1. Background
Knee osteoarthritis (OA) is the most prevalent joint disease, with an estimated prevalence of about 12.2% - 33% in the general population (1-3). Patients with knee OA suffer from a variety of clinical symptoms such as pain, joint stiffness, progressive muscle atrophy, and joint instability, which seriously impact patients’ quality of life (3). The principal pathological feature of knee OA is progressive cartilage degradation (3), which its exact mechanism not known yet. However, according to biomechanical theory, subchondral microfractures resulting from repetitive impulsive joint loading might engender cartilage depletion in knee OA (4). Accordingly, evaluation of knee joint forces during the activities of daily living has always been the focus of biomechanical investigations of knee OA.
Though in-vivo measurement of joint forces is not possible due to ethical concerns, research reveals that the knee adduction moment (KAM) represents the amount of the load imposed on the medial knee compartment with acceptable accuracy (5-7). The KAM significantly correlates with medial compartment force (5, 6), medial to lateral cartilage thickness ratio in both the femur and the tibia (8), severity of knee OA (9, 10), and the risk factors of OA such as age, sex, and obesity (11-13). These findings support a hypothesis that treatment interventions, which can reduce the KAM, may detain the progression of knee OA, and improve patients’ symptoms (14).
Exercise therapy plays an essential role in the non-pharmacologic conservative treatment of knee OA (15). The results of randomized clinical trials indicate that exercise therapy is effective in improving muscle strength, the range of motion, joint proprioception, balance, and cardiovascular function in patients with knee OA (16-18). There are different methods of exercise therapy for knee OA. However, there is a lack of evidence to support the superior efficacy of any of these practices over others (18, 19). In addition, there is no study to suggest that these exercise therapy regimens may reduce the KAM in patients with knee OA (14). For instance, Foroughi et al., and Bennell et al., showed that strengthening and neuromuscular exercises could not reduce the KAM in patients with knee OA (20, 21).
More recent studies showed that voluntary changes in gait pattern, including toe-out gait (22, 23), relatively slow walking (24), increasing mediolateral trunk sway (22, 25) and medial thrust (MT) gait (26-28) may decrease the KAM in knee OA. MT gait, walking with knee internal rotation, is preferable to other gait modifications because it resembles the normal gait, and causes a higher reduction of the first and second peaks of KAM when compared with other gait modification techniques in vitro study (28). Recent research also found that some yoga exercises, the warrior lunge, and the goddess squat, can reduce the KAM (29, 30). The warrior lunge and goddess squat are the modified versions of the squat and lunge exercises with a particular alignment in the lower limbs, which can increase muscle strength, improve balance, and significantly produce less KAM when compared with traditional squat and lunge exercises (29, 30).
An increased KAM is considered as a primary risk factor for development and progression of knee OA (31). However, the clinical efficacy of the exercises, which potentially influence the KAM, has not been examined yet.
2. Objectives
In this randomized controlled trial (RCT), we aim to examine the effectiveness of the MT gait training, and yoga exercises on the amount of KAM, pain, and function in people with knee OA, in comparison to the routine resistive knee extension/flexion exercises.
