1. Context
Lumbar disc herniation (LDH) is a common condition that frequently affects the spine in young and middle-aged individuals (1). This condition is usually treated when the disc material compresses the thecal sac or lumbar nerve roots (2). The pain that comes from LDH occurs due to a combination of some factors including nerve root ischemia and inflammation resulting from local pressure and degeneration of the disc material (3), which subsequently leads to lower limb radiculopathy (4).
Lumbar disc herniation with radiculopathy (LDHR) is treated using various therapies including surgical management (5), nonsurgical management (6), and a combination of many therapies (7). The possible reason for the existence of many different treatment strategies for the management of LDHR is that none of them seems to work all the time. One of the problems inherent in treating patients with LDHR is the difficulty in determining which intervention applies to which patients (8). However, during the last few decades, the paradigm regarding the best non-operative treatment to treat LDHR has shifted between spinal manipulation (9-17) and mobilization (18-25).
Even though there are a few recent systematic reviews (26, 27) that have examined the effects of spinal manipulation and mobilization, these reviews were largely conducted on participants with non-specific low-back (26, 27) and neck pains (27). Non-specific low-back or neck pain is quite unique and different from LDHR because the former is defined as the pain not attributable to a recognizable or known specific pathology (28) while the latter is defined as the localized displacement of disc material beyond the limits of the intervertebral disc space resulting in pain, weakness, or numbness in a myotome or dermatome distribution (29). Based on these definitions, it is very clear that the etiology of the pain in non-specific low-back or neck pain is often unknown and not categorized with a major pathogenic etiology, which is in contrast to LDHR.
Although a systematic review by Leininger et al. (30) collated the published evidence on the effects of spinal manipulation or mobilization for lumbar radiculopathy, the study failed to pool outcomes or identify who benefits more from spinal manipulation and who from mobilization. There are two potential explanations for the failure of the Leininger et al. review to identify this difference in treatment effect, including the poor reporting of data and the clinical heterogeneity of the included trials and their respective participants.
In addition, it has also been suggested that the median duration of survival time of a systematic review is 5.5 years, with almost one-quarter (23%) of the included studies being out of date in the first two years of publication (31). There has been a considerable growth in evidence-based practice since 2011, with an additional number of new trials being published. Therefore, a new study is highly warranted to gather the current evidence regarding the management of LDHR using spinal manipulation and/or mobilization. The objective of the current systematic review is to compare and summarize the current evidence regarding the effectiveness of spinal manipulation and/or mobilization for patients with radiculopathy due to lumbar disc herniation and if appropriate to identify who benefits more from manipulation and who from mobilization.
2. Methods
2.1. Data Sources
An electronic database search of titles and abstracts of articles published in English will be conducted in the following databases: PEDro (physiotherapy evidence database), CINAHL (cumulative index to nursing and allied health literature), PubMed, Science Direct, Google Scholar, and The Cochrane Library. The specific search strategies will depend on the particular database being searched. The MeSH criteria for PubMed and Cochrane database search strategies will be used. In PEDro, a simple search will be conducted, combining search terms separately. In CINAHL, Google Scholar, and Science Direct, all search terms will be combined. The keywords and search strategies used for the PubMed database are illustrated in Table 1. The reference lists of the included articles will also be manually searched. This review has been registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD42019131292). Any change regarding the review will be updated in the PROSPERO database.
| No. | Search Terms |
|---|---|
| 1 | Spinal manipulation or high-velocity manipulative thrust or high-velocity low-amplitude manipulative thrust |
| 2 | Spinal mobilization or spinal apophyseal glides or spinal oscillations |
| 3 | Lumbar disc herniation or lumbar disc disease or lumbar disc lesion or lumbar disc proplapse or discogenic lumbar disc |
| 4 | 1, 2, and 3 |
2.2. Eligibility Criteria
Studies will be included if they meet the following criteria: (1) investigating male and/or female participants diagnosed with lumbar disc herniation of any duration, (2) recruiting participants with the age of 18 or above, (3) using spinal manipulation and/or mobilization of the spine as the primary therapy in at least one intervention group or in combination with other active treatments, (4) reporting an acceptable comparison group including no treatment, placebo, and any other type of active intervention, (5) evaluating outcome(s) including at least one of the main clinically relevant outcome measures for lumbar disc herniation (i.e., pain, functional ability, global perceived effect, sciatica frequency, sciatica bothersomeness, return to work, absenteeism, or recovery) using a valid instrument, and (6) randomized controlled or clinical trials (RCTs) published in English. Studies not performing between-group analyses for the measured outcomes will be excluded from the review.
