1. Background
Cardiovascular diseases (CVDs) and their long-term consequences are considered as the main source of disability and mortality around the world, particularly in Iran (1, 2). CVDs are always a threat to the health of the general population as well as various clinical populations. Cancer (3), hypertension and diabetes (4, 5), and mental diseases such as anxiety and depression (6) are instances of populations vulnerable to these diseases. While there have been a plethora of studies on cardiac risk among smokers (7, 8), there is a shortage of studies on the CVDs risk among drug addicts (9, 10). Drug addiction is a chronic, progressive, and destructive illness (11), which is often accompanied by an unhealthy lifestyle in the long run (12). Nevertheless, the majority of patients and therapists mainly focus on stopping drug abuse and controlling high-risk behaviors (11). This has led to neglecting the risk of comorbidities, such as CVDs in this population.
A study shows that after controlling for all the cardiac risk factors, there is a relationship between drug abuse and coronary heart disease; drug addiction increases the risk of CVDs up to 38 times (9). According to Reece et al., cannabis is considered a cardiovascular risk factor, which accelerates the aging of the heart (10). Moreover, the results of a review study shows that high doses of methadone will potentially increase the likelihood of cardiac arrhythmia (13). Based on these findings it can be predicted that drug addicts being treated by methadone are susceptible to a level of cardiovascular risks (14), not knowing it and not perceiving its risks can have fatal consequences.
Perception of cardiac risk is an important predictor for utilizing a healthy lifestyle for preventing CVDs (15). Preventing CVDs requires risk perception and understanding the risk factors for these diseases, which can create the incentive for lifestyle modification (15). Various reports on general and clinical populations, with regards to more than three cardiac risk factors, show that people usually underestimate the risk of CVDs (16). The risk of CVDs and underestimating this risk is probably influenced by various factors such as heart knowledge among the vulnerable populations. Heart knowledge involves the ability of an individual to identify the risk factors of the disease and increasing information about cardiac health (17). Heart knowledge involves information about the epidemiology of the disease, the knowledge related to nutrition, the risk factors of the disease, the knowledge of cardiac symptoms, and medical and healthcare issues, which can significantly influence health control (17). Heart knowledge is a very important concept in the field of healthcare training (18), which has not gained a lot of attention in relation to comorbidity issues such as drug addiction. The results of previous reports on general and non-addict clinical populations show that individuals do not have satisfactory heart knowledge (16, 19) and the fact that poor heart knowledge plays a role in underestimating the risk of CVDs (19). Accordingly, Lambert et al. performed a cross-sectional study and found out that about 62% of individuals were exposed to moderate to severe risks of CVDs, which stems from their poor heart knowledge (19).
2. Objectives
The current study aims to perform a cluster analysis of heart knowledge and cardiac risk perception among substance misusers and their correlates.
3. Methods
3.1. Design and Inclusion and Exclusion Criteria
The population of this cross-sectional study includes all the patients being treated in methadone maintenance treatment (MMT) centers in the city of Kermanshah from October to December 2017. The inclusion criteria included age 18 - 70 years, ability to speak Farsi fluently, minimum of a preliminary school diploma, lack of illegal drug abuse/more than one drug before treatment, and informed consent on participating in the study. Questionnaires with more than five items left unanswered were eliminated from the study. The current study was approved by the Ethical Committee of Kermanshah University of Medical Sciences (ID: KUMS.REC.1396.57).
3.2. Participants and Data Gathering
Among more than 100 MMT clinics in the city of Kermanshah, four centers were randomly selected. Then, with regard to the gender distribution of patients, 200 participants were selected using stratified random sampling. Since the study uses cluster analysis and logistic regression analysis, the minimum size of the sample was calculated using the (N = predictive variables {9} × {8} + 50) formula (20). After applying the inclusion criteria, 27 people were dropped out due to lack of inclusion criteria and and eight people refused to participate in the study. In addition, nine individuals were excluded due to the fact that the exclusion criteria included incomplete data on questionnaires. Finally, after acquiring the written consent of the participants as well as considering the ethical principles, 156 individuals (78 percent of the total sample) were entered into the study. In order to collect data, and after a brief interview by the interviewer, samples were asked individually to fill out the questionnaire in the presence of the researcher. Filling out the scales was done in the MMT centers where they were being treated.
