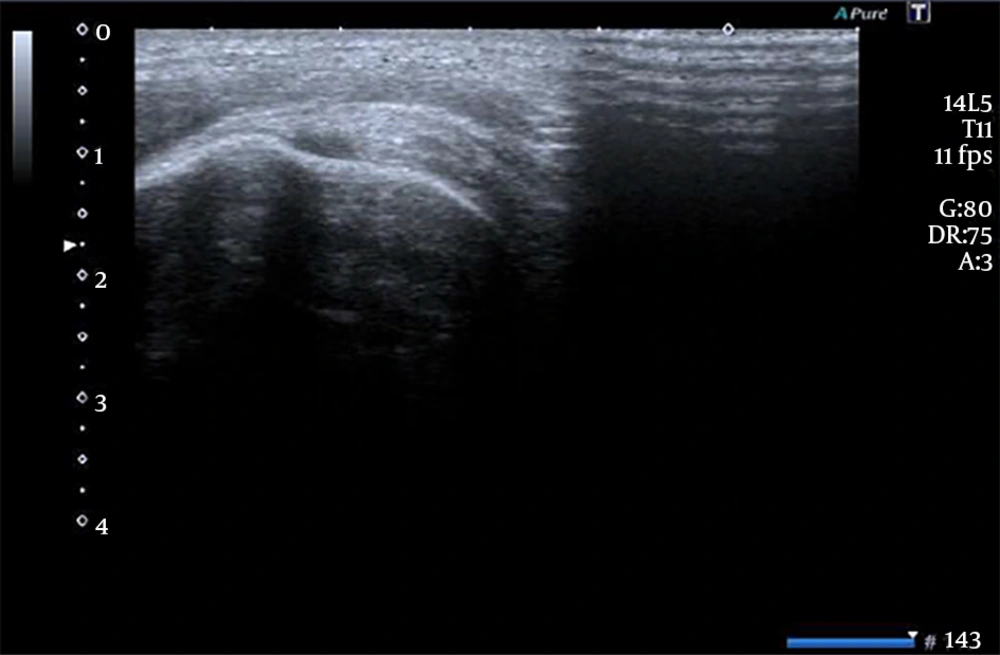
Inadequate conduction medium: US requires sufficient amount of conduction medium between the transducer and the skin of the patient for the sound waves to travel adequately from the transducer to the tissue and back to provide a clear image. Conduction gel or standoff pads might avoid this artifact since US waves do not conduct well through the air. This is commonly observed when Aquiles or fingers tendons are evaluated (Figure 4) (1, 5).
Reverberation artifact: Reverberation artifact occurs as a repetitive reflection back and forth between two highly reflective surfaces. In the rehabilitation settings, it is mostly observed with needle guidance or implants of metal. This artifact is observed as equally spaced hyperechoic lines that blur the image. This property let physicians guide needles on interventional procedures (Figure 5) (2).
