1. Background
Menopause is one of the developmental stages in the life cycle of women who experience it with aging. During this period, women undergo physical changes affecting their socio-mental status (1). In this period, the prevalence of depressive symptoms has been reported higher (2). It is estimated that 26% to 33% of women experience the first depressive symptoms of their life in the menopausal period (3). Depressive symptoms consist of chronic fatigue syndrome, restlessness, concentration problems, and sleep disorder (4). Anxiety-related disorders are accompanied by feelings of extreme concern, irrational thoughts, and believing in unfortunate events (4). Anxiety prevalence is assessed to be 7.3%, ranging from 5.3% to 10.4% (5).
Menopause has a significant effect on perceived stress among women. Stress as the response of the body to internal and external threats and relevant consequences (6) potentially exacerbate the menopause symptoms (7).The percentage of women with stress (88.8%) is much higher after the menopause (8). The information concerning whether the levels of perceived stress are related to age is scarce (9). A few investigations have discovered a decrease of perceived stress with increasing age (10, 11); others demonstrated no differences between younger and older adults (9, 12).
The prevalence of vitamin D deficiency has been accounted for 31% - 70% in postmenopause (13, 14). In a cohort study, a low amount of vitamin D was related to the prevalence of depressive disorder (15). Vitamin D deficiency was related to depression and mental health-associated life quality (16). In a systematic review, there was a positive correlation between vitamin D deficiency and psychiatric disorders (17). The effect of vitamin D in the elderly population on depression has not been studied extensively. Also, there is a controversy in the relationship between vitamin D and depression (18). There was no relationship between vitamin D and depression in some studies. Pan et al. (19) and Zhao et al. (20) also reported no significant relationship between vitamin D levels and depression.
Also, a direct relationship has been observed between psychosomatic symptoms and hormonal changes with estrogen reduction (2), and depression can be related to decreased estrogen (7). In addition, menopause symptoms are attributed to estrogen deprivation (21), and postmenopausal women lose the protective effects of estrogen (22). Moreover, in a meta-analysis of 28 studies, the serum levels of vitamin D were associated with the incidence of metabolic syndrome, body mass index (BMI), diabetes, hypertension, and heart disease (23).
However, the evidence is inadequate regarding the relationship between vitamin D and estrogen with stress, depression, and anxiety in postmenopausal women, as well as no study found the prevalence of depression, stress, and anxiety in postmenopausal women in Semnan. Therefore, this study aimed to evaluate the levels of vitamin D and estrogen-related to depression, anxiety and perceived stress in postmenopausal women.
2. Objectives
The objective of this study was to determine the prevalence of depression, anxiety, stress, and their association with vitamin D and estrogen levels in postmenopausal women in Semnan.
3. Methods
This study was approved by the Ethics Committee of Semnan University of Medical Sciences under the No. IR.SEMUMS.REC.2015.146, dated 14.02.2015. The present analytical cross-sectional study was conducted on women in different regions of Semnan using multistage sampling. In a preliminary study consisting of 40 postmenopausal women, the correlation coefficient between vitamin D and depression, anxiety, and stress was -0.267, -0.331, and -0.295, respectively. Considering the 95% confidence and power 80% of the sample size of the below equation, it was estimated that the maximum was 108, thus 120 people were examined in this study.
The inclusion criteria were the willingness to participate in the study and the consent to this, passing at least 12 months without menstruation, they have been postmenopausal, naturally and without surgery of the uterus and ovaries, and age range of 45 to 70 years. The exclusion criteria were cancers, a history of a physical disability or a clear mental disorder, hearing or visual impairments, preventing proper communication, a history of the stressful event in the last six months, and a history of depression and anxiety before the menopause.
