1. Background
Neck pain (NP) is a widespread and painful musculoskeletal disorder (1). Chronic neck pain (CNP) represents the bulk of the public health conditions such as poor psychological health, including cognitive distress, anxiety, and depressed mood (2), sleep disturbance (3) resulting in loss of work output at all levels (4). Neck pain is one of the key causes of disability worldwide and it was concluded that stakeholders in a clinical setting, government members, and health researchers need to focus more on the treatment of neck disability (5). Despite the predominance of neck pain, there is a paucity of research on the frequently used therapy (6).
A previous study showed that neck stabilization exercises (NSE) decreased pain and disability in patients with neck pain (7). There is a greater amount of proof on the efficacy of muscle energy technique (MET) in chronic pain condition (8). In spite of the recognition of stabilization exercise in the management of spine and pelvic dysfunction (9), there is a paucity of properly planned intervention studies to determine its effectiveness. The MET is a type of soft-tissue manipulation that uses isometric contraction before subsequent stretching or movement of restricted tissues (10). The mode of operation of MET was attributed to either post-isometric relaxation (PIR), which has an effect on the tissues that were isometrically contracted, or reciprocal inhibition (RI), which affects the antagonists to the tissues that have undergone contraction. It was reported that PIR and RI partially explain the benefits of MET (11), which are relatively pain-free joint and soft tissue motion after mild isometric contractions (12). The NSE is a form of a rehabilitation program that was developed for the purpose of relieving pain, improving function, preventing further injury (13) as well as improving the innate mechanisms by which the cervical spine keep up a stable and injury-free state (14).
Presently there are only limited published evidence-based researches to support their usefulness. A reduction in the function of the deep cervical flexor can result in a compensatory rise in activities of the superficial muscles around the neck and shoulder girdle, as well as muscle fatigue under sustained low loads (15). There is a lot of information that poor psychological health, including cognitive distress, anxiety and depression, loss of employment and reduction of income, and increased stress are associated with CNP (2). Artner et al. (3), in a study on the prevalence of sleep deprivation in CNP concluded that sleep disturbance should be assessed when patients with CNP are under treatment. There is also limited studies comparing MET and NSE in NSCNP patients with a wide range of interventions to manage neck pain with lack of effectiveness in some of them.
2. Objectives
This study compared the effects of MET and NSE on pain, neck disability, depression, anxiety, and sleep disturbance of patients with NSCNP.
3. Methods
This study is a single-blinded randomized controlled trial comprising thirty-five patients with NSCNP. They were recruited from the general out-patient department and physiotherapy department of 2 tertiary hospitals in Lagos state Nigeria. Inclusion criteria were the participants with a recurrent history of NSCNP of more than 3 months without any specific condition detected as the primary reason for the complaint, with pain level greater than or equals to 5/10. The participants with the previous history of spinal surgery, history of trauma to the neck, spinal deformity, and specific neck pain as a result of malignancy, narcotic drugs, and a previous history of physiotherapy intervention were excluded from the study.
3.1. Procedure
Participants’ physical characteristics, including age, sex, occupation, height, and weight were recorded before commencing the study. Baseline assessment of pain, neck disability, depression, anxiety, and sleep disturbance was done using numerical pain rating scale (NPRS), neck disability index (NDI), hospital anxiety depression scale (HADS), and insomnia severity index (ISI), respectively. Informed written consent was obtained from the participants while ethical approval was obtained from the Health Research and Ethics Committee of Lagos University Teaching Hospital, Nigeria with approval number (ADM/DST/HREC/APP/1535).
