1. Background
Lumbar disc herniation with radiculopathy (LDHR) is a common problem that affects people globally. The true incidence of symptomatic LDHR is yet to be adequately established because of the disagreement about what constitutes a typical disc herniation and inability to quantify the specific population at risk (1). In addition, the whole natural history of this disorder is also poorly described however some studies (2, 3) suggest that a significant proportion of patients with lumbar disc lesion will develop spontaneous recovery without significant therapeutic interventions.
LDHR is treated with various therapies that run the spectrum from well-constructed surgeries (4) to non-surgical care (5) and a combination of many therapies (6). Perhaps the reasons there are so many different treatment strategies for LDHR is that none of them seems to work all of the time. One of the problems inherent to treating patients with LDHR is the difficulty determining which interventions to apply to which patients. However, there are no standardized guidelines for appropriate non-operative care, which suggest that more treatment options are urgently needed to ameliorate LDHR (6).
Studies (7, 8) demonstrate that most patients with LDHR have signs of joint dysfunction at the level and on the sides of the dysfunction and thus, they have indications for manipulation at the involved level and there is overwhelming evidence (9-18) that patients with lumbar radiculopathy can be treated with manipulation without adverse reaction beyond the occasional short-term increase in pain. In spite of this, LDHR particularly in the acute stage can be very volatile with the pain easily provoked in response to spinal manipulation and some authors (11, 12, 19-21) have even gone as far as to dissuade the use of spinal manipulation in the presence of neurological symptoms due to the possible risk of increased herniation or a threat to causing cauda equina syndrome (CES) (22-25) which have been stated as the leading cause of claims against chiropractors (26). Thankfully, a systematic review and risk assessment of the literature (27) have assessed the risk of spinal manipulation leading to a symptomatic disk lesion or CES in patients presenting with LDH from the published studies to be fewer than 1 in 3.7 million which advocated the apparent safety of spinal manipulation in the management of the condition.
On the other hand, spinal mobilization may be useful in the management of LDHR as it is less likely to cause a flare-up of pain in many cases compared to spinal manipulation and many studies (19, 28-30) have reported its therapeutic efficacy. However, despite the overwhelming literature reporting the therapeutic efficacy of spinal manipulation and mobilization individually, there seems to be a scarcity of evidence that compared the efficacy of both techniques in individuals with LDHR. Therefore, the identification of groups of patients with LDHR who respond favorably to either manipulation or mobilization has been deemed a research priority. In addition, the patient’s safety and well-being should always be prioritized in any clinical setting. For these reasons, this study would like to investigate the effect of spinal manipulation compared with spinal mobilization in the management of individuals with LDHR. The major hypothesis of the study was stated as: “there will be no significant difference between spinal manipulation and spinal mobilization in pain, disability and other outcomes in the management of individuals with LDHR”.
2. Methods
2.1. Study Design and Setting
This study will be designed as a double-blind randomized clinical trial (RCT). Ethical approval to conduct this study was obtained from the Health Research Ethics Committee of Federal Medical Centre (FMC), Nguru, Yobe State, Nigeria with the following File Reference Number: FMC/N/CL.SERV/355/VOL IV/131. Trial registration was done in the Pan African Clinical Trial Registry (Registration Number: PACTR201812840142310).
2.2. Eligibility Criteria
Participants with back and leg pains who were diagnosed with sub-acute LDHR will be included in the study. Sub-acute individuals will be selected because of the belief that acute LDHR may resolve spontaneously within a few weeks of onset (2, 3). The criteria for inclusion will be; patients with an age range of 25 - 55 years having unilateral radiculopathy and pain in the distribution of the sciatic nerve. The pain will be accepted as evidence of L5 root compression when distributed to the anterolateral aspect of calf and to the dorsum of the foot and as evidence to S1 root compression when distributed to the posterior aspect of calf extending to the heel and lateral aspect of the foot. If pain did not extend below the ankle, at least one additional neurological sign will be required for the patient to be included. These signs are; painful passive knee flexion, weakness of resisted hip flexion and resisted knee extension and absence or sluggishness of knee jerk reflex for L2/L3 nerve roots, hypoesthesia in the dorsum of the foot, weakness of dorsiflexion of foot or first toe and impaired medial hamstring reflex for the L4/L5 nerve roots, hypoesthesia at the lateral aspect of the foot, weakness of the plantar flexion of the foot or first toe, impaired Achilles tendon reflex and painless weakness on resisted eversion for the L5/S1 nerve roots, gluteal mass wasting and weakness on tiptoeing on the affected leg for the S1/S2 nerve roots.