Data collection tools were a demographic questionnaire, Spielberger State-Trait anxiety inventory, Beck depression inventory (BDI), and the perceived stress scale. The subjects responded to the 21-item Beck depression inventory on a four-point scale that ranges from 0 to 3 (24). The validity and reliability of this questionnaire were confirmed (25). Spielberger State-Trait anxiety inventory has 40 items; responses are rated on a 4-point Likert scale and range from 1 to 4 (26). Validity and reliability of the Spielberger anxiety inventory were confirmed (27). The validity and reliability of the perceived stress scale consist of 14 questions, with a range of scores in the Likert scale from zero to four (28).
After obtaining informed consent, blood sampling was carried out in the middle of summer (August) at the site of the central laboratory. Blood (5 cc) was taken at intervals of 8 - 9.30 a.m. from each person. The sample of blood was taken by a female laboratory expert. The level of serum 25 hydroxyvitamin D (ng/mL) and estrogen (pg/mL) were determined by using the ELISA method. The kit of EUROIMMUN AG (Lübeck, Germany) used to determine the serum level of 25 hydroxyvitamin D and the level of estrogen was determined by using of IAP (USA), according to the manufacturer’s instruction.
The ethical considerations of this study included obtaining approval from the Ethics Committee of the Semnan University of Medical Sciences, explaining the research objectives, keeping the information confidential, ensuring the satisfaction of subjects and obtaining written informed consent. The data were analyzed using SPSS version 18 software with Shapiro-Wilk, Mann-Whitney, Pearson correlation coefficient, and partial correlation coefficient. The significance level was considered to be less than 0.05.
4. Results
The current study was conducted on 120 postmenopausal women in Semnan. The mean age of women was 55.6 ± 5.4 years. In terms of marital status, 91.7% were married and the remaining 8.3% were widows. The mean number of children in these women was 3.3 ± 1.3. Furthermore, 20.8% of women had a history of heart disease, 30% hypertension, 8.3% digestive disease, and 31.7% diabetes (Table 1). Also, 85.8% (n = 103) of them were homemakers and the rest were employed (4.2%), self-employed (1.7%), and retired (8.3%). No significant correlation was found between body mass index (BMI) and the levels of depression, anxiety, stress, vitamin D, and estrogen (Table 1). In the two groups of patients with and without diabetes, digestive disease, hypertension, and heart disease, the levels of depression, anxiety, stress, vitamin D, and estrogen showed no significant difference (Table 1). There was a positive and significant correlation between age and vitamin D (Table 1). However, no significant correlation was found between age and estrogen levels, depression, anxiety, and stress (Tables 1 - 3).
| Characteristic | No. (%) | r (P Value) | ||||
|---|---|---|---|---|---|---|
| Depression | Anxiety | Stress | Vitamin D | Estrogen | ||
| Age | -0.082a (0.375) | -0.119 (0.197)a | -0.133a (0.149) | 0.309a (0.001) | -0.105a (-0.252) | |
| < 50 | 15 (12.5) | |||||
| 50 - 54 | 32 (26.7) | |||||