3.3. Instruments
3.3.1. Heart Disease Knowledge Questionnaire
This tool is a paper-based questionnaire, which was developed in 2011 by Bergman et al., and it is designed based on its previous formats (17). This questionnaire includes 30 items, which assess five areas. The subscales include nutrition (six items), epidemiology of CVDs (four items), medical issues of the disease (seven items), heart risk factors (nine items), and symptoms of cardiac attack (four items). The responses include three options of (a) true, (b) false, and (c) I don’t know. The scoring for the items is based on 0 and 1; for some items, the true option is scored and in others, the false option is scored. However, selecting option c (I don’t know) will not get a score and it will be scored as zero. Finally, the total score of each one of the subscales is calculated separately and then, the score for the entire scale is computed. The range of the total score for this questionnaire is from 0 to 30. Bergman et al., (2011) show that this scale has a significant and positive correlation with the original scale, which includes 80 items and has a weak positive correlation to the health literacy scale. Moreover, the validity of the scale was confirmed using factor analysis (17). This tool has already been used appropriately in the Iranian population (21). In the current study, Cronbach's alpha for this instrument was 0.804.
3.3.2. Perception of Risk of Heart Disease Scale
This tool is a paper-based scale developed and standardized by Ammouri and Neuberger in 2008 (15). This scale has 20 items, which measures cardiac risk perception. Perception of risk of heart disease scale (PRHDS) has three subscales, which include: dread risk (items 1, 2, 4, 5, 7, 8, and 9), risk (items 3, 11, 12, 14, 15, and 16), and unknown risk (items 6, 10, 17, 18, 19, and 20). The scoring for this scale is based on a Likert scale (completely disagree = 1 to completely agree = 4). Moreover, items 6 and 10 - 20 are scored in reverse. The total score of this scale is 20 - 80. Ammouri and Neuberger reported Cronbach’s Alpha coefficients of 0.80, 0.72, and 0.68 for subscales of dread risk, risk, and unknown risk, respectively. The correlations for the subscales in the retest method with a two-week time range were 0.76, 0.70, and 0.61, respectively. The construct validity of this tool and its correlation with the subscales of the health promotion lifestyle profile II (HPLP-II) was positive and significant (ranging from 0.20 to 0.39) (15). This tool has already been used appropriately in the Iranian population (21). In the current study, Cronbach’s alpha for this instrument was 0.880.
3.4. Data Analysis
Firstly, the cardiac risk perception was coded as poor perception (scores equal to or less than 40) or good perception (scores equal to or higher than 41). The scores for the components related to heart knowledge were entered into the analysis as the mean and standard deviation. Due to the simultaneous presence of categorical and continuous variables, two-step cluster analysis (TSCA) was performed for identifying the clusters. The fitting of the model was determined using Schwarz’s Bayesian Information Criterion (BIC) using the average silhouette coefficient. In the next step, heart knowledge and cardiac risk perception were compared between the clusters using analysis of variance (ANOVA) and chi-square. Then, the multinomial logistic analysis was carried out to identify the correlates of the derived clusters. Considering the presence of three categories, cluster 1 (participants with good risk perception) was considered as the reference cluster. All the statistical analyses were carried out using SPSS20 (IBM Corp., Armonk, NY, USA) software application. All the tests had two ranges and statistical significance was defined as P values < 0.05.
4. Results
A total of 96.2% of the participants were male and 87.8% of them were employed. 72.4%, 14.7%, and 12.9% of the participants had a history of using opioids, sedatives, stimulants, and other substances, respectively. 85.3%, 12.8%, and 1.9% of the participants were under treatment with methadone, buprenorphine, and opium tincture, respectively.