3. Methods
3.1. Study Design
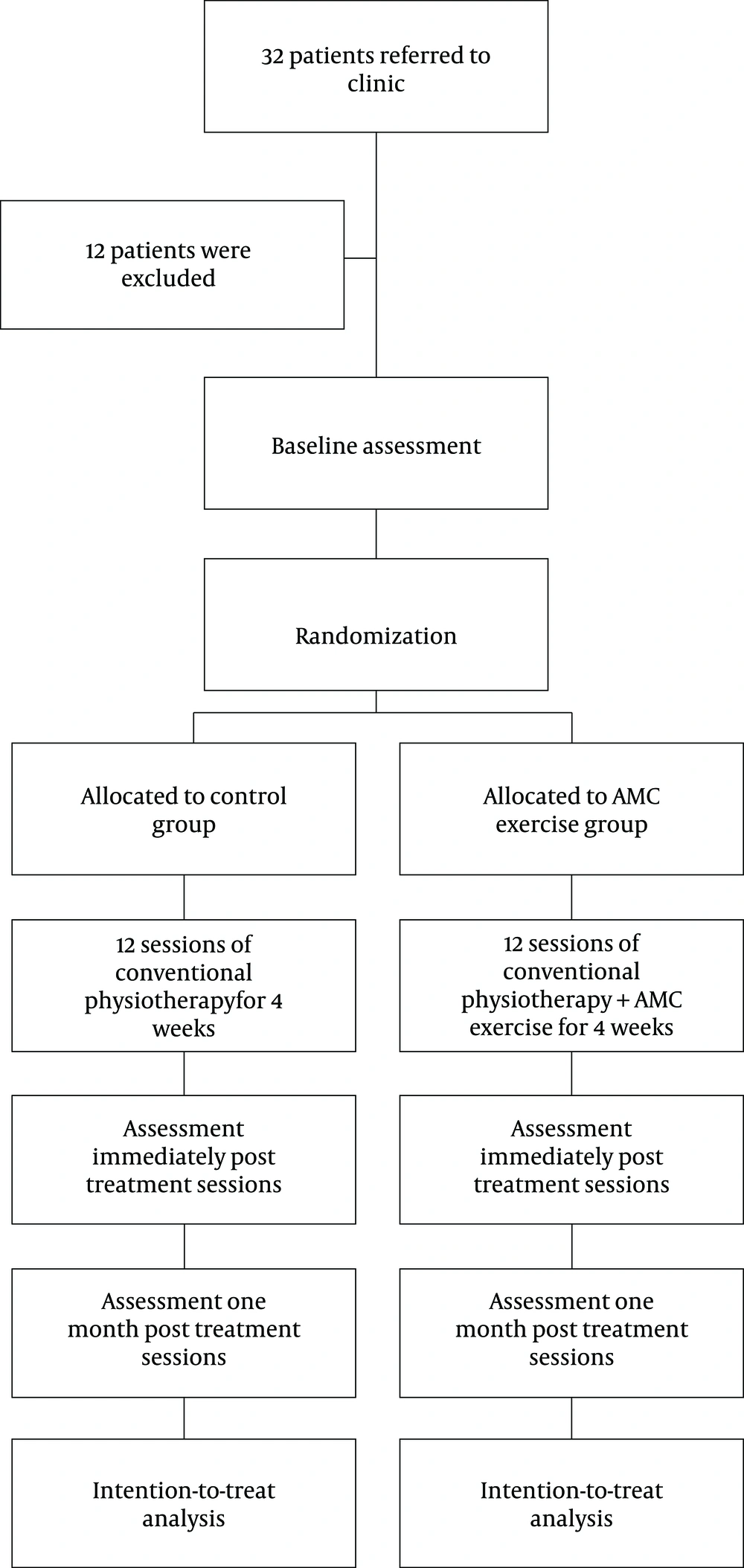
Double-blinded (data analyst and assessor), parallel design randomized controlled trial, which conforms to CONSORT guidelines for non-pharmacological studies (Figure 1).
3.2. Setting
This trial will be conducted in the Mowafaghian Research Centre of Intelligent Neuro-Rehabilitation Technologies.
3.3. Participant
Patients with unilateral and bilateral knee osteoarthritis will be recruited from rheumatology clinics located in downtown Tehran, near the research center. They will be examined by an experienced physical therapist for inclusion/exclusion criteria. The inclusion criteria will include the age of 45 - 76 years, pain severity of greater than 30 based on a 100 mm visual analogue scale (VAS), a history of symptoms for more than a month, ability to walk without assistive devices, and mild to moderate (grade 1 - 3) tibiofemoral joint osteoarthritis, according to the Kellgren and Lawrance classification system (32).
The exclusion criteria will include a history of systemic arthritis, diabetes, neuromuscular diseases, uncontrolled hypertension, uncontrolled cardiovascular and respiratory diseases, surgery or injection in the lower extremity joints in the last six months, prior hip or knee joint replacement or tibial osteotomy surgery, symptomatic hip OA, recent (last month) trauma to the knee joint, and extreme physical weakness. We will also exclude patients who take oral corticosteroid treatment and those who have taken other nonpharmacologic treatment within the past six months.
3.4. Procedure
Patients with knee OA will be recruited from public and private rheumatology clinics located in downtown Tehran. The office staffs at the clinics to be invited into the study will contact them.
