1. Background
Hypovolemic shock, defined as a decrease in circulating blood volume, is the most common type of shock (1) and a life-threatening condition (2) if not promptly treated. It is categorized into two forms: Hemorrhagic and non-hemorrhagic shock (3). Hemorrhagic hypovolemic shock is characterized by an acute reduction in intravascular volume due to bleeding, whereas non-hemorrhagic hypovolemic shock results from a reduction in effective intravascular fluid due to fluid loss from sources such as the gastrointestinal tract, kidneys, skin, or third-space sequestration (4, 5). Hemorrhagic hypovolemia is the predominant form of shock, with traumatic events being the most frequent cause of hemorrhage (6). The pathophysiology of hypovolemic shock involves the depletion of intravascular volume (7). Hemorrhagic shock is classified into four categories based on signs and symptoms:
(1) Class I hemorrhage (less than 15% of total blood volume): In this phase, compensation is adequate to maintain central blood volume and preserve blood flow to vital organs, along with systemic metabolic acidosis and activation of humoral and cellular elements in major under-perfused organs. Signs and symptoms include normal urine output, alert consciousness, a normal respiratory rate, mild increase in pulse rate, relatively cold and pale extremities, and normal blood pressure. Blood and fluid replacement are generally unnecessary.
(2) Class II hemorrhage (15% - 30% of total blood volume loss): Characterized by tachycardia, tachypnea, reduced urine output, an anxious level of consciousness, decreased pulse pressure, cold and sweaty peripheries, and delayed capillary refill. Diastolic blood pressure may rise slightly with minimal changes in systolic pressure. Most cases require stabilization with crystalloid solutions.
(3) Class III hemorrhage (31% - 40% of total blood volume loss): Typically presents with marked tachycardia, tachypnea, a drowsy level of consciousness, reduced urine output, and marked hypotension. Immediate intervention with packed RBCs, blood products, and fluids is necessary to reverse shock.
(4) Severe shock or class IV hemorrhage (more than 40% of blood volume loss): This is an immediate life-threatening event characterized by significant tachycardia, a marked reduction in systolic blood pressure, unmeasurable diastolic blood pressure resulting in narrow pulse pressure, negligible urine output, and a depressed mental state. Patients in this class require rapid transfusion and immediate surgical intervention (8-11).
The prognosis of hemorrhagic shock depends on factors like injury severity, time to receive treatment, and injury location (11). Head injuries are commonly encountered in emergency departments and can vary in presentation, including scalp lacerations, skull fractures, and other forms of intracranial hemorrhage (12). Although these types of head injuries are unlikely to cause hemorrhagic shock due to the limited space within the skull, scalp lacerations are an exception due to the scalp’s rich blood supply and superficial location. Uncontrolled scalp bleeding may lead to hemorrhagic shock if not properly managed (13).
There is a correlation between crowded events and trauma with hemorrhage; as crowd density increases, so does the risk of trauma (14). One of the most significant and crowded events is the 10th of Muharram (Ashura) in Iraq, a day of religious rituals commemorating the martyrdom of Al-Hussain bin Ali (peace be upon him), his family, companions, and near relatives. One ritual, Tatbir, involves creating a superficial laceration on the scalp using a sword or cleaver (15, 16). Proper management of Tatbir-associated head injuries includes assessing airways, breathing, and circulation, controlling bleeding, and resuscitating with fluids and blood according to hemorrhage classification. Other essential measures include wound sterilization, suturing, and administering anti-tetanus serum and antibiotics.
The Ashura gathering has been growing annually, with increasing numbers participating in Tatbir, which raises health-related issues and the need for logistical planning, including adequately stocked blood banks. This study aims to assess any association between Tatbir-related head injuries and hemorrhagic shock or blood transfusion. To the author’s knowledge, Tatbir-related head injuries have minimal representation in the literature except for one article examining their neurosurgical aspects, which reported two main injury categories: Scalp wounds (84%) and skull fractures (14%). Patients were treated in the emergency department, and a few were admitted, primarily due to skull fractures. Follow-up data is limited (17).
2. Methods
This cross-sectional study was conducted at Imamein Kadhimain Medical City in Baghdad on July 29, 2023, corresponding to the 10th of Muharram, 1445 Hijri. Fifty patients who presented to the emergency department after practicing Tatbir were sampled, along with 50 patients with scalp wounds from other causes, sourced from hospital records from the last three months. These other causes included falls from height, road traffic accidents, and trauma from other materials. Inclusion criteria encompassed all patients who practiced Tatbir and patients with scalp wounds due to other causes. Exclusion criteria included refusal to provide information or participate in the study, and patients with non-hemorrhagic shock. Ethical approval was obtained through verbal consent from patients or their relatives. Data were collected using a pre-designed form applied to all patients in the emergency department. Patients were questioned about the method of sword sterilization and whether the same sword was used on multiple individuals. Patients were assessed in the emergency department according to the ATLS protocol and evaluated for the presence and classification of hemorrhagic shock. In this study, patients with class II hemorrhage and above were considered to have hemorrhagic shock. The management protocol for each patient was recorded, and those who required blood transfusions were noted. Statistical analysis was conducted using Microsoft Excel, and the chi-square test was used to assess any associations.