The exclusion criteria will be; subjects diagnosed with dementia or other cognitive impairment, subjects diagnosed with claudication, inflammatory or other specific disorders of spine such as ankylosing spondylitis, vertebral collapse, rheumatoid arthritis, stenosis, spondylolisthesis, osteoporosis, previous spinal surgery, a known pregnancy, bilateral radiculopathy, and presence of red flags (history of significant trauma, cancer, constitutional symptoms; fever, malaise, weight loss, recent infection, bladder and/or bowel dysfunction).
2.3. Sample Size Estimation
The sample size that will be used in this study was calculated using G*Power version 3.1. The effect size (ES) used for calculating the sample size was obtained from the previous study (31) using pain as the primary outcome. The probability level (α), the power (p) and the effect size (ES) used for the calculation were then set at 0.05, 0.95 and 1.3, respectively which yielded a sample size of 17 participants per group (total sample size was 34) using Independent t-test for between-group analysis. In addition, a 20% attrition rate was adjusted which brings the total sample size to 40.
2.4. Randomization and Concealment
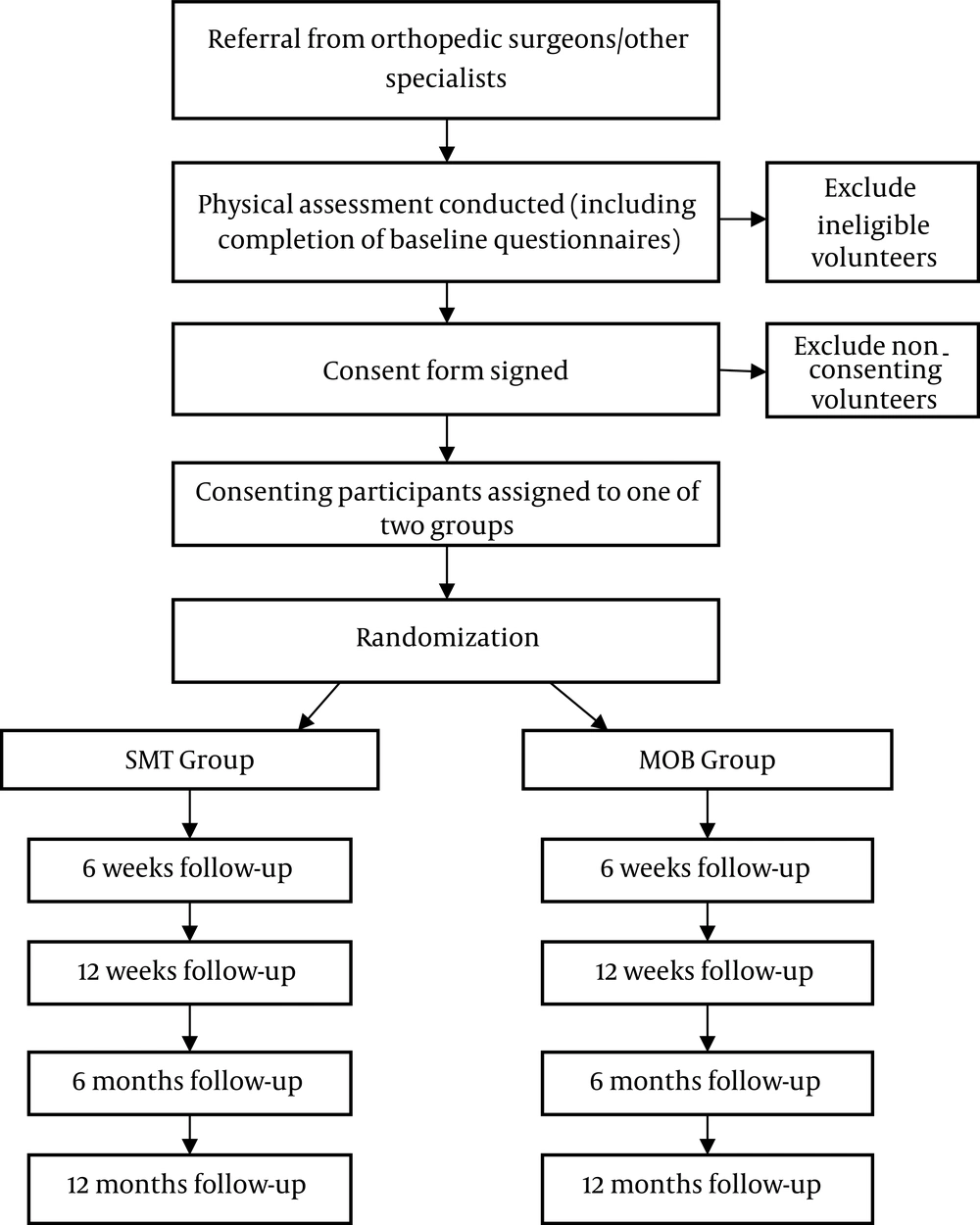
Eligible participants who provide informed consent will be randomized into one of two treatment groups; spinal manipulation or mobilization. A randomization timeline will be prepared by a research assistant who will not have communication with any participant throughout the trial and will be unaware of the recruitment, screening, assessment, enrolment or treatment process. The randomization series will be created by the use of SAS 9.4 statistical software (Cary, NC, USA) with the participants likely to be assigned to a group with an equal chance of allocation. See Figure 1 for the study flow chart.