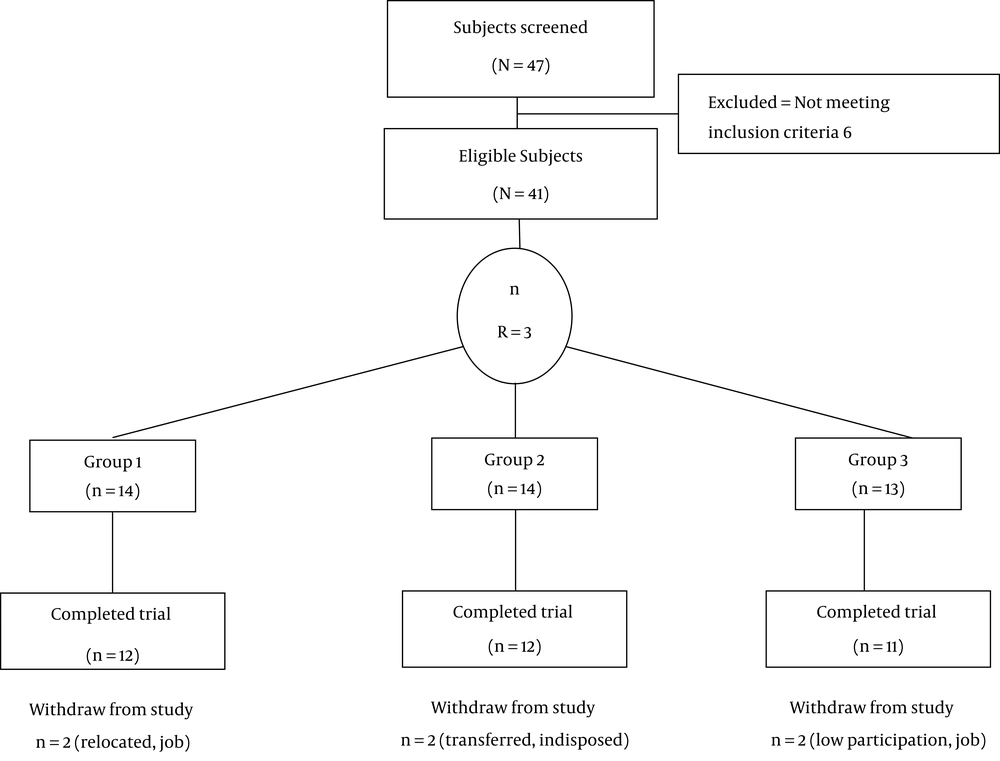
Out of the 47 participants screened for this study, 6 were found ineligible regarding the inclusion criteria and were excluded from the study. The 41 eligible participants were randomly assigned to 3 groups (1, 2, and 3), using the computer-generated random number sequence (Figure 1). The participants in group 1 received MET to the neck for 15 seconds (10), infrared radiation (IRR) and NCE (7). The participants in group 2 received NSE for 30 minutes (16), IRR, and NCE while group 3 received NCE and IRR to the neck. However, only 35 participants completed this study, 6 participants did not complete the study due to different reasons (Figure 1). The participants did this exercise two times a week for 8 weeks. Assessment of pain, neck disability, depression, anxiety, and sleep disturbance was done at baseline, end of 4th and 8th weeks.
3.2. Protocol for Neck Stabilization Exercise
Chin tuck, cervical extension, shoulder shrugs, shoulder rolls, scapular retraction 15 repetitions each for 30 minutes (16, 17).
3.3. Protocol for Muscle Energy Technique
The participant was in the supine lying position. The therapist was at the end of the bed near the participant’s head. The therapist assessed the movements of the cervical spine that were restricted. The therapist localized the joint or the body tissue into the position of the initial range of motion resistance to a specific movement. Once the therapist feels the restriction, the participant’s cervical spine was positioned in that range and then a resistive force was applied. In this regard, the patient was asked to isometrically contract for 5 seconds, but not to overcome the force of the therapist; then the counterforce by the therapist was ceased slowly and the participant was asked to relax. The therapist then took the joint to a new barrier and the same procedure was repeated 3 times (10, 18).
