1. Introduction
Femoral neuropathy is an infrequent complication after surgeries or obstetric procedures and is most commonly reported after direct trauma (1, 2). The neurological lesion after hip surgery is one of the most horrible complications for both surgeon and patient (3).
Femoral nerve injury may be due to (1) compression, (2) stretching, (3) ischemia, (4) direct nerve trauma during hip surgery: the use of self-retractors in abdominopelvic surgery, the position of lithotomy after anesthesia or delivery, and other rare reasons, and (5) heat released by methacrylate in the cementation of the hip prosthesis (4).
The incidence of this complication after abdominal and gynecological surgery has decreased, but the absolute number of complications after hip surgery has increased in the last decade (1). An incidence of 0.08% to 7.5% has been described in primary hip arthroplasties (5) and between 2% and 7% in revision arthroplasties (6). With the aging of the population, it is expected that femoral nerve injury becomes a more common complication after total hip arthroplasties whether in primary or revision surgeries.
The femoral nerve (union of the posterior division of the ventral branches of L2, L3, and L4) runs between the psoas and iliac muscle and descends below the iliac ligament lateral to the femoral artery, in a region where the nerve can be compressed by retractors in the hip surgery (7). The clinical picture of the femoral nerve lesion is characterized by hypoesthesia and/or pain in the anterior aspect of the thigh, knee and the anteromedial portion of the leg (in mild to moderate lesions). In the most severe cases, it may be accompanied by weakness for knee extension and hip flexion (2).
Femoral nerve lesions can be classified according to clinical and histological features, in mild, moderate and severe grades. In fact, Seddon classified the severity of nerve lesions in three grades: (1) Neuroapraxia (compression of myelin sheaths), (2) Axonotmesis (lesion of axons), and (3) Neurotmesis (lesion that compromises myelin sheath, axon and the connective tissue that surrounds them). There is a good correlation between clinical symptoms and histological damage. This fact is of paramount importance because the prognosis and management depend on the severity of nerve lesions.
The objective of this article is to present the unusual complication of femoral nerve injury after the implantation of a hip prosthesis and a subsequent revision for secondary acetabular fracture and to review the clinical picture, the probable causative factors, the diagnostic confirmation tests and the therapeutic options as well as the prognosis in a special case.
2. Case Presentation
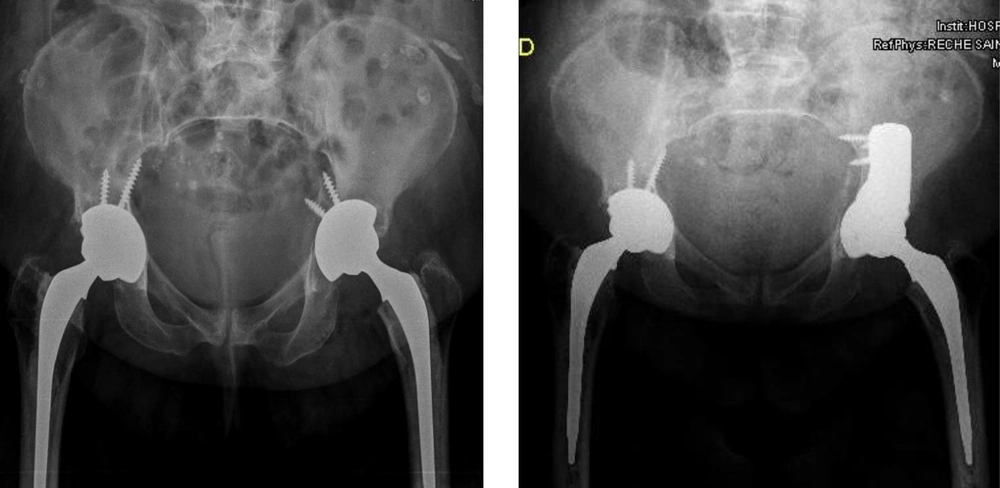
The patient, an 83-year-old woman with a baseline life history limited by arthrosis of the hip, was operated on by implanting a total hip prosthesis 2 months ago (Moore’s posterior approach and a cemented cup implant with 2 screws and a cemented femoral stem Versys). One day after the surgery, the acetabular fracture was seen in the control radiograph (Figure 1). It was decided to perform revision surgery a week after the first surgery, confirming in the operating room a comminuted fracture of the wall and back column.