4.1. The Identified Clusters
Table 1 shows the heart knowledge and cardiac risk perception profile obtained from the two-step cluster analysis and a summary of the model. As can be seen, the silhouette measure of cohesion and separation is very good. Based on the results depicted in this table, there is a significant difference between the clusters with regards to all the components of heart knowledge and risk perception (P < 0.001). This model suggests three clusters with the following characteristics: (i) moderate knowledge with good risk perception, (ii) moderate knowledge with poor-risk perception, and (iii) poor knowledge with low cardiac risk perception. While the members of the first cluster (32.7%) had an average level of heart knowledge, they had a high cardiac risk perception. In contrast, the participants in cluster two (44.9%) had a moderate heart knowledge with poor-risk perception. The participants in the third cluster (22.4%) had poor heart knowledge and low cardiac risk perception.
| High-Risk Behaviors | Total (N = 156) | Cluster 1 (N = 51; 32.7%) | Cluster 2 (N = 70; 44.9%) | Cluster 3 (N = 35; 22.4%) | P Value |
|---|---|---|---|---|---|
| Moderate Knowledge with High Perception | Moderate Knowledge with Low Perception | Poor Knowledge with Low Perception | |||
| Heart knowledge (mean ± SD)b | |||||
| Dietary | 2.3 ± 1.4 | 2.8 ± 1.0 | 2.8 ± 1.2 | 0.5 ± 0.8 | < 0.001 |
| Epidemiology | 1.8 ± 1.0 | 2.1 ± 0.9 | 2.2 ± 0.8 | 0.8 ± 0.7 | < 0.001 |
| Medical | 2.6 ± 1.5 | 3.2 ± 1.2 | 3.1 ± 1.2 | 0.9 ± 1.0 | < 0.001 |
| Risk factors | 4.7 ± 1.7 | 4.9 ± 1.4 | 5.5 ± 1.2 | 2.7 ± 1.4 | < 0.001 |
| Symptoms | 1.8 ± 1.1 | 1.9 ± 0.9 | 2.1 ± 1.0 | 0.8 ± 0.8 | < 0.001 |
| Risk perception (%)c | < 0.001 | ||||
| Low perception | 95 (60.9) | 0 (0) | 70 (44.9) | 25 (16.0) | |
| High perception | 61 (39.1) | 51 (32.7) | 0 (0) | 10 (6.4) |
aSummary of model: Silhouette measure of cohesion and separation is 0.4; ratio of sizes for largest to the smallest cluster is 2.0; the most important predictors are: heart risk perception = 1.0, components of heart knowledge = 0.3 to 0.7.
bChi-square test
cANOVA
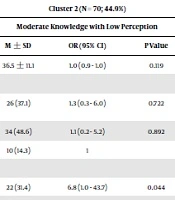
4.2. Correlates of the Clusters
Table 2 depicts the characteristics of the participants based on the clusters at the baseline. Moreover, this table presents the results of the multinomial logistic regression as well. The results show that the model is able to predict 20.3% - 39.8% of the variance in the clusters. The information in this table shows that among the demographic variables, only marital status is significantly related to at-risk clusters (P = 0.044, P = 0.014). In other words, single individuals have poorer heart knowledge and risk perception. Moreover, the history of hypertension in cluster 3 is significantly less than the reference cluster (P = 0.045), i.e. lack of hypertension history reduces heart knowledge and good cardiac risk perception up to 0.2 times.