Eligibility for volunteers first will be assessed by telephone screening. An experienced physiotherapist will then screen prospective participants for eligibility based on inclusion and exclusion criteria and knee X-ray findings. Eligible participants will receive information about the study and sign a written consent if they agree to participate. This study received approval from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1396.317) and is registered in the Iranian Registry for Clinical Trial (IRCT201702222793N4).
Patients will be assessed for the outcome measures at the baseline (pre-intervention), one-day and one month after the interventions. An assessor, blinded to group allocation, will conduct baseline and follow-up assessment at Mowafaghian Research Centre of Intelligent Neuro-Rehabilitation Technologies. After the baseline assessment, participants will be randomly allocated to the YogaMT and the conventional physiotherapy group. Participants in both groups will receive 12 sessions of physiotherapy, three sessions per week for four weeks, with at least 24 hours between the sessions.
3.5. Randomization and Allocation Concealment
Covariate adaptive randomization technique (33) will be used to allocate participants to either the YogaMT and the conventional physiotherapy group. First, 10 participants will be randomly assigned to the treatment groups using sequentially numbered, opaque, sealed envelopes, which will be selected by a third party who has no other role in the RCT. Then, Taves method will be used to assign other participants to the groups (34). The envelopes will be kept in a locked drawer and will only be accessible to the person responsible for randomization. The tibiofemoral joint osteoarthritis severity and pain severity will be matched in both groups.
3.6. Outcome Measures and Measurements
Participant’s characteristics including age, gender, height, and weight, will be recorded at the first visit. The outcome measures are the amount of KAM, pain severity, and functional level, which will be assessed as follow.
3.6.1. Pain
Patients will be asked to rate the severity of their pain using a visual analog scale (VAS) and the short type of WOMAC scale. VAS is a 100-millimeter line graded from 0 (no pain at all) to 100 (the most severe pain that I can imagine) (35). The short WOMAC scale consisted of eight questions about the patient’s assessment of his pain severity in daily activities. Each question is graded from zero (no problem) to four (severe problem). Higher scores indicate higher pain in daily activities (36).
3.6.2. Function
The 2-minute walk test (2MWT) will be employed to assess patients’ functional ability.
Participants will be instructed to “walk as quickly and safely as they can for 2 min, back and forth along a well-lit 25-m tiled hallway. The total distance traveled for 2 min will be recorded (37). Participants will practice walking before the actual test; however, to prevent fatigue, the complete 2MWT will not be practiced.
3.6.3. The KAM
For evaluating the first maximum external knee adduction moment during gait, motion and the ground reaction force data will be recorded while participants walk barefoot along a 10-m pathway at a self-selected speed. A Vicon motion analysis system (Vicon Oxford, Oxford, UK), with 12 cameras at a sampling frequency of 120 HZ will be used to record the motion data. The ground reaction force data will be collected by two Kistler force plate systems (Kistler Force Plate, Winterthur, CH) at a sampling rate of 1200 Hz. Walking speed will be measured by a photoelectric beam sensor.
Three-dimensional reflective landmarks will be bonded bilaterally on the acromioclavicular joint, medial epicondyle of the humerus and distal ulnar head, the anterior superior iliac spine (ASIS) and the posterior superior iliac spine (PSIS), the lower lateral 1/3 surface of the thigh, the lateral epicondyle of the knee, the lateral malleolus, and second metatarsal head (38).
Participants will perform two familiarization trials, and five test trials of walking with a 30-second rest interval between the trials. The 3D marker positions will be filtered using a low-pass Butterworth filter with a cutoff frequency of 6 Hz. The KAM will be determined using inverse dynamics via the Plug-in-Gait model, programmed in Vicon Nexus 2.6 software (Vicon Oxford, Oxford, UK) (38). The recorded KAM for each patient will be averaged of all trials.
3.7. Intervention
3.7.1. The YogaMT Group
The exercise therapy in the YogaMT group comprises medial thrust gait training, goddess squat, and warrior lunge training. MT gait pattern is defined as walking with internal rotation of the hip (about 18º) and slightly knee flexion (to about 19º - 20º) (28). Participants in this group will receive instruction about MT gait pattern in a separate session before the beginning of treatment. They will practice walking with MT pattern at their selected speed for 20 minutes in each treatment session. When necessary, the participant receives verbal feedbacks during training. Participants will be asked to wear the same comfortable pairs of shoes during the assessment, training and treatment sessions.