In order to correct the acetabular fracture, a posterior column was placed, cemented to a 5° tantalum wedge (fixed with 4 screws to ilium), placing a tantalum-cemented multi holes cup (and fixed to the bone with a screw) and polyethylene with 20° posterosuperior brow. When reduced, motility was observed in the stem, so the stem was removed, the proximal cement of the femur was removed and again the Versys Heritage stem cementation was performed (Figure 1).
Following the revision surgery, it was decided that the patient should continue keeping the operated member unloaded for six weeks, having to perform at the moment bed-armchair and armchair-bed living.
After the 6th postoperative week, loading was authorized, but the patient was unable to stand up, presenting claudication of the left knee to the standing position. Standing, there was a lack of control of the quadriceps and recurvate of the knee. At the sitting examination, the muscle balance (MB) according to the modified Oxford Scale (graded from 0 to 5), was as follows: psoas iliac 2/5, gluteus medium 1/5, quadriceps 0 - 1/5, tibialis anterior 2 - 3/5, extensor common fingers 3/5, long extensor of 1st finger 3/5. Examination of sensitivity revealed hypoesthesia in the anterior aspect of the thigh. The patellar reflex was not evoked (it was abolished). Suspecting probable lesion of the femoral nerve, electromyogram/electroneurogram (EMG/ENG) and Lumbar Tomography were requested and Rehabilitation was prescribed awaiting confirmation of the diagnosis (neuropathy, plexopathy or radiculopathy), typing of the severity and kind of injury (neuropraxia, axonotmesis or neurotmesis).
The aim of the rehabilitation protocol was to reduce pain and to improve the functionality of the patient. The patient was prescribed to stand with the support of the bed’s bar. As postural control improves, orthotics would be placed for extension of the knee. We insist that the patient should perform exercises in decubitus or a sitting position (for 10 minutes) of both lower limbs (active ankles and counter-resistance exercises, isometrics of quadriceps and gluteus muscles, trunk control and transfers). In addition, quadriceps electrostimulation was prescribed during isometric exercises (30 minutes once a day).