2.3. Doppler Imaging
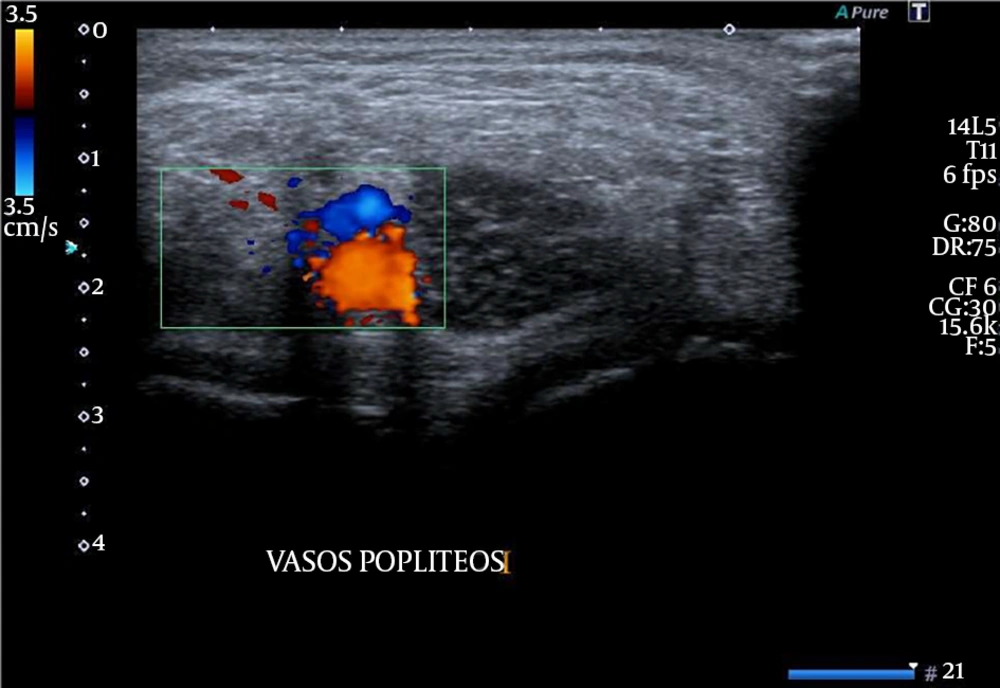
Doppler imaging is an important complement to the grayscale image in the routine US evaluation. It provides a color signal with movement, making it particularly useful for assessing vascular flow. It helps to identify vascular structures and can be used to assess for the increased vascularization in case of pathologic conditions such as synovitis or any inflammatory condition. Power Doppler is generally preferable for low flow states, as in inflammatory states, and color Doppler is used for higher flow states and assessment of direction, as in the vascular evaluation of clots, anatomic variations, and aneurysms. In color Doppler, the red color represents flow toward the transducer and the blue color represents flow away from the transducer (Figure 6) (1, 5).
2.4. Musculoskeletal Evaluation
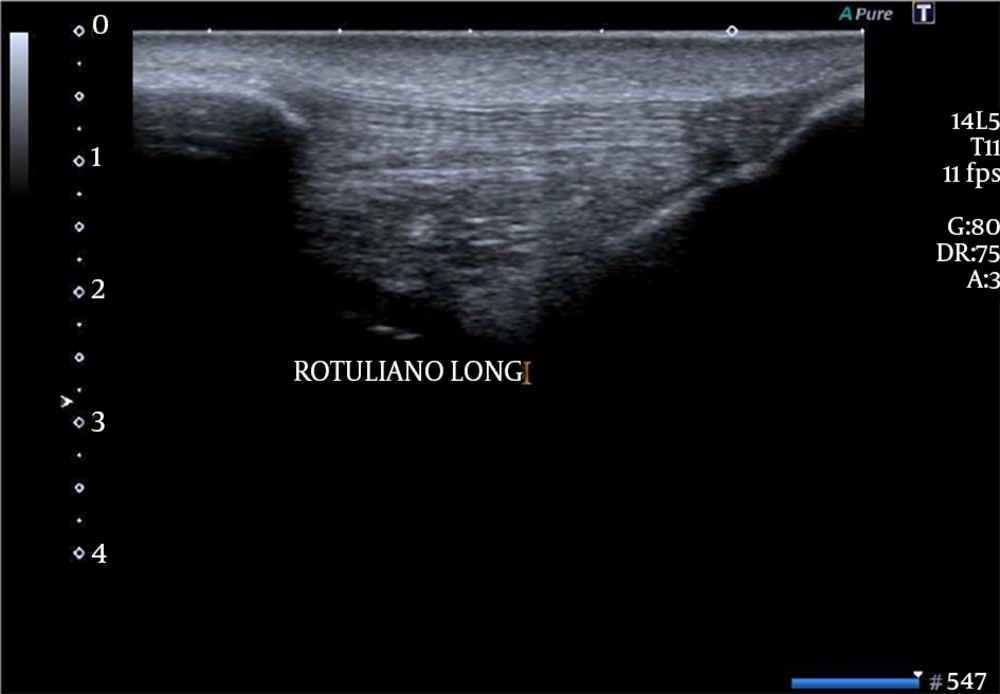
Tendon imaging: US is an excellent imaging modality for assessing tendons. Evaluation of tendon and tendinopathy is one of the most frequent uses of US in musculoskeletal medicine. Tendons are dynamic structures and highly visible with the high-frequency US. Tendons connect muscles to bones; therefore, they are important to be evaluated correctly. Tendons are constituted by fascicles of collagen; the fascicular pattern of fibers in the longitudinal view is observed in the picture, denoting hyperechoic images (Figure 7).
