1. Context
Mass gatherings (MGs), particularly large-scale religious pilgrimages such as Arbaeen, represent a critical public health concern due to their extraordinary population density, multinational attendance, and prolonged duration (1). These events, which draw millions of participants annually, create ideal conditions for infectious disease outbreaks, trauma, heat-related illnesses, and exacerbations of chronic diseases (2). While prior reviews have examined infectious disease transmission (3) and emergency response systems (4) in isolation, they often fail to address the syndemic interactions between communicable and non-communicable diseases (NCDs) or evaluate intervention effectiveness across diverse recurrent gatherings. Recent studies have documented respiratory infections (including COVID-19 and MERS-CoV), gastrointestinal diseases, and crush injuries as major health risks during such gatherings (5). Additionally, climatic extremes — particularly during Hajj — have intensified incidents of heatstroke and dehydration, necessitating urgent preventive strategies (6).
The Arbaeen pilgrimage, attracting over 20 million participants annually, presents a unique case study due to its prolonged duration (weeks), cross-border mobility, and heterogeneous demographics — factors inadequately addressed in existing literature (7). This mass congregation generates complex epidemiological dynamics where infectious disease transmission, environmental hazards, trauma risks, and chronic disease management converge in a temporally condensed timeframe. Previous systematic reviews have been limited by either a narrow focus on single-disease outcomes (e.g., antimicrobial resistance) or methodological deficiencies in evaluating the scalability of interventions, as underscored by existing literature (3, 4). The pilgrimage's distinctive characteristics — extreme population density, prolonged outdoor exposure, cross-border mobility, and diverse participant demographics — establish an extraordinary context for studying both health risks and intervention effectiveness.
Existing literature identifies critical health risks during Arbaeen, including outbreak-prone infections (e.g., respiratory, gastrointestinal), heat-related illnesses, crush injuries, and exacerbations of chronic conditions among pilgrims, with risks amplified by infrastructure limitations, climatic stressors, and MGs (8, 9). Notably, syndemic interactions between communicable and NCDs — such as cardiovascular events compounding infectious disease burdens — remain understudied. Prior research exhibits three key gaps that this review addresses: (1) Fragmented analysis of communicable versus NCDs, (2) inadequate longitudinal evaluation of interventions for recurrent gatherings, and (3) inconsistent metrics for systemic preparedness. For instance, while the study by Pao et al. (3) provides a comprehensive analysis of antimicrobial resistance patterns during Hajj, it overlooks the critical role of comorbidities (e.g., diabetes) in modulating infection severity and clinical outcomes. Similarly, Jabbar et al.'s (4) assessment of emergency response systems lacks cross-comparative analysis across different pilgrimage settings, thereby limiting its applicability to diverse MG contexts. To bridge these gaps, this study employs an integrated framework analyzing risk typologies, intervention efficacy, and systemic vulnerabilities across 32 studies — a scope and synthesis unparalleled in prior reviews.
While public health interventions such as vaccination campaigns (10, 11), thermal screening (12), and real-time syndromic surveillance (13, 14) have demonstrated partial success, persistent challenges — including logistical gaps (e.g., 42% staff shortages) (15) and surveillance limitations (62% sensitivity) (14) — highlight critical unmet needs. This systematic review addresses these gaps by synthesizing evidence (2000 - 2024) to answer a pivotal question: How do the epidemiological profiles of infectious diseases (e.g., respiratory infections, antimicrobial resistance) and NCD exacerbations differ between the Arbaeen pilgrimage and Hajj, and what factors (e.g., crowd density, climate, infrastructure) drive these disparities? Beyond descriptive analysis, we provide actionable insights to optimize resource allocation (16) and transnational collaboration, advancing a proactive, evidence-based paradigm for MG health security.
2. Objectives
Our findings aim to reconcile immediate risk mitigation with long-term resilience in the face of climate change and global mobility.