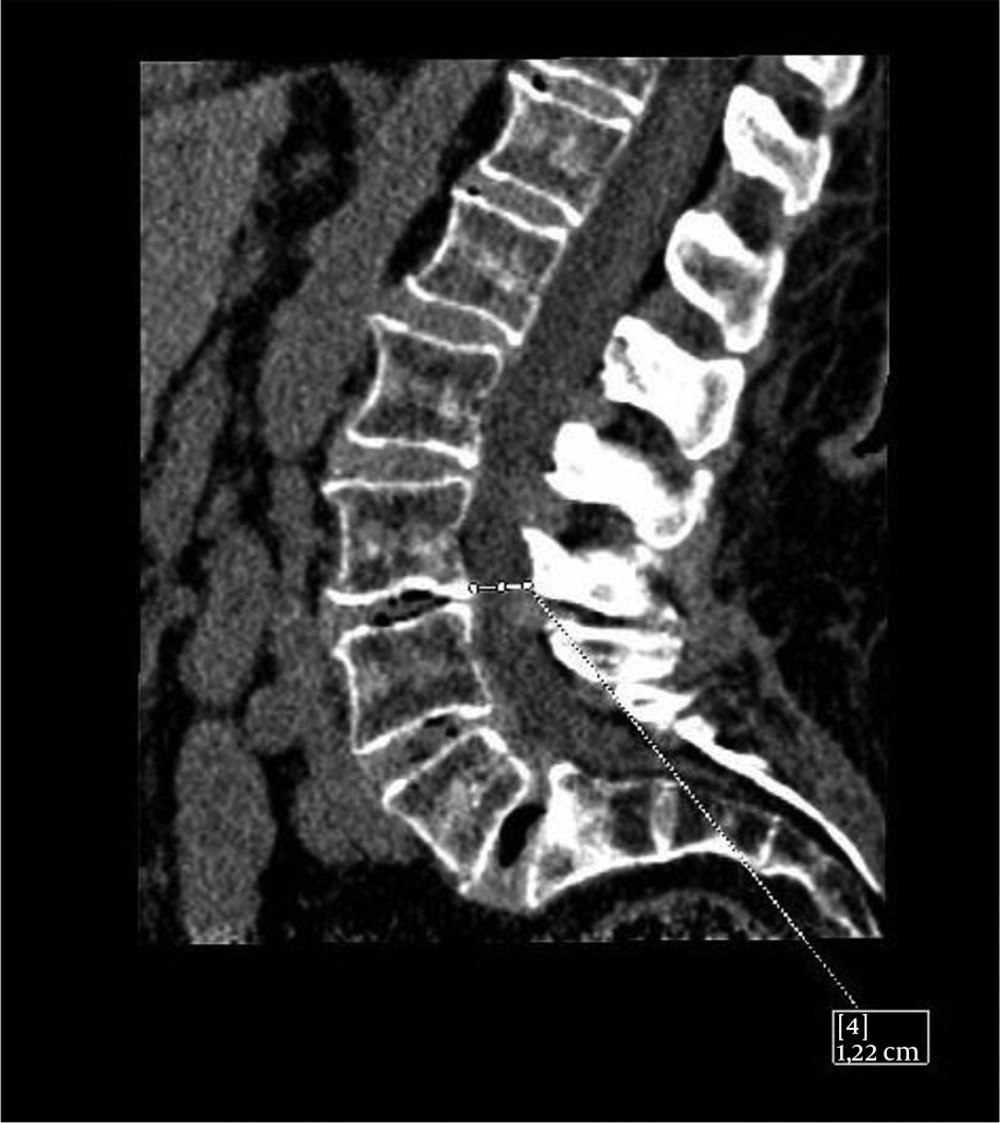
Lumbar tomography was performed, which revealed diffuse degenerative bony disc changes from L3 to S1 (third lumbar to first sacral vertebrae), ruling out radicular involvement at these levels (Figure 2).
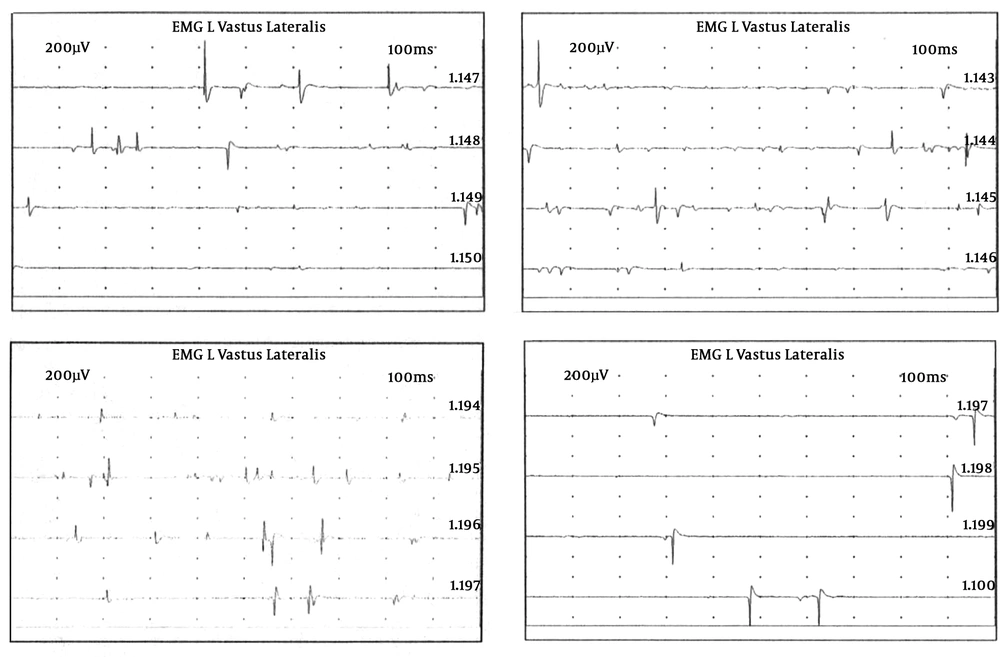
The EMG/ENG was performed 8 weeks postoperatively. The EMG study revealed abundant signs of active denervation (fibrillations and positive waves) with some nascent reinnervation potential in left vastus lateralis muscle (femoral nerve-dependent muscle) (Figure 3). Signs of active denervation and chronic reinnervation were seen in the tibialis anterior, extensor digitorum brevis, and bilateral gastrocnemius muscles, however, they were more predominant on the left side such as paraspinal musculature. There was some polyphasic muscle potential in the left anterior tibial muscle. In the right vastus lateral muscle, there were denervation signs and reinnervation signs to a lesser degree. The ENG revealed that the nerve conduction study of right peroneus common nerve and right posterior tibial nerve presented normal morphology, amplitude and distal latency (Table 1). The same nerves on the left side were prolonged, with sparse morphology, reduced amplitude, prolonged distal latency and slow MCV (motor conduction velocity) (Table 2). There was an absence of late F-response on the left side compatible with radicular or more proximal nerve involvement (plexopathy). The latency of the left H-reflex showed prolonged latency. The superficial peroneal nerve and left sural nerve had scattered morphology, reduced amplitude and SCV (sensory conduction velocity) slightly slowed. The left saphenous nerve was absent (continuation of the femoral nerve).