3. Results
This study presents the number and percentage of patients who used sterilized versus non-sterilized swords. Among the participants, 58% (n = 29) used sterilized swords, a higher percentage than those using non-sterilized swords. However, the number of patients in the non-sterilized group remains considerable, with 21 patients, representing 42% of the total, as shown in Table 1.
| Sterilization Status | No. (%) |
|---|---|
| Sterilized/once use | 29 (58) |
| Not sterilized | 21 (42) |
| Total | 50 (100) |
Number and Percentage of Both Sterilized and Non-sterilized Swords
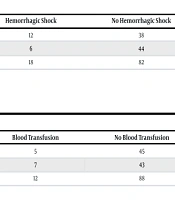
This study examines the association between head trauma resulting from Tatbir and other causes in relation to hemorrhagic shock. Among the 50 patients with head trauma attributed to Tatbir, 12 (24%) experienced hemorrhagic shock, while 6 out of 50 patients (12%) with head trauma from other causes developed hemorrhagic shock. The analysis showed no significant association between head trauma due to Tatbir and the occurrence of hemorrhagic shock, as indicated by a P-value of 0.11 (see Table 2).
| Conditions | Hemorrhagic Shock | No Hemorrhagic Shock | Total |
|---|---|---|---|
| Head trauma due to Tatbir | 12 | 38 | 50 |
| Head trauma due to other causes | 6 | 44 | 50 |
| Total | 18 | 82 | 100 |
Association Between Tatbir and Hemorrhagic Shock
This study examines the association between Tatbir and the need for blood transfusion. Among the 50 patients who underwent Tatbir, only 5 (10%) required a blood transfusion, while 7 out of 50 (14%) patients with trauma from other causes needed transfusions. Statistical analysis indicated no significant association between Tatbir and the necessity for blood transfusion, with a P-value of 0.53 (see Table 3).
| Conditions | Blood Transfusion | No Blood Transfusion | Total |
|---|---|---|---|
| Head trauma due to Tatbir | 5 | 45 | 50 |
| Head trauma due to other causes | 7 | 43 | 50 |
| Total | 12 | 88 | 100 |
Association Between Tatbir and Blood Transfusion
4. Discussion
To the best of our knowledge, Tatbir-related head injuries have not been reported in the literature, except for one article that considers the spectrum of head injuries associated with Tatbir. In the present study, there was a high number of non-sterilized swords used for Tatbir, raising concerns about major health problems related to the transmission of bloodborne infections such as hepatitis B or C viruses and human immunodeficiency virus (HIV). Most of the methods used for sterilization were inappropriate and depended on alcohol or povidone-iodine solution. Awareness of this major issue needs to be highlighted (18). This study also found no association between hemorrhagic shock and Tatbir-associated head injuries. This can be explained by the fact that most of these scalp wounds are small and tend to be superficial. They are mostly located on the sagittal and para-sagittal planes. This is consistent with the study by Hoz et al., which examined head injuries caused by Tatbir (17). However, Turnage and Maull found that some scalp lacerations could lead to severe hemorrhagic shock and even death. Of particular importance is that patients who present to the emergency department with shock may have minimal scalp bleeding due to the low perfusion pressure of the scalp vessels. Under such circumstances, these wounds may be initially dismissed and considered trivial. However, after initial resuscitation, blood pressure returns to normal, and bleeding from these scalp wounds becomes more profuse, resulting in a hemostatic challenge for the clinician (19). This study also found no statistically significant association between Tatbir-related head injuries and blood transfusion. This contrasts with the study by Boutin et al., which examined blood transfusion in patients with head traumas. They found that blood transfusion in this group is common but is associated with unfavorable outcomes (20).
4.1. Limitations
- The sample size was small compared to the large population that practices this religious ritual.
- Most patients refused or were unwilling to cooperate with researchers.
- All data were collected from the adult age group, even though there were patients in the pediatric age group.
4.2. Recommendations
- Conduct a study with a larger sample that includes the three holy cities: Karbala, Al-Najaf, and Al-Kadhimya.
- Determine the number of fluid packs, bandages, blood packs, sutures, and other logistics that could be used to help in preparation for this mass gathering event.
- Compare Tatbir-associated head injuries with each class of hemorrhage and define the most common type.
4.3. Conclusions
- The practice of Tatbir involves the use of a high number of non-sterilized swords, which raises major health concerns regarding the transmission of bloodborne infectious diseases.
- Tatbir-related head injuries were not associated with hemorrhagic shock.
- There was no association between Tatbir-related head injuries and blood transfusion.