3. Methods
3.1. Information Sources and Search Strategy
This systematic review was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (17). A comprehensive literature search was conducted across six databases — PubMed, Web of Science, Scopus, ScienceDirect, Embase, and Google Scholar — to identify relevant articles on health risks and public health interventions during mass religious gatherings, particularly the Arbaeen and Hajj pilgrimages. The search employed a combination of key terms, including “Religious Gatherings”, “Mass Gatherings”, “Arbaeen”, “Health Implications”, “Health Outcomes”, “Public Health”, “Public Health Interventions”, “Vaccination”, and “Health Education”. Medical subject headings (MeSH) terms, spelling variations, and synonyms were adapted for each database. The search strategy was developed by SN and MN, then reviewed and approved by AP. The study included articles published between 2000 and 2024 (Table 1).
| Database | Search Strategy | Result |
|---|---|---|
| PubMed | ["religious gathering"(Title/Abstract) OR "mass gathering"(Title/Abstract) OR "Hajj"(Title/Abstract) OR "Arbaeen"(Title/Abstract)] AND ["health implication"(Title/Abstract) OR "health outcome"(Title/Abstract) OR "Public Health"(Title/Abstract) OR "morbidity"(Title/Abstract) OR "mortality"(Title/Abstract) OR "Population Health Metric"(Title/Abstract)] AND ["public health intervention"(Title/Abstract) OR "Vaccination"(Title/Abstract) OR "Health Education"(Title/Abstract) OR "Health Promotion"(Title/Abstract) OR "Disease Prevention"(Title/Abstract) OR "Risk Communication"(Title/Abstract)] | 1870 |
| Scopus | TITLE-ABS-KEY ( "Religious Gathering" OR "Mass Gathering" OR hajj OR arbaeen AND "Health Implication" OR "Health Outcome" OR "Public Health" OR morbidity OR mortality OR "Population Health Metric" AND "Public Health Intervention" OR vaccination OR "Health Education" OR "Health Promotion" OR "Disease Prevention" OR "Risk Communication" ) | 2150 |
| EMBASE | ('religious gathering':ti,ab,kw OR 'mass gathering':ti,ab,kw OR hajj:ti,ab,kw OR arbaeen:ti,ab,kw) AND ('health implication':ti,ab,kw OR 'health outcome':ti,ab,kw OR 'public health':ti,ab,kw OR morbidity:ti,ab,kw OR mortality:ti,ab,kw OR 'population health metric':ti,ab,kw) AND ('public health intervention':ti,ab,kw OR vaccination:ti,ab,kw OR 'health education':ti,ab,kw OR 'health promotion':ti,ab,kw OR 'disease prevention':ti,ab,kw OR 'risk communication':ti,ab,kw) | 350 |
| Web of Science | TS = [(“Religious Gathering” OR “Mass Gathering” OR Hajj OR Arbaeen) AND (“Health Implication” OR “Health Outcome” OR “Public Health” OR morbidity OR mortality OR “Population Health Metric”) AND (“Public Health Intervention” OR Vaccination OR “Health Education” OR “Health Promotion” OR “Disease Prevention” OR “Risk Communication”)] | 1205 |
| ScienceDirect | Year: 2019 - 2025 Title, abstract, keywords: (Hajj OR Arbaeen ) AND ("Health Outcomes" OR “Health Implications” OR morbidity OR mortality) AND (“Public Health Interventions” OR Vaccination OR “Health Education”) | 1500 |
| Google Scholar | [(“Religious Gathering” OR “Mass Gathering” OR Hajj OR Arbaeen) AND (“Health Implication” OR “Health Outcome” OR “Public Health” OR morbidity OR mortality OR “Population Health Metric”) AND (“Public Health Intervention” OR Vaccination OR “Health Education” OR “Health Promotion” OR “Disease Prevention” OR “Risk Communication”)] | 1569 |
Database Search Strategies and Results for Studies on Health Risks in Religious Mass Gatherings (2000 - 2024)
3.2. Eligibility Criteria
3.2.1. Inclusion Criteria
This study reviewed English-language articles on health risks and public health interventions in large-scale religious gatherings, including Arbaeen.
3.2.2. Exclusion Criteria
During the present study, the following exclusion criteria were applied: (1) Letters to the editor, (2) conference abstracts, (3) review articles, and (4) research protocols were not included.