2.5. Study Team
The study team will consist of four orthopedic physiotherapists (OPTs) and one neurologist. Two OPTs will administer the techniques independently to the two study groups. One of the remaining two OPTs will act as a research assistant while the other will work with the neurologist to screen participants for eligibility.
2.6. Intervention Procedure
There will be two intervention groups in this study. One of the groups (Group A) will receive spinal manipulative therapy (SMT) while the other group (Group B) will receive spinal mobilization (MOB). In addition, each treatment group will receive neural mobilization exercises as adjunct therapies. The full intervention protocol will be described below:
2.6.1. Group A
Participants in this group will receive the spinal manipulative therapy (SMT) protocol. The SMT will consist of high-velocity, low-amplitude manipulative technique, which is commonly employed for this type of disorder (8, 16, 28, 32). The full spinal manipulative therapy protocol requires that the patient lies on the side with the affected leg uppermost. The physiotherapist (PT) will hook the prominence of the spinous process of the inferior vertebra of the involved motion segment and then applies traction to pull out a tissue and/or joint slack. This will be aided by a downward force directed through the PT’s knee to assist in stabilizing the spine of the patient. The other hand’s middle finger of the therapist will be used to block the transverse process of the superior vertebra. Rotation will be minimized, with extension motion limited from semiflexion to neutral, just like in the previous studies (28, 32). The thrust will be delivered by the hand which is in contact with the patient’s spine and with the body drop of the therapist.