| Predictors | Total (N = 156) | Cluster 1 (Reference) (N = 51; 32.7%) | Cluster 2 (N = 70; 44.9%) | Cluster 3 (N = 35; 22.4%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Moderate Knowledge with High Perception | Moderate Knowledge with Low Perception | Poor Knowledge with Low Perception | |||||||
| Values | OR (95% CI) | Values | OR (95% CI) | P Value | Values | OR (95% CI) | P Value | ||
| Age, y (mean ± SD) | 39.0 ± 11.9 | 45.4 ± 13.0 | 1 | 36.5 ± 11.1 | 1.0 (0.9 - 1.0) | 0.119 | 34.4 ± 7.3 | 0.9 (0.9 - 1.0) | 0.088 |
| Education, N (%) | 1 | ||||||||
| Under diploma | 68 (43.6) | 24 (47.1) | 26 (37.1) | 1.3 (0.3 - 6.0) | 0.722 | 18 (51.4) | 1.2 (1.0 - 1.4) | 0.999 | |
| Diploma | 71 (45.5) | 22 (43.1) | 34 (48.6) | 1.1 (0.2 - 5.2) | 0.892 | 15 (42.9) | 6.5 (0.7 - 60.2) | 0.477 | |
| Academic | 17 (10.9) | 5 (9.8) | 10 (14.3) | 1 | 2 (5.7) | 2.2 (0.2 -20.4) | |||
| Marital status, N (%) | 1 | ||||||||
| Single | 42 (26.9) | 3 (5.9) | 22 (31.4) | 6.8 (1.0 - 43.7) | 0.044 | 17 (48.6) | 17.7 (1.7 - 142.1) | 0.014 | |
| Married | 92 (59.0) | 36 (70.6) | 41 (58.6) | 1.5 (0.4 - 5.1) | 0.516 | 15 (42.9) | 1.2 (0.2 - 5.8) | 0.856 | |
| Widow/divorced | 22 (14.1) | 12 (23.5) | 7 (10.0) | 1 | 3 (8.6) | 1 | |||
| Smoking, N (%) | 1 | ||||||||
| Never | 29 (18.6) | 7 (13.7) | 18 (25.7) | 1.8 (0.5 - 5.7) | 0.352 | 4 (11.4) | 0.6 (0.1 - 3.2) | 0.586 | |
| Cessation | 17 (10.9) | 10 (19.6) | 5 (7.1) | 0.6 (0.1 - 2.4) | 0.457 | 2 (5.7) | 0.4 (0.1 - 2.6) | 0.321 | |
| Active | 110 (70.5) | 34 (66.7) | 47 (67.1) | 1 | 29 (82.9) | 1 | |||
| Drinking, N (%) | 1 | ||||||||
| Never | 88 (56.4) | 27 (52.9) | 40 (57.1) | 0.7 (0.2 - 2.7) | 0.628 | 21 (60.0) | 1.5 (0.2 - 9.6) | 0.640 | |
| Cessation | 45 (28.8) | 16 (31.4) | 18 (25.7) | 0.8 (0.2 - 3.1) | 0.733 | 11 (31.4) | 2.0 (0.3 - 13.0) | 0.452 | |
| Active | 23 (14.7) | 8 (15.7) | 12 (17.1) | 1 | 3 (8.6) | 1 | |||
| Heart and risk factors history, N (%) | 1 | ||||||||
| CVDs | 36 (23.1) | 21 (41.2) | 12 (17.1) | 0.6 (0.2 - 1.9) | 0.407 | 3 (8.6) | 0.5 (0.1 - 2.6) | 0.413 | |
| HTN | 93 (59.6) | 41 (80.4) | 35 (50.0) | 0.4 (0.1 - 1.2) | 0.094 | 17 (48.6) | 0.2 (0.1 - 1.0) | 0.045 | |
| DM | 45 (28.8) | 21 (41.2) | 15 (21.4) | 0.6 (0.2 - 1.6) | 0.295 | 9 (25.7) | 1.3 (0.4 - 4.5) | 0.710 | |
| HLP | 87 (55.8) | 33 (76.5) | 39 (47.1) | 0.6 (0.2 - 1.7) | 0.330 | 15 (42.9) | 0.5 (0.1 - 1.8) | 0.273 | |
Abbreviations: CVDs, cardiovascular diseases; DM, diabetes mellitus; HLP, hyperlipidemia; HTN, hypertension.
aThe socio-demographics and other factors in this table were all included as covariates in the generation of the multinomial logistic regression model. Boldface indicates a statistically significant (P < 0.05).
bSummary of model: The model fitting information is: Chi-square = 67.170, P < 0.0005; Pseudo R-square based on McFadden and Nagelkerke = 0.203 to 0.398.