2.3. Study Selection
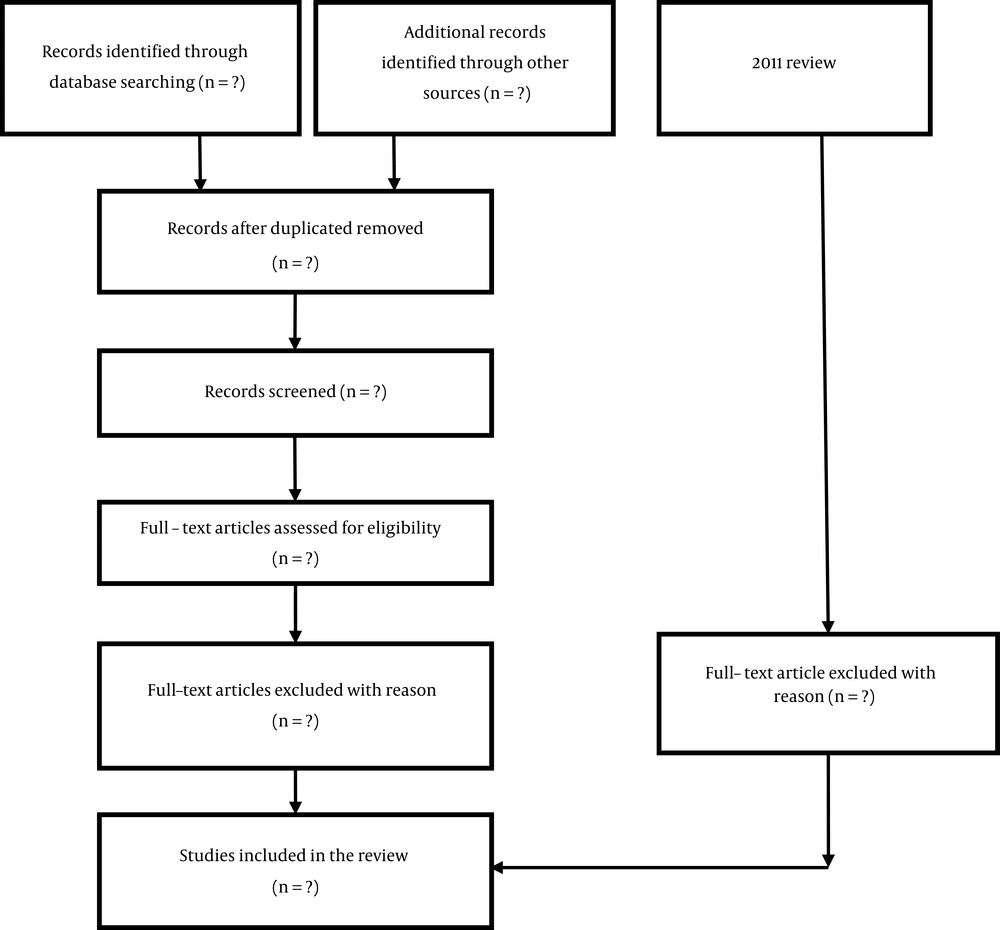
Two independent reviewers will conduct the electronic database searches and screen the titles and abstracts of the retrieved studies (see Figure 1 for the review flow chart). After the removal of duplication records, full copies of potential eligible papers will be retrieved and screened by the two reviewers. The percentage of agreement between the reviewers will be assessed using Cohen’s kappa (κ) statistic method (32). Disagreements will be resolved by consensus with a third reviewer if applicable.
2.4. Data Extraction
Data to be extracted from the studies include study design, sample size, sex, age, participants, interventions, outcomes, and follow-up. In addition, the information will also be retrieved directly from previous systematic reviews conducted in the field of spinal manipulation and mobilization (26, 27, 30). Data will be extracted by two independent reviewers and will be cross-checked by other co-authors so that any disagreements will be resolved by consensus.