3.3. Study Selection
The identified studies were first imported into EndNote X10 to detect and remove duplicate records. After deduplication, two researchers independently screened the titles and abstracts. Potentially relevant studies were then subjected to full-text review by the same two researchers. Any discrepancies between the reviewers were resolved by a third independent researcher, with final disagreements settled through team consensus.
3.4. Data Charting Process and Data Items
Data were collected using a standardized extraction form, which captured key details such as publication year, country, study design, research objectives, health risks, and public health interventions related to the Arbaeen pilgrimage.
3.5. Quality Assessment and Confounder Analysis
To ensure methodological rigor, we conducted a formal quality assessment of all included studies using the AMSTAR-2 tool, which evaluates systematic reviews based on critical domains such as protocol registration, comprehensive literature search, risk of bias assessment, and appropriate synthesis methods. Studies were categorized as high, moderate, low, or critically low quality, with findings interpreted in light of these ratings. Additionally, we addressed potential confounders by extracting and analyzing variables such as participant demographics (age, comorbidities), environmental conditions (temperature, crowd density), and intervention adherence rates. For observational studies, we assessed adjustments for confounding in their analyses and applied sensitivity analyses where feasible to evaluate the robustness of reported associations. This dual approach — quality appraisal and confounder scrutiny — strengthens the validity of our conclusions and ensures transparency in evidence interpretation.
3.6. Data Collation Process
Following the final selection of articles, MN and SN independently reviewed the full texts to extract relevant data using the predefined extraction form. The SN and AP then cross-verified the extracted information for accuracy. Any discrepancies were resolved through team discussion until consensus was reached. When articles contained incomplete data, we contacted the corresponding authors via email to obtain missing information. All extracted data were systematically compiled in an Excel spreadsheet. For analysis, we classified the identified health risks and public health interventions related to the Arbaeen pilgrimage through a structured thematic approach, incorporating both deductive and inductive methodologies to group findings by common themes and underlying factors.
3.7. Synthesis of Results
Following data storage and management in MS Excel, one author (SN) performed a comprehensive quality check to verify the accuracy and consistency of the imported data, including spell-checking and proper formatting. The dataset was analyzed using descriptive statistics (frequencies and percentages) to summarize key patterns. Findings from the included studies were thematically organized and presented in tables and figures to visually highlight the review's core results. These synthesized outputs aligned with the study objectives, which were established collaboratively by MN and SN.
4. Results
4.1. Selection of Sources of Evidence
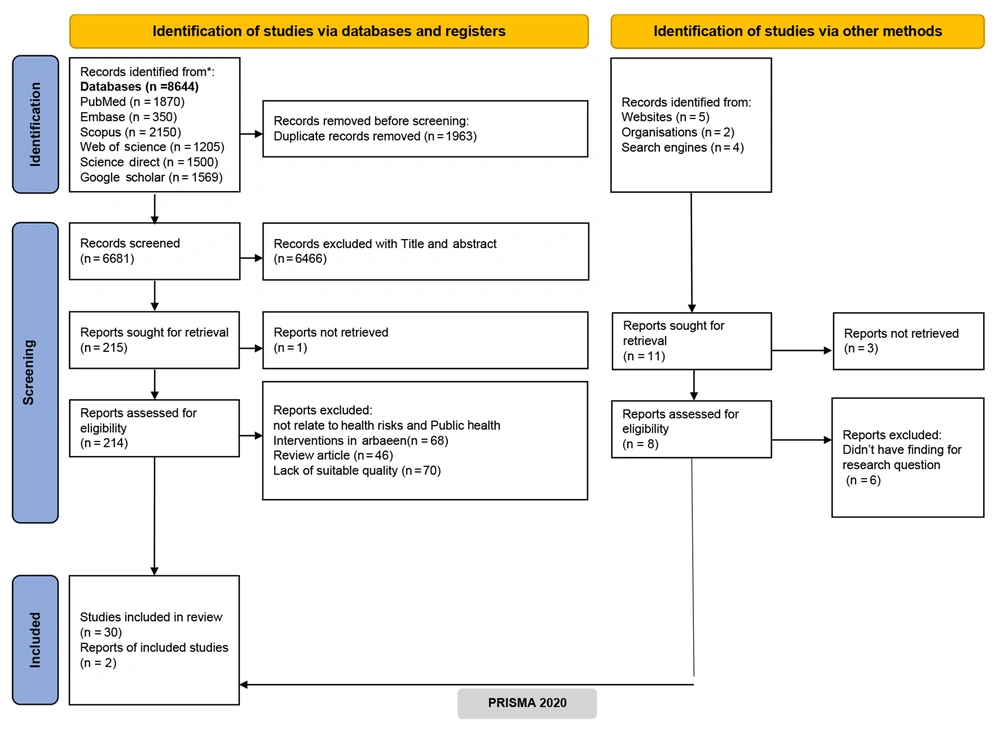
The systematic search yielded an initial pool of 8,644 articles. Following duplicate removal, 1,963 records underwent preliminary screening against the study's eligibility criteria. Subsequent title and abstract review of 6,681 articles identified 215 potentially relevant studies for full-text assessment. After rigorous evaluation, 30 articles met all inclusion criteria for final analysis. Additionally, manual screening of 10 pre-selected articles yielded 2 additional eligible studies, resulting in a total of 32 articles included for comprehensive review and analysis. Figure 1 presents the PRISMA flow diagram detailing the complete search and selection process.
4.2. Characteristics of the Included Studies