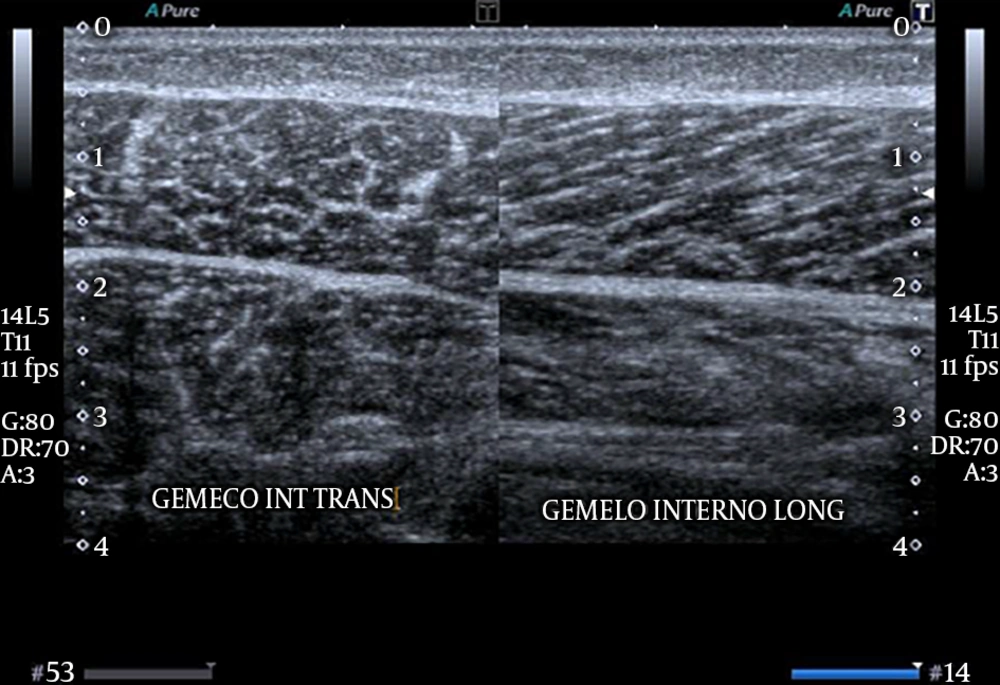
Muscle imaging: US provides high-resolution images of muscles and can detect even subtle abnormalities. The dynamic capabilities of US allow the identification of pathology not appreciable with static imaging. Muscles on the transversal view are defined as “sky with stars”. On the contrary, a longitudinal view shows fibers on parallel disposition. US allows the precise measurement of muscle size and detects atrophy, as well as echotexture changes, in muscle disease (Figure 8) (1, 4, 5).
Nerve imaging: US is an excellent modality for the evaluation of peripheral nerve tissue. The high resolution and dynamic capabilities allow the precise measurements of even subtle changes, detection of alteration of internal structure, and dynamic effect of surrounding tissue. Developing skills for imaging peripheral nerves can be used for proper tissue recognition in the musculoskeletal evaluation, diagnostic assessment of focal and generalized neuropathies, and in the identification of nerve blocking. The nerve is seen as a hyperechoic image due to the collagen that forms the perineurium and epineurium that surround it (Figure 9).