| 55 - 59 | 48 (40) | |||||
| 60 ≤ | 25 (20.8) | |||||
| Education | 0.153b (0.095) | 0.115b (0.212) | 0.139b (0.130) | -0.120b (0.193) | -0.066b (0.475) | |
| Illiterate | 15 (12.5) | |||||
| Primary | 53 (44.2) | |||||
| Diploma | 45 (37.5) | |||||
| Collegiate | 7 (5.8) | |||||
| Income | 0.026b (0.782) | -0.052b (0.573) | -0.015b (0.873) | -0.047b (0.610) | -0.046b (0.646) | |
| Low | 20 (16.7) | |||||
| Average | 90 (75) | |||||
| Good | 10 (8.3) | |||||
| Number of children | 0a (1) | -0.008a (0.929) | -0.073a (0.430) | 0.224a (0.014) | -0.087a (0.347) | |
| ≤ 2 | 29 (24.2) | |||||
| 3 | 38 (31.7) | |||||
| ≤ 4 | 53 (44.2) | |||||
| BMI | -0.001a (0.994) | 0.065a (0.481) | -0.096a (0.297) | -0.104a (0.258) | -0.081a (0.382) | |
| Diabetes (Yes) | 38 (31.7) | - (1.00c) | - (0.252c) | - (0.212c) | - (0.188c) | - (0.745) |
| Digestive disease (Yes) | 10 (8.3) | - (0.539c) | - (0.801c) | - (0.138c) | - (0.857c) | - (0.943) |
| Hypertension (Yes) | 36 (30) | - (0.272c) | - (0.535c) | - (0.470c) | - (0.989) | - (0.474) |
| Heart disease (Yes) | 25 (20.8) | - (0.051c) | - (0.297c) | - (0.470) | - (0.972c) | - (0.650) |
Distribution of Age, Education, Income, Number of Children, BMI, Diabetes, Digestive Disease, Hypertension and Heart Disease in Postmenopausal Women in Semnan (2015)
| Characteristic | Age | |||
|---|---|---|---|---|
| < 50 | 50 - 54 | 55 - 59 | 60 ≥ | |
| Depression | 10.53 (6.56) | 11.44 (7.08) | 9.33 (7.69) | 9 (6.14) |
| Stress | 22.47 (4.52) | 23.81 (4.86) | 22.19 (5.67) | 21.08 (5.71) |
| Anxiety | 87.67 (13.26) | 85.28 (17.35) | 84.33 (16.83) | 80.92 (16.88) |
| Vitamin Db | 26.07 (13.65) | 39.81 (28.18) | 41.27 (23.68) | 53.96 (36.54) |
| Estrogenb | 50.57 (52.27) | 21.76 (49.82) | 12.7 (26.82) | 12.03 (16.80) |
Mean and Standard Deviation of Indicators in Postmenopausal Women of Different Ages in Semnan (2015)a
| N (%) | Vitamin D | Estrogen | |||
|---|---|---|---|---|---|
| Mean ± SD | ra (P Value) | Mean ± SD | ra (P Value) | ||
| Depression | -0.1982 (0.031) | -0.103 (0.159) | |||
| Normal (0 - 10) | 75 (62.5) | 47.55 ± 27.77 | 21.68 ± 40.23 | ||
| Mild (11 - 16) | 27 (22.5) | 30.41 ± 25.68 | 15.09 ± 25.78 | ||
| Moderate and higher (≥ 17) | 18 (15) | 33.78 ± 26.37 | 18.42 ± 46.08 | ||
| Anxiety | -0.3636 (< 0.001) | -0.105 (0.254) | |||
| Mild (40 - 79) | 56 (46.7) | 52.61 ± 28.18 | 20.41 ± 39.77 | ||
| Moderate and higher (80 - 160) | 64 (53.3) | 31.14 ± 23.37 | 19.10 ± 37.16 | ||
| Stress | -0.2884 (0.001) | 0.104 (0.262) | |||
| Low stress (< 28) | 95 (79.2) | 44.94 ± 38.18 | 8.59 ± 6.38 | ||
| High stress (28 - 56) | 25 (20.8) | 29.04 ± 23.76 | 7.08 ± 5.57 | ||
Mean, the Standard Deviation of Vitamin D and Estrogen Scores to Separate the Different Levels of Depression, Anxiety and Stress in Postmenopausal Women Semnan (2015)
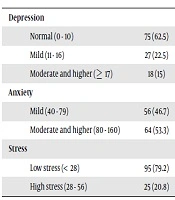
The depression levels were mild (22.5%), moderate (13.3%) and severe (1.7%); the anxiety levels were mild (46.7%), moderate (50.8%) and severe (2.5%); 79.2% had lower stress and 20.8% had higher stress (Table 3). The mean ± SD, median, interquartile range, min, and a max of depression, anxiety and stress scores, vitamin D, and estrogen in postmenopausal women in Semnan are shown in Table 4.