2.6.2. Group B
Participants in this group will receive spinal mobilization (MOB) using Mulligan’s (33) protocol. This technique will be performed with the participant in a side-lying position, with the affected leg uppermost. The participant will be lying facing the treating therapist, and an assistant therapist will be holding the affected leg. The treating therapist will then flex over the participant and place one thumb reinforced over the other on the prominence of the affected vertebra as palpated by taking the posterior superior iliac crest as the reference zone. The therapist will then push down on the chosen spinous process of the affected vertebra and maintain the pressure while the participant will be asked to actively perform straight leg raise (SLR) for the leg held by the assistant therapist if there is not too much discomfort. The position will be maintained for some time, after which the therapist will release the pressure on the spinous process and the participant will be asked to lower his/her supporting leg down to the couch. During first visit, three repetitions will be applied. On the subsequent visits as the participant improves, the assistant therapist will apply over-pressure on the supported leg of the participant as he/she performs the SLR. This will be also sustained for some time after which the leg will be lowered to the starting position. Six repetitions will be given on the subsequent visits.
2.7. Neural Mobilization Exercises
Neural mobilization exercises will be conducted by carrying out straight leg raise (SLR) to induce tension in the sciatic nerve. The SLR technique will be conducted as per the guidelines of Butler, and Jones (34). The participant will be in the supine position and comforted with pillows. The therapist will stand on the side to be treated, and raise the affected side perpendicular to the bed with one hand on the popliteal fossa and the other on the patella until sciatic nerve pain is provoked. The limb will then be taken down some few degrees from this painful position. The therapist will start to stretch (mobilize) the sciatic nerve by a series of oscillatory movements toward the ankle dorsiflexion and then reassess progress. To create further tension (i.e., sensitization) into the proximal segment of the affected nerve, hip adduction, and internal rotation will be added to the SLR. Many repetitions will be performed depending on the participant’s responses and tolerance. As the symptom improves, the range of motion will be increased until the maximum range of SLR is obtained (35). The position will be held for 30 seconds and a total of 5 repetitions will be conducted. Each participant will receive two sessions a week for twelve weeks.
2.8. Outcomes Assessment
2.8.1. Pain
Visual analogue scale (VAS) will be used to assess pain intensities in the leg and back. These will be done by asking the participants to complete the entire questionnaires at the beginning of the study (baseline assessment). Outcomes will also be assessed at 6 and 12 weeks, after which participants will be discharged home and placed on therapeutic exercises as a home regimen. Participants will also be followed up at 6 and 12 months post-intervention. VAS has been shown to have a high inter-observer reliability coefficient (r = 0.88) (36).
2.8.2. Disability
Functional disability will be assessed using the Rolland-Morris disability questionnaire (RMDQ). This will be done by asking the participants to complete the questionnaire at the beginning of the study (baseline assessment). Outcomes will also be assessed at 6 and 12 weeks after which participants will be discharged home and placed on therapeutic exercises as a home regimen. Participants will also be followed up at 6 and 12 months post-intervention. RMDQ has a documented high level of internal consistency reliability (Cronbach’s alpha of 0.87), test-retest reliability (ICC of 0.9) construct validity, and responsiveness to change (37).
2.8.3. Sciatica
Sciatica bothersomeness will be assessed using the sciatica bothersomeness index (SBI) and sciatica frequency will be assessed using the sciatica frequency index (SFI). These will be done by asking the participants to complete the entire questionnaires at the beginning of the study (baseline assessment). Outcomes will also be assessed at 6 and 12 weeks after which participants will be discharged home and placed on therapeutic exercises as a home regimen. These questionnaires have a high level of internal consistency reliability (Cronbach’s alpha of 0.74 for SBI and 0.70 for SFI) and test-retest reliability (ICC of 0.86 for SBI and 0.90 for SBI) (38).
2.8.4. Quality of Life
Quality of life will be assessed using the health survey (SF-36) questionnaire. This will be done by asking the participants to complete the questionnaire at the beginning of the study (baseline assessment). Outcomes will also be assessed at 6 and 12 weeks, after which participants will be discharged home and placed on therapeutic exercises as a home regimen. Participants will also be followed up at 6 and 12 months post-intervention. Extensive testing has established the psychometric properties of the SF-36. Most studies demonstrate that reliability estimates for the whole test exceed the recommended minimum value of 0.70, with figures typically over 0.80. Reliability estimates for the physical health scale and the mental health scale usually exceed 0.90 (39).