5. Discussion
It is obvious that behaviors more than anything else are influenced by individuals’ thoughts, beliefs, and attitudes (22). Based on the health belief model, the health perception of individuals changes their behaviors when they feel that they are exposed to a threat or disease and when they believe that this change in the behavior is effective in controlling threat or illness (23). Good cardiac risk perception plays an important role in adopting a healthy lifestyle and preventing CVDs (15). The risk factors caused by unhealthy lifestyles is not only prevalent among the general population of Iran (24), they are also creating complications among drug addicts (12). Factors such as smoking cigarettes (25), obesity (26), hypertension (27), diabetes (28), malnutrition (29), sedentary lifestyle and lack of mobility (30), as well as stress (31) are prevalent among addicts. Considering that about two-thirds of our patients had poor cardiac risk perception, the likelihood of controlling these risk factors is weak.
None of the clusters derived from the patients in the current study had good heart knowledge. In other words, the cardiovascular knowledge level of all the participants was moderate or lower. Poor health literacy and heart knowledge among the participants along with poor cardiac risk perception show the high vulnerability of these individuals to CVDs. Zakiei et al. (32), found that cardiovascular health literacy and higher cardiac risk perception could play a significant role in controlling the risk factors of CVDs. Moreover, lower health literacy is related to all types of morbidity among cardiovascular patients (33). Vulnerable clusters with unsatisfactory heart knowledge and poor cardiac risk perception were generally of a younger age. Many of these are single adolescents who believe CVDs are the realm of the elderly and very far from their age group. Through aging and getting married, people get closer to middle age and old age; thus, they will better understand the psychological and behavioral reasons behind CVDs. This is the while the younger populations do not have a suitable attitude to CVDs and believe genetics (without any relation to controllable behaviors) are the main reason for these illnesses (1).
The results of the current study also shows that substance misusers with a personal or family history of hypertension have higher heart knowledge and risk perception. If these individuals are afflicted with chronic hypertension, they are likely to be examined routinely by a physician. The physician’s visits, instructions, and recommendations with regards to using medication, controlling the dietary regime, and adopting a healthy lifestyle can improve the level of knowledge and risk perception in these individuals. If they have a family member suffering from hypertension, accompanying their family members on visits to the doctors can improve their risk perception. Since hypertension is considered as a chronic illness and it hugely affects the functionality of the patient, as time passes, all the members of the family will acquire useful information about the diseases related to this complication. The results of a study shows that there is a relationship between the history of hypertension and understanding it as a cardiac risk factor (2). On the contrary, they do not have an appropriate understanding of other cardiac risk factors such as obesity, high blood fat, aging, and drug abuse and they will underestimate these factors significantly (2). In line with the above-mentioned report, the current study shows that histories of CVDs, hyperlipidemia, and diabetes play no significant roles in improving the heart knowledge and risk perception of the patients.
One of the limitations of the study was the unequal ratio of men and women. A total of 96% of male participants should be considered in generalizing the findings. Choosing a larger sample including more women can be an important target in future studies. Examination of the samples separately by the type of drug can also help increase the accuracy of the results in future studies.
5.1. Conclusions
Cluster analyses can appropriately partition substance misusers based on their level of heart knowledge and cardiac risk perception. The identified vulnerable groups are affected by a number of demographics and family histories of chronic diseases. The results of the current study provide useful insights for family physicians and cardiovascular health professionals.