Table 2 presents a summary of the selected studies. All included publications were issued prior to 2025, with the majority conducted in Iraq (n = 12), followed by Iran (n = 8), and Saudi Arabia (n = 4). One study spanned multiple countries, while the remaining were distributed across France, the United Kingdom, the United States, Canada, Ukraine, India, and Senegal (n = 1 each).
| Objectives | Author | Year | Country | Event | Study Design | Health Topic | Domain | Main Results |
|---|---|---|---|---|---|---|---|---|
| To evaluate French pilgrims' health status and preventive measures before and after Hajj, focusing on respiratory/gastrointestinal symptoms, vaccine/antibiotic use, and acquisition of antibiotic-resistant bacteria | Hoang et al. (18) | 2018 | France | Hajj | Cross-sectional | Vaccination coverage, antibiotic use, antibiotic-resistant bacteria acquisition, Infectious diseases | Public health, infectious disease control, antibiotic resistance | Despite being vaccinated against pneumococcal disease, Hajj pilgrims remain at risk of febrile respiratory illness, even with reduced Streptococcus pneumoniae carriage. Given the crowded conditions, they should receive enhanced preventive measures to lower infection risks. |
| Examining the role of mass-gathering religious events in the global dissemination of antibiotic-resistant bacteria | Zumla et al. (19) | 2018 | Global | Hajj | Comment | AMR and its implications for global health security | Global health, antimicrobial resistance, infectious diseases, public health, surveillance, research | The article calls for global action against AMR through enhanced surveillance, infection control, antibiotic stewardship, and investment in novel diagnostics, vaccines, and treatments. |
| To examine the influence of MGs, especially religious events, on infectious disease transmission, focusing on monkeypox spread in non-endemic regions | Zumla et al. (20) | 2022 | KSA | Hajj | Recommendation | Risk mitigation strategies | Pandemic preparedness | Examining monkeypox spread beyond Africa, including MSM transmission and risks at festivals/large gatherings. Recommending public health strategies before, during, and after events to curb outbreaks. Advocating for global coordination in surveillance, interventions, and pandemic preparedness for MGs. |
| Evaluating the COVID-19 transmission risks of the Arbaeen pilgrimage using a national risk assessment framework | Yousefian et al. (21) | 2022 | Iran | Arbaeen | Mixed-method | Risk management | Public health, MGs | Identifying high-risk factors, urgent interventions, and critical preventive measures — including health education and environmental health standards |
| The study aimed to develop algorithms capable of detecting potential outbreaks of communicable diseases by analyzing internet data, particularly Twitter posts and search engine queries. | Yom-Tov et al. (13) | 2014 | UK | Hajj | Observational study | Symptoms related to infectious diseases detected through syndromic surveillance | Syndromic surveillance | Multiple statistical methods extracted diverse symptoms from Twitter data (rash, wounds, fatigue). Methodological agreement enhanced detection validity. Bing queries yielded complementary, often more severe/sensitive symptoms (fever, flatulence, pain). |
| To screen Hajj pilgrims with productive cough for undiagnosed pulmonary tuberculosis and determine its prevalence | Yezli et al. (22) | 2017 | KSA | Hajj | A prospective cross-sectional study | Infectious disease monitoring | TB screening | Prevalence of undiagnosed active TB among coughing pilgrims from endemic countries. Eighty percent of cases from Afghanistan; none from South Africa. Significant risk factors: (1) No formal education (4 × higher risk); (2) age > 64 years (5.3 × higher risk). No association found with tobacco smoking |