| Nerve/Sites | Rec. Site | Onset Lat, ms | Peak Lat, ms | NP Amp, µV | PP Amp, µV | Segment | Distance, mm | Peak Diff, ms | Velocity, m/s |
|---|---|---|---|---|---|---|---|---|---|
| R Sural-Ankle (Calf) | |||||||||
| 1 | Ankle | 1.56 | 2.34 | 6.9 | 6.1 | 1-Ankle | 75 | 48 | |
| L Sural-Ankle (Calf) | |||||||||
| 1 | Ankle | 1.77 | 2.34 | 1.5 | 4.1↓ | 1-Ankle | 70 | 40↓ | |
| R Superficial peroneal-Ankle | |||||||||
| 1 | Ankle | 3.23 | 5.47 | 4.3 | 6.1 | 1-Ankle | 150 | 46 | |
| L Superficial peroneal-Ankle | |||||||||
| 1 | Ankle | 3.13 | 4.90 | 3.0 | 4.0↓ | 1-Ankle | 135 | 43 ↓ | |
| 2 | Ankle | 3.13 | 4.69 | 1.6 | 4.0 | 2 - 1 | -0,21 |
Abbreviations: Amp, amplitude; Diff, difference; Lat, latency; L, left; m/s, meters/second; ms, milliseconds; Rec, recording; PP, peak to peak; R, right; µV, microvolts.
| Nerve/Sites | Muscle | Latency, ms | Amplitude, mV | Rel Amp, % | Duration, ms | Segments | Distance, mm | Lat Diff, ms | Velocity, m/s |
|---|---|---|---|---|---|---|---|---|---|
| L Peroneal-EDB | |||||||||
| Ankle | EDB | 5.83 | 0.4↓ | 100 | 3.70 | Ankle-EDB | 70 | ||
| Pop fossa-Ankle | |||||||||
| R Peroneal-EDB | |||||||||
| Ankle | EDB | 5.89 | 3.4 | 100 | 2.97 | Ankle-EDB | 75 | ||
| Fib head | EDB | 13.07 | 2.5 | 73.7 | 4.69 | Fib head-Ankle | 335 | 7.19 | 47 |
| Pop fossa-Ankle | |||||||||
| L Tibial-AH | |||||||||
| Ankle | AH | 5.00 | 0.7↓ | 100 | 4.90 | Ankle-AH | 95 | ||
| Pop fossa | AH | 12.92 | 0.0 | 4.18 | 11.93 | Pop fossa-Ankle | 310 | 7.92 | 39 |
| R Tibial-AH | |||||||||
| Ankle | AH | 4.48 | 3.0 | 100 | 7.29 | Ankle-AH | 95 | ||
| Pop fossa | AH | 12.19 | 0.1 | 2.6 | 15.00 | Pop fossa-Ankle | 330 | 7.71 | 43 |
| R Tibial-AH | |||||||||
| Ankle | AH | 4.43 | 3.2 | 100 | 7.55 | Ankle-AH |
Abbreviations: Amp, amplitude; AH, abductor halluces; Diff, difference; EDB, extensor digitorum brevis; Fib, fibular, Pop, popliteal; L, left; mm: millimeters; , ms, milliseconds; mV, millivolts; m/s, meters/second; R, right.
The clinical judgment after EMG/ENG was: (1) incomplete axonotmesis of the left femoral nerve, of severe intensity, with very isolated nascent reinnervation potentials; (2) signs of chronic injury in muscles dependent on L4 roots and mostly bilateral L5-S1. Signs of active denervation were seen in L4, L5, and S1 roots, with a left predominance; (3) the decrease in amplitude of posterior tibial nerve, left common peroneus nerve, in addition to left polyphasic regenerative potential seen in left anterior tibial muscle with a diminution of speed makes possible suspicion of associated sciatic nerve injury.