3.4. Protocol for Neck Care Education
Participants were advised to relax, activate, and adopt stress-coping skills, workplace ergonomics, and self-care strategies (19). The NPRS is an 11-point scale for patient’s self-report of pain. The NPRS can be administered verbally or graphically for self-completion, scores ranged from 0 - 10 points, with higher scores indicating greater pain intensity. It has a construct validity ranging from 0.86 to 0.95 (20).
3.4.1. The NDI
This is a self-administered questionnaire listing activities that can be compromised by neck pain. The NDI consists of 10 items to measure disability secondary to neck pain. The score ranges from 0 - 50, with 0 - 4 representing no disability and 34 and above representing severe disability with test-retest reliability of 0.55 (21).
3.4.2. The ISI
This is a self-administered questionnaire, which is an outcome measure to determine the severity of sleep disorder. It is a 7-point scale listing the problems associated with falling and staying asleep. The score range from 0 - 28 with a reliability of 0.74 (22).
3.4.3. The HADS
This is a widely used self-report questionnaire for detecting overall states of anxiety and depression in non-psychiatric medical contexts (23). It consists of 14 items, which are statements to be scored on 4-point Likert scale (0 - 3), generating ‘anxiety’ or ‘depression’ scores ranging from 0 to 21 (total score = 0 - 42). It has a reliability of 0.73 for anxiety and 0.77 for depression.
3.5. Data Analysis
Statistical Package for Social Science (SPSS Inc., Chicago, Illinois, USA) version 22.0 for windows package was used for data analysis. Quantitative data were expressed as mean and standard deviation (SD). Baseline and 8-week intervention values were recorded using Wilcoxon sign rank test and paired t-test. Analysis of variance (ANOVA) test and Kruskal Wallis test were used to summarize baseline, end of 4th week and 8th week values post-intervention. Least significant difference (LSD) post hoc analysis was done to compare the mean changes in the three groups in order to determine the significant difference at the alpha level of 0.05.
4. Results
A total of forty-one (41) participants with non-specific chronic neck pain participated in the study, while 35 subjects completed the study. Twenty-three (65.7%) of the participants were females and 12 (34.3%) were males. The 3 groups did not differ significantly in their physical characteristics (Table 1).
4.1. Outcome Measure Parameters Across the Three Groups at the End of 4th Week, and 8th Week
The result showed that there was a significant difference at the end of the 4th and 8th week post-intervention for pain severity (P = 0.01, 0.004), neck disability (P = 0.01, 0.001), and sleep disturbance (P = 0.02, 0.002). The post-hoc analysis showed that there were significant differences between MET and NCE groups and NSE & NCE for pain, neck disability, and sleep disturbance (Table 2). Paired t-test showed that there was a significant difference (P < 0.05) between pre- and post-treatment interventions for pain in all the groups. Wilcoxon test showed that there was a significant difference between the pre- and post-treatment interventions for the outcome measures across the groups (Table 3).