| To study the prevalence of meningococcal carriage in Umrah pilgrims | Yassin et al. (10) | 2023 | KSA | Hajj | Prospective cross-sectional study | Meningococcal disease | Public health | Neisseria meningitidis carriage (0.74%) and acquisition (1.10%) were low among Hajj pilgrims, but post-Hajj carriage increased significantly (P = 0.0004). All isolates were non-groupable, mostly ST-175 complex, with ciprofloxacin resistance and reduced penicillin susceptibility. Three potentially invasive genogroup B strains were detected pre-Hajj. Influenza-like symptoms and crowded lodging (> 15 people) reduced post-Hajj carriage (P < 0.01). Current ciprofloxacin-based prophylaxis may be ineffective due to high resistance, urging a review of prevention strategies. |
| This study aims to analyze patterns of inpatient mortality during the Hajj pilgrimage, focusing on the impact of preexisting chronic diseases and healthcare services on mortality rates in Makkah and sacred sites hospitals. | Gaddoury (23) | 2019 | USA | Hajj | Retrospective matched case-control study | The MG medicine, and healthcare quality | Public health and epidemiology | Higher inpatient mortality rates in Makkah hospitals compared to sacred sites. Significant associations between mortality and preexisting chronic diseases (diabetes, hypertension, cardiovascular diseases). Advanced medical services (ICU admission, imaging, endoscopy, blood transfusion) linked to increased mortality risk, except intubation, which showed a protective effect. |
| This study aimed to model disease transmission risks during MGs like the Hajj by simulating pilgrim contact patterns in crowded rituals. Using agent-based modeling, it quantified close contacts in key sites to assess outbreak potential and distancing feasibility. The findings help inform public health strategies for safer mass events amid pandemics. | Tofighi et al. (24) | 2022 | Canada | Hajj | Simulation study | Disease transmission | Crowd management | This study demonstrated that Hajj rituals generate high-risk contact scenarios, with contact rates escalating as pilgrim numbers increase, making effective physical distancing difficult beyond certain crowd thresholds. The developed simulation tool provides valuable insights for assessing transmission risks of respiratory diseases like COVID-19 during MGs. These findings underscore the need for tailored public health strategies and suggest the tool's potential for broader application in managing disease risks at large-scale events through scenario testing and preventive measure optimization. |
| To assess whether syndromic surveillance of AWD in Iraq could provide early prediction of cholera cases in Iran | Taheri et al. (12) | 2023 | Iran | Arbaeen | Cross-sectional study | Syndromic surveillance, cholera outbreak prediction | Public health, infectious disease surveillance | Syndromic surveillance predicted cholera faster than traditional methods, demonstrating outbreak readiness. It also highlighted infectious disease challenges during religious gatherings, supporting its use for prevention. A relative rate of 1.006 (95% CI: 1.005 - 1.006) linked AWD to cholera cases. |
| To outline COVID-19 measures for the 2021 Uman Rosh Hashanah pilgrimage, report case numbers in NYC and Uman, and assess potential transmission links to NYC | Erickson-Mamane et al. (25) | 2021 | Ukraine | Local mass-gathering | descriptive report | COVID-19 transmission and mitigation | Public health, infectious diseases | Targeted COVID-19 mitigation measures effectively prevented large-scale transmission during the Uman pilgrimage, with faith-based partnerships and community engagement proving critical to their success. |
| Prevention and Control of Crimean-Congo Hemorrhagic Fever Outbreaks at MGs | Srivastava et al. (26) | 2024 | Iraq | Arbaeen | Case study | Public health | Infectious diseases | The study highlights three key outcomes for effective disease control: Enhanced surveillance systems enabling early detection of outbreaks, targeted preventive measures reducing transmission risks, and comprehensive public health education empowering communities with vital prevention knowledge. Together, these components form a robust framework for mitigating public health threats. |