2.8.5. General Perception of Recovery
The overall perception of change of care in each participant will be assessed using the global rating of change (GROC) scale. This will be done by asking the participants to complete the questionnaire at the beginning of the study (baseline assessment). Outcomes will also be assessed at 6 and 12 weeks after which participants will be discharged home and placed on therapeutic exercises as a home regimen. Participants will also be followed up at 6 and 12 months post-intervention. This outcome scale has been used in previous studies (40-42) and has been proven reliable (ICC of 0.90) and responsive to change (43).
2.8.6. Timed Up and Go Test (TUG)
This test will be used to objectively measure the functional impairments of the participants. It will be performed with a high chair with back and armrests. Participants will begin by sitting down and leaning back in the chair. The participants will rise from the chair by using the arms for support following the command “go”. The participants will walk 3 meters in a straight line at their usual speed and then return to the chair and sit down. A stopwatch will be used to measure the time taken to complete the task. The task duration will measure up to the moment when the participants will lean back in the chair again. Outcomes will be assessed at baseline, 6 and 12 weeks, after which participants will be discharged home and placed on therapeutic exercises as a home regimen. Participants will also be followed up at 6 and 12 months post-intervention. TUG has been shown to have a high inter-observer reliability coefficient (r = 0.99) and intra-class correlation coefficient (r = 0.97) (44).
2.9. Statistical Consideration
Data obtained from this study will be analyzed using SPSS version 20.0 software (SPSS Inc., Chicago, Illinois, USA). The demographics and clinical parameters of the participants will be summarized using descriptive statistics. The normality of the data will be assessed using Shapiro-Wilk statistics. Participants’ characteristics will be compared at baseline using Independent t-test. Levene’s test will be used to assess the homogeneity of variances between groups. Repeated measures ANOVA with the intervention (SMT and MOB) as the between-subject variable and time (baseline, weeks 6 and 12, months 6 and 12) as the within-subject variable will be used to analyze treatment effects. The dependent variables to be analyzed will be the RMDQ, VAS for leg, VAS for back, SBI, SFI, SF-36, and GROC. When significant intra-group differences are detected by ANOVA, Bonferroni post-hoc analysis of variance will be used to assess differences across timelines. Two-way ANOVA with groups and timelines as independent variables (factors), will be used to measure between-group interactions and effects across timelines (weeks 6 and 12, months 6 and 12). The data will be analyzed according to the intention to treat analysis by carrying the last available score forward. Differences between the means will be considered at 5% probability level (P < 0.05) and the value of confidence interval (CI) will set at 95%.
3. Results
In this randomized clinical trial, we aim to compare the effect of spinal manipulation and spinal mobilization in individuals with LDHR. We hypothesized that participants who will receive spinal manipulation will not be significantly better than those who will receive spinal mobilization on all outcomes. We will be testing this hypothesis in participants with sub-acute LDHR. This agreement was made to prevent inclusion of participants who may resolve their symptoms spontaneously due to the natural healing of the disc which is usually in the acute phase (45).
This study will be utilizing several outcome measures to track participants’ progression throughout the study period and data will be taken at baseline, 6th and 12th weeks. Participants will be discharged home after the 12th week of intervention and then placed on therapeutic exercises as a home regimen. Outcomes will also be assessed at 6th and 12th months of follow-up.
Due to the nature of the interventions, the treating physiotherapists will not be blinded in this trial. However, therapists will be blinded to group allocation and outcomes assessment. In addition, therapists and participants will also be notified about the quality of both treatment arms and be informed that each arm has a positive influence on lumbar disc herniation and there is no existing evidence to suggest that one treatment approach is better than the other. We are determined to finish recruitment for the study by the end of 2019, with the one-year follow-up data expected to end by December 2020.