Mean, Standard Deviation, Median, Interquartile Range Scores of Depression, Anxiety, Stress, Vitamin D, Estrogen in Post-Menopausal Women in Semnan (2015)
There was a negative and significant correlation between depression and vitamin D (r = -0.1982, P = 0.031), but no significant correlation was found between depression and estrogen (r = -0.103, P = 0.159). A negative and significant relationship was found between vitamin D and anxiety (r = -0.3636, P < 0.001). There was no significant correlation between estrogen with anxiety (r = -0.105, P = 0.254). There was a significant negative correlation between stress and vitamin D (r = -0.2884, P = 0.001). No correlation was seen between estrogen and stress (r = -0.104, P = 0.262) (Table 4). No correlation was seen between estrogen and vitamin D (r = -0.070, P = 0.450).
5. Discussion
Our findings showed the prevalence of depression level was higher than the other studies (3). Also, there was a significant negative correlation between depression and vitamin D. In line with our study, vitamin D deficiency was related to depression (29). Some studies reported that there is no correlation between vitamin D and depression (30, 31). Vitamin D receptor (VDR) has the potential for a neuroactive effect on brain function (32) and modulates the hypothalamic-pituitary-adrenal axis, in the adrenal cortex with managing dopamine production through VDRs, noradrenaline, and adrenaline (33); and secures against the decrease of dopamine and serotonin centrally (34).
Our findings indicated there was also no significant correlation between depression and estrogen levels. The research showed that estrogen increases the availability of serotonin and has direct consequences on depression during menopause (35). Also, the findings of the study demonstrated that estrogen has either a weak or no relationship with depression (36).
The results of our study indicated the anxiety levels were higher than the other studies (37). Also, there was a negative correlation between vitamin D with anxiety. In a study, low levels of vitamin D were associated with increased anxiety (38). Alatram indicated a positive significant correlation between vitamin D deficiency and anxiety (39).
Our findings showed there was no significant correlation between estrogen and anxiety. In a study, psychological symptoms were not related to changes in estrogen levels (40). However, one report indicated the increased risk of anxiety with estrogen receptor (41).
Our results indicated there was a negative and significant relationship between stress and vitamin D. In a study, the use of multi-vitamin and mineral supplements reduced the stress (42). Premkumar et al. observed that lower vitamin D was associated with depression and stress (43).
Our findings showed there was no correlation between stress and estrogen. Hormone and age-related changes may at least partially explain why perceived stress increased during perimenopause (44) but changes in estradiol levels might increase the sensitivity to psychological stress, especially the social exclusion sensitivity, and this increased sensitivity might develop depression (45).
The findings of the present study indicated there was no correlation between estrogen and vitamin D. The hormonal alterations in women in the perimenopausal and postmenopausal periods may result in an effect on mental health. All these conditions may also be related to vitamin D deficiency (46). In the menopausal stage, there is a slow decrease in the amount of estrogen released by the ovaries (47). This decrease in estrogen release is thought to deteriorate vitamin D deficiency. The following vitamin D challenge is related to a decline in the amount of vitamin D receptors (48). Additionally, the decline in estrogen related to postmenopausal women diminishes the action of 1-alpha-hydroxylase vitamin D responsible for activating vitamin D and VDRs (49).
In this study, the diet of postmenopausal women, out-of-home activities, and exposure to sunlight were not evaluated. Also, the use of medication in postmenopausal women was not studied, which can affect the metabolism of vitamin D and estrogen. Since the willingness of postmenopausal women in Semnan to participate in the project was low due to the difficulty of referring to the laboratory, blood sampling and follow-up of the test, it is suggested further studies should be conducted with larger sample size in other countries and the relationship between the levels of vitamin D and estrogen with sleep disorders and cognitive and behavioral problems should be assessed in postmenopausal women.
5.1. Conclusions
In postmenopausal women, no significant relationship was observed between estrogen and depression, anxiety, and perceived stress, but considering the relationship between vitamin D and depression, anxiety, and stress in postmenopausal women, and increasing the amount of vitamin deficiency, screening and medical treatment for vitamin D deficiency are recommended in postmenopausal women.