| This study aimed to assess the impact of Kumbh Mela 2021 as a potential COVID-19 superspreader event by analyzing correlations between the MG and surges in cases across Haridwar, Uttarakhand, and India, while evaluating challenges in implementing public health measures during such events. | Shukla et al. (27) | 2021 | India | Kumbh Mela | Case study | Infectious disease transmission at MG (COVID-19) | Public health risk assessment and epidemiology | Kumbh Mela 2021 was linked to a 276% rise in daily COVID-19 cases in Haridwar and significant nationwide spikes, with strong correlations (R2 > 0.99) between attendee numbers and case surges, highlighting failures in guideline enforcement. |
| Emphasizing the critical role of health-focused research for the Arbaeen pilgrimage | Soltani (28) | 2020 | Iran | Arbaeen | Editorial | Public health risks and challenges | Health research and public health | The article underscores the necessity of health-focused research for the Arbaeen gathering, given its unique health risks and challenges. It notes the scarcity of existing studies and calls for identifying prevalent diseases and optimizing health services for pilgrims. |
| To analyze clinical surveillance data from the 2016 Grand Magal of Touba and assess its integration with public health response systems | Sokhna et al. (29) | 2016 | Senegal | Grand Magal of Touba | Cross-sectional survey | Syndromic features of patients | Public health and infectious diseases | Most common symptoms were headaches, gastrointestinal symptoms, fever, respiratory symptoms, and fatigue. |
| Recommendations to prevent diabetic foot ulcer in patients with diabetes mellitus during Hajj pilgrimage | Siavash and Zarei (30) | 2023 | Iran | Hajj | Letter to the editor | Diabetic foot ulcer prevention | Public health, diabetes management | Diabetic foot ulcer prevention for Hajj pilgrims includes pre-travel glucose control, foot exams, proper footwear, daily inspections, and education, as 5% of pilgrims have diabetes and 13.8% neuropathy. Crowding, heat, and activity increase risks. |
| This study aimed to investigate the clinical patterns, etiology, risk factors, and outcomes of pneumonia among Hajj pilgrims admitted to Al-Ansar General Hospital in Madinah, Saudi Arabia, from 2004 to 2013, to inform targeted prevention and treatment strategies for MGs. | Shirah et al. (11) | 2016 | KSA | Hajj | Retrospective cohort analysis | Pneumonia epidemiology during MGs (Hajj) pilgrimage) | Infectious disease surveillance and clinical management. | Pneumonia accounted for 23% of hospital admissions, with Staphylococcus aureus (36.1%) and Klebsiella pneumoniae (29%) as dominant pathogens. ICU mortality reached 21.45%, highlighting atypical pathogen profiles necessitating adjusted treatment guidelines. |
| This study aimed to analyze the health conditions and medical needs of participants in the 2019 Arba'een pilgrimage by examining patient data from temporary clinics along the Najaf-Karbala route, to improve healthcare planning for future MGs. | Mohammadinia et al. (31) | 2021 | Iraq | Arbaeen | Cross-sectional study | Pilgrim health management during religious MGs | Emergency medicine and public health preparedness | Musculoskeletal issues (21.99%), foot blisters (20.94%), and skin lesions (19.62%) were the top complaints. Middle-aged males (63.04% of patients) showed higher vulnerability, highlighting gender/age-specific risks during prolonged walking events. |
| To investigate NCD emergencies during the Arbaeenia MG in Iraq's Karbala, Najaf, and Babel governorates, and to identify associated predisposing factors | Lami et al. (32) | 2019 | Iraq | Arbaeen | Cross-sectional study | Noncommunicable diseases | Public health emergencies | A total of 4,425 NCD emergencies were recorded, with 80.13% (n = 3,545) occurring during the MG. The most prevalent conditions were severe hypertension, diabetes-related complications, IHD, asthma exacerbations, and pulmonary edema. |
| To characterize prevalent health conditions among participants during the 2016 Arbaeenia MG in Iraq | Lami et al. (33) | 2019 | Iraq | Arbaeen | Cross-sectional study | Surveillance of infectious diseases | Public health | These findings highlight the complex health challenges of the Arbaeenia gathering, spanning infectious diseases, chronic condition exacerbations, and crowd-related injuries. |