2.5. Methodological Quality Assessment
The methodological quality of the included studies will be reported in a table. The rating of trials on methodological quality (internal validity) will be carried out using the PEDro scale (supplementary file Appendix 1) (33). The scale was developed by Verhagen et al. (34) using the Delphi consensus technique to develop a list of criteria thought by the experts in the field to measure the methodological quality. The scoring of the PEDro scale depends on the number of items in the scale and the design of the included studies. Items 2 - 9 refer to the internal validity of studies and items 10 and 11 refer to the statistical analysis, ensuring sufficient data to enable appropriate interpretation of the results. Item one is related to the external validity of the included studies and thus, it will not be included in the total PEDro scores (35). Studies scoring ≥ 6 out of 10 will be considered as high-quality, while studies scoring ≤ 6 out of 10 will be considered as low-quality (36). The external validity of the included studies will be assessed using the external validity assessment tool (EVAT) (37). This tool measures the generalizability of studies to other individuals (external validity) and settings (model validity) outside the scope of a study.
2.6. Risk of Bias Assessment
The risk of bias will be assessed using the Cochrane risk of bias assessment tool (38). The tool uses five different items (selection bias, performance bias, detection bias, attrition bias, and reporting bias) to determine the quality of the included studies. The tool items will be rated on a three-point scale to assess the risk of bias (0 = high-risk, 1 = unclear risk, 2 = low-risk). The tool has a maximum score of 16 points and lower scores indicate a higher risk of bias.
2.7. Clinical Relevance
The clinical relevance of the included studies will be independently assessed by two reviewers using the five-criteria recommended by the Cochrane Back Review Group (supplementary file Appendix 2) (39). In addition, the authors will also extend the third criterion to require a paper to comment on the reliability and validity of the outcome measures used in their studies because reporting on such properties is recommended in the revised CONSORT statement (40).
2.8. Statistical Analysis
The included studies will be categorized under separate comparisons with clinically homogeneous characteristics. A priori list of items will be used for data extraction. Both descriptive data and quantitative data will be extracted regarding the primary and secondary outcome measures. With sufficient clinically and statistically homogeneous and comparable reported outcomes, data will be pooled with the aid of RevMan-5 software and a random or fixed-effects model will be used in the analysis (39). Between-study statistical heterogeneity will be assessed with the I2 statistic and this review will consider ≤ 25% as low, ≤ 50% as moderate, and ≥ 75% as high heterogeneity (41). To identify publication bias, funnel plots will be examined (42).
2.9. Sensitivity Analysis
The reliability of our results will be tested using sensitivity analysis (39). We have planned to assess the impact of using high-quality studies with low, medium, and high-quality combined studies.
3. Data Synthesis
Data synthesis will be performed to pool studies for inclusion into the meta-analysis. Meta-analysis in this study will be conducted in two parts. The first part will consist of studies that compared spinal manipulation with other interventions and the second part will consist of studies that compared spinal mobilization with other interventions. The criteria that will inform about the study choice for inclusion in the meta-analysis will be clinical homogeneity in the study population, study design, outcome measure, and duration. Any study that did not meet the clinical homogeneity criteria will not be considered for inclusion in the meta-analysis. In the case in which the meta-analysis is not feasible, the best evidence synthesis will be conducted using low-risk-of-bias studies. The overall quality of the evidence will be graded as high, moderate, low, or very low, according to the GRADE approach by Furlan et al. (39).
Statistical heterogeneity among included studies will be assessed using the index of variability, chi-square test (I2). If the I2 is ≤ 25%, studies will be considered homogeneous and the fixed-effects model will be used for the meta-analysis. If the I2 is ≥ 75%, studies will be considered highly heterogeneous and the random-effects model will be used for the meta-analysis (43). In addition, if all the included studies measured the same outcome and used the same measurement scale, the mean difference (MD) would be used to determine the effect measure. Furthermore, if all the included studies measured the same outcome but did not use the same measurement scale, the effect measure would be determined by two options. The first option is to convert the data so that all data are on the same scale. However, if this is not possible, then the standardized mean difference (SMD) will be used. The SMD is the MD standardized (adjusted) by the units of the standard deviation. There are many standardized effect measures but this systematic review will use Hedge’s g, which includes an adjustment for small sample bias and is used by default in the RevMan software (44).
4. Conclusions
This systematic review will investigate and give an overview of the current evidence on the effects of spinal manipulation or spinal mobilization in comparison with other interventions in the management of individuals with LDHR. A meta-analysis will also be conducted where appropriate in this review to compare the effects of spinal manipulation or mobilization and other interventions to find out which technique is better in the management of LDHR. In addition, studies conducting a neck-to-neck comparison of spinal manipulation with mobilization will be examined to determine which of the techniques is better in the management of LDHR. Furthermore, methodological limitations of the current review and that of the included trials will be reported to give recommendations for future research.