| Outcome Measure | Group 1b | Group 2c | Group 3d | Fe | Hf | P Value |
|---|---|---|---|---|---|---|
| Pre-Rx Baselineg | ||||||
| Pain | 5.92 ± 2.11 | 7.67 ± 1.83 | 5.36 ± 1.91 | 4.42 | 0.02h | |
| ND | 28.67 ± 14.53 | 34.50 ± 13.81 | 27.27 ± 11.32 | 2.41 | 0.30 | |
| P (ANX) | 4.75 + 4.372 | 9.00 ± 5.39 | 5.09 + 3.42 | 4.80 | 0.09 | |
| P (DEP) | 5.00 + 3.954 | 9.00 ± 5.71 | 5.09 + 3.75 | 4.44 | 0.11 | |
| SD | 6.00 + 3.814 | 11.08 + .055 | 9.27 + 6.635 | 6.87 | 0.03h | |
| Mid-Rx 4th week | ||||||
| Pain | 2.92 ± 1.51 | 5.08 ± 1.31 | 3.91 ± 1.81 | 5.89 | 0.01h | |
| ND | 12.50 + 4.83 | 23.33 + 9.43 | 23.27 + 11.77 | 9.88 | 0.01h | |
| P (ANX) | 2.67 + 3.393 | 4.67 + 2.90 | 3.91 + 3.05 | 3.01 | 0.22 | |
| P (DEP) | 2.67 + 3.143 | 5.75 + 4.67 | 4.18 + 2.96 | 3.39 | 0.18 | |
| SD | 3.75 + 2.896 | 7.42 + 2.746 | 7.91 + 5.683 | 7.73 | 0.02h | |
| Post-Rx 8th week | ||||||
| Pain | 1.75 ± 1.14 | 1.83 ± 0.72 | 3.18 ± 1.25 | 6.58 | 0.004h | |
| ND | 7.17 ± 3.56 | 12.00 ± 6.21 | 9.27 ± 6.64 | 13.85 | 0.001h | |
| P (ANX) | 1.58 + 2.109 | 2.50 + 2.02 | 3.27 + 2.45 | 3.44 | 0.18 | |
| P (DEP) | 2.00 + 2.796 | 3.00 + 3.30 | 3.18 + 2.82 | 1.57 | 0.46 | |
| SD | 1.67 + 2.270 | 2.17 + 1.467 | 6.91 + 5.338 | 12.29 | 0.002h |
Across Group Comparison of Pain, Neck Disability, Depression, Anxiety and Sleep Disturbance at Baseline, End of 4th Week, and 8th Week Post-Interventiona
| Outcome Measure | Pre-Rxb Baseline | Post-Rxb End of 8th Week | tc | Zd | P Valuee |
|---|---|---|---|---|---|
| Group 1f | |||||
| Pain | 5.92 ± 2.11 | 1.75 ± 1.14 | -7.42 | 0.001 | |
| ND | 28.67 ± 14.53 | 7.17 ± 3.56 | -3.06 | 0.002 | |
| P (ANX) | 4.75 ± 4.37 | 1.58 ± 2.11 | -2.43 | 0.02 | |
| P (DEP) | 5.00 ± 3.95 | 2.00 ± 2.80 | -2.55 | 0.01 | |
| SD | 6.00 ± 3.81 | 1.67 ± 2.27 | -2.61 | 0.01 | |
| Group 2g | |||||
| Pain | 7.67 ± 1.83 | 1.83 ± 0.72 | -12.31 | 0.001 | |
| ND | 34.50 ± 13.81 | 12.00 ± 6.21 | -3.07 | 0.002 | |
| P (ANX) | 9.00 ± 5.39 | 2.50 ± 2.02 | -3.07 | 0.002 | |
| P (DEP) | 9.00 ± 5.71 | 3.00 ± 3.30 | -3.06 | 0.002 | |
| SD | 11.08 ± 0.55 | 2.17 ± 1.47 | -3.06 | 0.002 | |
| Group 3h | |||||
| Pain | 5.36 ± 1.91 | 3.18 ± 1.25 | 8.28 | 0.001 | |
| ND | 27.27 ± 11.32 | 9.27 ± 6.64 | -2.99 | ||
| P (ANX) | 5.09 ± 3.75 | 3.27 ± 2.45 | -2.21 | 0.03 | |
| P (DEP) | 5.09 ± 3.75 | 3.18 ± 2.82 | -2.38 | 0.02 | |
| SD | 9.27 ± 6.64 | 6.91 ± 5.34 | -2.53 | 0.01 |
Within Group Comparison of Pain, Depression, Anxiety, and Sleep Disturbance at Pre-Treatment (Baseline) and Post-Treatment (End of 8th Week)a
5. Discussion
This study revealed that MET, NSE, and NCE provided considerable benefit to NSCNP patients when it was administered to them. There was a noticeable improvement in outcome measure parameters of pain and neck disability in the MET group, NSE group as well as the control group post-intervention. This finding supports the reports of the study outcome by Dusunceli et al. (7) who reported that multimodal care approach or intervention in the management of NSCNP is beneficial in the treatment of patients with neck pain. The outcome of this study revealed a considerable improvement in pain associated with NSCNP in both MET and NSE groups in comparison to the control group after 8 weeks of treatment. This is consistent with the findings of Phadke et al. (18) who revealed that MET reduced pain in patients with non-specific neck pain.