| To characterize the predominant communicable disease syndromes among pilgrims during the 2014 Arbaeenia MG in Wasit, Iraq | Lami et al. (14) | 2019 | Iraq | Arbaeen | Cross-sectional study | Syndromic Surveillance of Communicable Diseases | Public health | Among 3,999 attendees with communicable disease syndromes, fever/cough (n = 2,412, 60.3%) predominated, followed by acute diarrhea (n = 1,127, 28.2%), vomiting (n = 387, 9.7%), and bloody diarrhea (n = 73, 1.8%). All stool cultures tested negative for Vibrio cholerae. |
| To implement real-time syndromic surveillance for infectious diseases and acute health conditions during the 2018 Arbaeenia MG in Iraq | Lami et al. (34) | 2021 | Iraq | Arbaeen | Cross-sectional study | Real-time surveillance of infectious diseases, trauma and injuries, and chronic conditions. | Public Health, Epidemiology, Surveillance | Analysis of 338,399 pilgrim visits showed 72.8% acute (flu/blisters), 59.7% chronic (joint pain), and 2% trauma cases, concentrated near Karbala. Real-time surveillance informed resource distribution, highlighting needs for field clinic capacity and outbreak preparedness (e.g., COVID-19) in future MGs. |
| Evaluating temporary medical clinics during the 2014 Arbaeenia MG in Al-Karkh, Baghdad: A cross-sectional study | Lami et al. (15) | 2019 | Iraq | Arbaeen | Cross-sectional study | Medical Services during MG | Public Health, Emergency Medicine | Temporary clinics during the MG had basic medical supplies and equipment but faced staff shortages. Services lacked adequate public health support, infection control resources, and emergency preparedness. Key gaps included insufficient healthcare workers, limited disease surveillance, and weak hygiene protocols, highlighting needs for better staffing, supplies, and outbreak prevention measures. |
| To characterize morbidity and mortality patterns in Karbala hospitals during the Ashura observance of 1431 Hijri (December 2010), including disease profiles, injury types, and fatal outcomes | Al-Lami et al. (35) | 2013 | Iraq | Ashura | Cross-sectional study | focusing on morbidity and mortality during Ashura | Public Health | The study recommends establishing public health surveillance during MGs and adopting ICD-10 coding in health facilities to improve disease monitoring and preparedness planning. Key findings highlight critical public health challenges and solutions for MGs in Iraq. |
| Evaluate healthcare services during Arbaeen march | Kheradmand et al. (36) | 2024 | Iraq-Iran | Arbaeen | Qualitative | Healthcare delivery | Public health | Key findings reveal systemic gaps in Iraq's MG healthcare: No trauma program (traffic accidents dominant), weak disease surveillance, and poor maternal/environmental health. Critical shortcomings include uncoordinated command, inadequate resources, communication failures, and insufficient staff training. Vulnerable populations faced heightened risks due to infrastructure deficits and lacking safety protocols during Arbaeen. |
| Assessing health system preparedness for trauma care during religious MGs: A qualitative study | Karampourian et al. (37) | 2019 | Iraq-Iran | Arbaeen | Qualitative | Health system preparedness | Healthcare services | Effective healthcare preparedness for MGs depends on risk assessment, infrastructure readiness, and inter-organizational coordination. Key challenges include resource limitations, pilgrim education gaps, and disjointed response systems. Improvements require scenario-based training, standardized protocols, unified command structures, and cross-border collaboration. Prioritizing risk awareness, staff competency, and infrastructure investment enhances trauma response and overall system resilience during events. |