With this diagnosis, it was decided to reinforce rehabilitation treatment in the afternoon adding: (a) quadriceps electrostimulation (triangular currents 9.8 mA, 300 - 1000 ms × 10 minutes + exponential currents 4.7 mA × 10 minutes) + Isometrics exercises of quadriceps, (b) standing and walking in the parallels with the use of orthotics blocked in the knee extension, (c) Active contraction of medium and larger gluteus muscles on stretcher and standing, psoas and lumbar extensors enhancement, (d) Lumbar electromagnetic fields therapy (20 Hertz, 30 Gauss, 20 - 30 minutes).
At 10 weeks post-surgery, the patient was transferred to a half-stay hospital to continue the rehabilitation without improvement in the muscular balance of the affected muscles (psoas and quadriceps), which is explained by the severity of the injury (incomplete but severe axonotmesis of the femoral nerve and probable associated sciatic nerve injury). However, the functionality for walking improved with the use of knee extension orthotics.
3. Discussion
In this clinical case, we report the infrequent femoral nerve injury as a complication after primary hip prosthesis surgery and revision surgery secondary to acetabular fracture with a probable associated sciatic nerve injury.
Femoral nerve injuries are mostly secondary to previous surgeries at the abdominal, pelvic, and recently after orthopedic surgery (7). The nerve can also be injured by an analgesic femoral blockage by puncture of the femoral artery (7). The mechanisms of injury may be due to nerve section, compression and ischemia, secondary to nerve retraction during these interventions (direct trauma, stretching or compression) (7). A more rare etiology would be pharmacological, which is psoas hematoma secondary to anticoagulant or anti-aggregate treatment (1, 8).
The femoral nerve is a mixed nerve that originates from the fusion of the posterior divisions of the ventral branches of L2-L3-L4, which meet in the thickness of the psoas muscle forming the longest branch of the lumbar plexus. The nerve exits the psoas externally, runs distally between it and the iliac muscle, and descends below the inguinal ligament, lateral to the femoral artery, to enter the thigh. At 4 cm distally to the inguinal ligament, it provides anterior and posterior division. The anterior division gives a motor branch for the Sartorius muscle (flexor and abductor thigh) and a sensitive branch, the anterior femoral cutaneous nerve, which innervates the skin of the anterior and medial aspect of the thigh. The posterior division of the crural nerve is divided into the saphenous nerve (which innervates the medial aspect of the knee and leg and the plantar arch of the foot) and into motor branches that innervate the following muscles: pectinate muscle (adductor, flexor and thigh abductor), and quadriceps (extensor of the leg) (7).
In the specific case of lesions of the femoral nerve associated with hip arthroplasties, the following factors are described as causal factors: (a) elongation of the operated limb (5), (b) local hematoma (8), (c) dislocation of the components (9), (d) lateral displacement of the femur in relation to the pelvis (10), and (e) direct trauma (3). It has been described that the methacrylate heat that is applied during the cementing of the hip prosthesis could act as a physical factor capable of injuring the femoral nerve (4). Buttaro et al. have reported that the most common cause of femoral nerve injury in primary arthroplasties is the compression by the acetabular “C” retractor, while the most likely cause is direct trauma in revision surgeries (3). They also indicated that the risk of neurological injury in revision surgery is three times more frequent than in the case of a primary arthroplasty (3). In fact, Gruson says that surgical management of acetabular fractures can be a cause of femoral nerve injury (11).
In our clinical case, the patient presented primary surgery and revision surgery secondary to acetabular fracture, with a period between both surgeries of only one week, which increases the risk of presenting the neurological lesion. The clinical picture of the femoral nerve injury includes (a) pain in the inguinal region that partially improves with flexion and external rotation of the hip, (b) dysesthesia in the anterior thigh and anteromedial leg, and (c) difficulty walking with bowing of the leg and/or subjective block of the knee (2). Our clinical case revealed dysesthesia in the anterior thigh and difficulty in standing and walking.
Clinical examination of a femoral lesion characteristically reveals (a) weakness to extend the knee, (b) absence of a patellar reflex and (c) sensory deficit in the thigh (2). It is noteworthy that all these signs were observed in our patient. If a neurological lesion is suspected, the case should be documented, the respective diagnostic tests should be requested (imaging tests, neurophysiological tests) and the respective assessment by Neurology, Neurophysiology or Rehabilitation should be requested to confirm the diagnosis, rule out other causes and early initiation of treatment (3).