They also perform the goddess and warrior exercises, three times each with the least rest interval of 40 seconds. For the goddess exercise, participants will be asked to stand bilaterally, with the feet in about 45º externally rotated position and slightly greater than shoulder width apart, and hands on the pelvis. Then, they will squat down to about 30º of knee flexion while maintaining the pelvic and torso upright, and sustain this posture for 30 s. For the warrior exercise, participants will be asked to step forward with the right/left leg while looking forward and keeping their torso and pelvis straight, then bend the right/left knee until their thigh is parallel to the floor and the thigh and shank are perpendicular to one another (Figure 2).
In the warrior lunge exercise subject stand bilaterally, with the feet in about 45º externally rotated position and slightly greater than shoulder width apart, and hands on the pelvis (left) and in goddess squat exercises subject squat down to about 30º of knee flexion while maintaining the pelvic and torso upright (right).
Table 1 showed progression levels of goddess and warrior exercises (29). The level of difficulty of the goddess and warrior exercises will be adjusted based on the Borg Perceived Exertion Scale (29). When the intensity of physical activity during the yoga exercises falls below 5 (moderate sweating and easy talking), the exercise will be upgraded to the next level (39) .If the participant feels pain (VAS ≥ 5), the duration of practice will be reduced, and the exercise will be downgraded to the previous level if needed.
| Level 1 | Level 2 | Level 3 | Level 4 | |
|---|---|---|---|---|
| Goddess squat | Hands on hips, knees flexion to 30º | Hands on hips, knees flexion to 60º | Shoulders flex to 90º, elbows straight, knee flex to 60º | Arms overhead, knee flex to 80º |
| Warrior lunge | Hands on hips | Shoulders flex to 90º with elbows straight | Arms overhead | Arms overhead, look up to the ceiling for added challenge |
3.7.2. Conventional Physiotherapy Group
Treatment in the conventional physiotherapy group consists of three sets of resistive knee extension/flexion exercises with two minutes interval using the quadriceps chair. In the first session of each week, the maximum load that each participant can lift to complete ten Repetition Max (10 RM) without pain will be determined to adjust the amount load for each exercise. The amount of resistive load will be progressively increased from 60% - 65% of 10 RM in the first set to 70% - 75% of 10 RM in the second set and 80% - 85% of 10 RM in the third set (40, 41). If participants report pain during exercise (VAS ≥ 5), they will be instructed to perform the exercise only in a pain-free range. If the pain still persists, the load will be reduced (42).
Participants in both groups will also receive a five minute continuous ultrasound (1 MHz, 1-1.5 W/cm2) on the front of the knee, TENS for 20 minutes (100 Hz, 50 µs pulse duration), thermotherapy with a hot pack for 20 minutes. They will be instructed to avoid sitting in a cross-legged position, kneeling, and prolonged standing.
3.8. Sample Size
Twenty patients will be recruited to a pilot study. After the intervention, the number of participants in each group will be calculated by sample-size power analysis (β = 0.20 and α = 0.5) based on the mean changes of the peak KAM during the stance phase of walking.
3.9. Statistical Analysis
For each outcome variable, a 2-by-3 (intervention by time) mixed-model analysis of variance (ANOVA) with a repeated factor of time will be performed to determine whether the mean difference of the outcome variable differ between the groups across the times of evaluation. The pairwise comparisons with Bonferroni adjustments will be used to locate significant differences when appropriate. We use IBM SPSS Statistics 22 (SPSS Inc, Chicago, IL) for statistical analysis. Significance levels will be set at P < 0.05.
4. Discussion
Exercise therapy is an essential element for the treatment of knee OA (15). However, research showed only short-term improvement of clinical symptoms using routine exercise therapy regimens (14). For a more efficient treatment of knee OA, physiotherapists should explore exercise therapy protocols, which may reduce the progression rate of the disease by targeting potential predictive factors to OA. Research indicates that increased KAM may contribute to the initiation of knee OA and the disease progression (9). A combined exercise therapy protocol including yoga exercises and medial thrust gait training may introduce a more powerful tool with longstanding treatment outcomes. In addition, YogaMT program is an inexpensive treatment that can be performed at any place and time. We expect the results of this RCT help to find a more effective treatment for patients with knee OA.