The reduction in pain in MET is as a result of painful inhibition, through both the ascending and descending neurological passageway, after the activation of muscle and joint mechano-receptors over the course of the isometric contractions. It is noteworthy to know that throughout the contractions, endogenous pain-inhibiting chemicals are released, including endocannabinoids, enkephalins, and endorphins (24). This finding did not conform to the report of Strunk and Hondras (25) who revealed that the pain of the studied participants worsened in the MET group. Abdel-Aziem and Draz (26), concluded in their study that neck flexor exercises improved pain and physical disability in patients with neck pain. The mechanism by which stabilization exercises cause reduction of pain in patients with NSCNP is that the exercise may increase the movement in the neural pathways, thus causing a restrictive effect on pain centers in the central nervous system leading to contraction of muscle and tension on different tendons and ligaments as well as stimulation of the mechanoreceptors and enhancement of the activity of the sensory nerve; consequently, results in the inhibition of the mediating pain pathways (13).
In this study, there was an improvement in the neck disability in both MET and NSE groups compared to the control. This corroborates the findings of a previous study by Ylinen et al. (27) on NSE and Phadke et al. (18) on MET among CNP patients. The impact of MET was moderated by the afferent input from the proprioceptive sensory receptor organ, which occurs when a muscle is contracted isometrically, the afferent feedback inhibits the muscle, resulting in relaxation when the contraction is released. It is useful when the tightness of the muscle is a major causal factor to somatic dysfunction. The outcome of this study revealed improvement in sleep disturbance in the MET group, NSE, as well as the control groups post-intervention. To the best of the researcher’s knowledge, this study is the only one in this situation that measures the effect of these interventions on sleep disturbance. The improvement in sleep disturbance following the intervention could be due to the relaxing effect of exercise, as well as sedative effect of IRR on superficial nerve endings, which can also facilitate muscle relaxation.
It was observed that all the intervention groups (MET and NSE) improved the psychological status (anxiety and depression) post-intervention. This agrees with the result of other studies (17, 28), which recorded an improvement in the level of depression when neck muscles were treated with therapeutic exercises. The reason for the marked improvement in the psychological status may be that there was an improvement in the pain and disability of patients with NSCNP after undergoing MET and NSE. The control (NCE) group showed improvement in the clinical outcome of pain, neck disability, depression, anxiety, and sleep disturbance. This is consistent with the previous study by Chen et al. (29) on relief of pain symptoms while the report of the study by Dusunceli et al. (7) revealed the lack of reduction in the level of depression. This result is not in accordance with a report of a systematic review by Gross et al. (19), which revealed that neck care education has limited effect in the management of neck pain. The improvement of outcome measures in the control group may be due to a number of factors, including the psychological effect of being treated, biological variation in the participants, and spontaneous or natural recovery.
5.1. Limitation
The sample size for this study was small and the follow-up was a short duration (8 weeks). Therefore, caution should be considered in generalizing the outcome of this study.
5.2. Conclusions
In this study, NSE, MET, and NCE were shown to be effective in the improvement of pain, disability, psychological status, and sleep disturbance of patients with NSCNP. It was concluded that neck stabilization exercise provides a better benefit when compared with the other 2 interventions (MET and NCE) in the improvement of the outcome parameter.
5.3. Recommendation
It is therefore advised that physiotherapists can suitably make use of any of the three interventions (MET, NSE, NCE) in the treatment of patients with NSCNP, but preferably NSE for better effect.