For the definitive diagnosis, electroconductive studies (EMG/ENG) are required, not only to confirm the diagnosis, but also to determine the extension of the lesion, the severity of the same, and establish the prognosis and the possibility of recovery (2). The saphenous nerve conduction record (continuation of the femoral nerve) should be performed. The paraspinal, iliopsoas (L2 and L3) and the adductor muscles (innervated by the obturator nerve) should be assessed by EMG in order to rule out a radicular lesion, plexus lesion or peripheral nerve injury. EMG with a needle will probably be the most relevant study in the neurophysiological study, determining whether there is active or chronic denervation and if there are reinnervation potentials, which will give information on both the severity (axonal injury) and the prognosis (axonal recovery) (2). In the lesion of the femoral nerve, an electrodiagnostic study (ENG/EMG) will allow determining the location of the lesion, which cannot be determined only based on clinical signs; and to evaluate the degree of axonal loss which is essential to establish the prognosis (1).
Seddon classified the lesions into three degrees of severity: (1) Neuroapraxia, which is a blockage of anatomically intact nerve conduction caused by a minor injury; after a period of loss of sensibility recovery is completed. (2) Axonotmesis is a more severe injury in which the axons are injured, but the surrounding connective tissue is undamaged. Secondarily, Wallerian degeneration occurs that is the disintegration of the axon and myelin distal to the injured site. The preservation of the endoneurium will allow regeneration of axonal sprouts at a speed of 1mm/day, and the degree of subsequent recovery is variable. (3) Neurotmesis is the lesion of the myelin sheath, the axon and the surrounding connective tissue (complete section of the nerve), which leads to failed efforts of regeneration and presents the worst prognosis in the face of recovery (1).
DeHart and Riley have established that the incidence of femoral nerve paralysis after hip arthroplasty is very low, between 0.04% to 0.4%, and is more frequent when the acetabular retractor is placed after anterolateral approach (4). Moreover, Simmons et al. have reported that femoral nerve paralysis in hip arthroplasties may reach 2%; however, most patients present complete recovery at 12 months (12). Sunderland et al. has reported up to 2% of transient neurological injuries, but 0.5% may have permanent neurological damage after a primary hip prosthesis (13). Al-Ajmi et al. have reported that the risk of nerve injury due to an anterior approach after hip arthroplasty is very rare, meanwhile riskier than the posterior approach (1). However, lesions of the femoral nerve after hip arthroplasty are always severe (9, 14, 15). In fact, clinical experience suggests that the motor weakness that persists two months after surgery is unlikely to be completely resolved, and if it persists at 6 months, the lesion may be permanent (1). In our clinical case, the axonal injury was incomplete and severe 2 months after the injury, which indicates the severity of the case, and suggests that the prognosis is not favorable with the possibility of remaining the lesion permanently.
The treatment of a femoral nerve injury should be conservative and started as early as possible (2). The objectives of rehabilitative treatment consist of (a) early stimulation of the denervated muscle, (b) the use of knee orthotics in the extension to avoid delaying functional recovery (walking with aids), and (c) the use of tricyclic antidepressants to reduce initial dysesthesia (3). The use of a knee brace locked in extension will allow preventing instability and will favor walking (2). Acceptable recovery of up to 70% of patients after femoral neuropathy up to one year of injury has been reported; however, in patients with severe axonal injury, the degree of recovery may be incomplete or injury may persist permanently (2). In our clinical case, since the diagnosis (8 postoperative weeks), orthotics of the knee in extension, electrostimulation of the quadriceps and active exercises of the lower limb were prescribed, in physiotherapy sessions morning and afternoon. However, after three months of treatment (12 weeks post-surgery), the patient persisted with complete quadriceps paralysis (MB 0/5).
3.1. Conclusions
Femoral nerve injury is a rare complication that occurs in 1% - 2% of patients after primary hip arthroplasty and up to 2% - 7% in revision arthroplasties. Lesion mechanisms may include compression, ischemia, direct injury, traction and heat by methacrylate (cement) on the femoral nerve. The confirmatory diagnosis includes the EMG/ENG study, which allows not only to locate the lesion but also to typify the lesion (axonal, demyelinating), its severity and establish the prognosis. The treatment must be early, in order to promote functional recovery and reduce pain. The prognosis depends on the type of injury, nevertheless, most patients achieve complete recovery.