Mass imaging: A systematic approach to masses is needed for anybody involved in musculoskeletal ultrasound. Masses can be encountered incidentally in routine examinations and frequently are the representing complaint. Some features of evaluation include size, nature of borders, echotexture, compressibility, relationship with surrounding tissue, and relative vascularization. In the 1970 s, the first indication for US evaluation was to discriminate between Baker’s cyst from masses (Figure 3) (6).
Foreign bodies: US is an excellent modality for identifying foreign bodies. US is the ideal imaging modality for dynamic guidance at the removal of foreign bodies. Precise location helps to minimize any surgical exploration or improve the approach to percutaneous removal. Reverberation artifact is typical for foreign bodies and aids in the detection (1, 4).
For musculoskeletal evaluation, since structures are superficial, linear probes (7.5 MHz - 15 MHz) are better than convex probes (2.5 HMz - 7.5 MHz). Linear probes have lower penetration and better definition than convex probes; therefore, they are preferred on musculoskeletal evaluation (1).
3. Discussion
The musculoskeletal US is a technique that has extended in the last decade (4). Ozcakar et al. have reported 19 advantages for US imaging when compared to other techniques such as radiography, tomography, and magnetic resonance imaging (MRI); in fact, US is cheaper and less time-consuming than MRI (7).
US is an effective technique in the diagnosis of musculoskeletal pathologies; and, in the hands of a rehabilitation specialist, constitutes a dynamic, accurate, economic, and cost-effective tool (2).
Unfortunately, US is a very difficult and time-consuming technique (2). It is very important to be familiar with the knobology of the equipment to understand the physics and artifacts in US evaluation.
Images on US evaluation do not have an anatomical representation as radiographic, tomographic, or MR images do. A thorough knowledge of sonoanatomy is necessary to interpret such structures (2).
On the other hand, the technology has advanced in recent years and high-sensitive US probes are available on the market. Its spatial resolution has increased to an extent that its discrimination is 150 µm - 200 µm, far superior over the 450 µm discrimination obtained by MRI or the 1 mm resolution from radiographies (8-11).
It is very important to know US functioning since US equipment can be considered as a machine with a processor that configures electric signs obtained by a transducer to produce images (12).
It is of paramount importance to understand how images are obtained; therefore, a revision of physical terms such as acoustic impedance, attenuation, reflection, refraction, absorption, and scattering has been performed on this review article. These basic principles are necessary to perform US evaluation in the rehabilitation settings oriented to musculoskeletal pathologies.
There are different probes for US evaluation. Linear probes are mostly used in the musculoskeletal evaluation. US probes between 7.5 and 15 MHz offer a greater resolution but a lower depth. On the contrary, convex probes (2.5 MHz - 7.5 MHz) offer lower resolution but higher depth (12, 13).
Artifacts in US evaluation are images that do not correlate to real anatomical structures. Artifacts may shadow existent structures and/or show structures that really do not exist. The understanding of posterior acoustic enhancement or posterior acoustic shadow reflects this controversy on artifacts. Reverberation may help us identify metallic materials and guide on interventional procedures (13).
Doppler imaging may help us identify vascular structures and help us in quantifying inflammation on the surrounding tissue. US evaluation helps us identify musculoskeletal structures such as muscle, tendon, nerve, and artery/vein because of their own anatomical features. A correct integration of US basics, anatomy, and dynamic evaluation may help us diagnose musculoskeletal pathologies in the rehabilitation settings, all in a one-visit evaluation (2).
3.1. Conclusions
A correct understanding of principles and basics in ultrasound, artifacts, echotexture of muscle, tendon, nerve, and vessels is necessary to start a long-term learning curve in the musculoskeletal evaluation and the pathology related to such structures.