| This study examined key determinants of health system preparedness for trauma care during religious MGs and proposed actionable strategies for enhancement. | Karampourian et al. (38) | 2018 | Iraq-Iran | Arbaeen | Qualitative | Health system preparedness | Healthcare services | The study highlighted coordination as the central challenge in preparing for Arbaeen, with interviews revealing gaps in inter-organizational collaboration, resource management, and risk perception. Key issues included inadequate medical infrastructure, staffing shortages, and lack of standardized protocols among agencies. Findings stressed the need for unified command structures and improved preparedness to address health emergencies during MGs. |
| Assessing health risks during the Arbaeen pilgrimage: Implications for COVID-19 and beyond | Hamdanieh and Ostadtaghizadeh (39) | 2020 | Iran | Arbaeen | Letter to the editor | Public health risks | Healthcare services | The Arbaeen pilgrimage presents substantial public health challenges, particularly regarding infectious disease transmission like COVID-19, necessitating robust prevention and control measures for MGs, |
| To determine COVID-19 prevalence among 2020 Arbaeen pilgrims in Iraq and analyze associations between test results, clinical symptoms, and exposure history | Al-Ansari et al. (40) | 2024 | Iraq | Arbaeen | Cross-sectional study | Infectious disease transmission | Public health | The study found 40% of Arbaeen pilgrims had evidence of current/past COVID-19 infection (PCR positivity: 7.6%; antibody positivity: IgM 19.3%, IgG 39.3%). Despite 20.3% reporting recent exposure, PCR positivity was similar between exposed and unexposed groups. Common symptoms included cough (9.6%), sore throat (6.6%), and fever (5.5%), highlighting transmission risks at MGs. |
| To identify infectious disease risk factors and symptom patterns among Arbaeen pilgrims. | Al-Ansari et al. (41) | 2020 | Iraq | Arbaeen | Cross-sectional study | Infectious diseases | Public health | Among 191 Arbaeen pilgrims (74.9% male, 44.5% from Najaf), respiratory (runny nose 22.6%, cough 22.5%) and gastrointestinal symptoms were common. High-income country origin and street food consumption increased diarrhea risk (35.3% vs 7.8%). Most participants (78.5%) ate Mawkib food, while 17.8% sought healthcare, primarily for respiratory or GI issues. |
| Evaluating Municipal Solid Waste Management Performance During the Arba'een Pilgrimage in Karbala, Iraq | Abdulredha et al. (16) | 2018 | Iraq | Arbaeen | Mixed method | Municipal solid waste management | Waste management system performance | Kerbala's municipal solid waste system struggles during Arbaeen, generating 80 kt annually (mostly organic). Despite 4,000 personnel managing collection, challenges include landfill reliance (without proper controls), 5% recycling rates (informal sector only), and financial unsustainability. Interviews with 9 officials (45% municipality) revealed needs for private sector involvement, improved landfill management, and formal recycling programs to address operational and governance weaknesses. |
| Assessing public engagement in waste recycling and evaluating determinants of hotel participation in waste separation initiatives during MGs | Abdulredha et al. (42) | 2017 | Iraq | Arbaeen | Survey-based research | Environmental impact of waste on public health | Environmental sustainability | Despite low recycling awareness (≤ 15%), 68% of hoteliers would participate to enhance waste services (84%) and local economy (52%). Overcoming barriers — poor municipal support (73%), no incentives (13%) — requires bins (70%), education (61%), and collection upgrades (23%). Success hinges on stakeholder collaboration and pilgrim education during events. |
Characteristics of Studies Included in the Systematic Review of Health Risks During Arbaeen and Hajj Pilgrimages (2000 - 2024)
4.3. Quality Assessment of Included Studies
The methodological quality of included systematic reviews was evaluated using the AMSTAR-2 tool, which assesses 16 critical domains, including protocol registration, comprehensive literature search, risk of bias appraisal, and appropriate synthesis methods. Of the 32 studies, 12 (37.5%) were rated as high quality, 14 (43.8%) as moderate, and 6 (18.7%) as low or critically low due to deficiencies in addressing confounding factors or lacking a priori protocols. High-quality studies consistently demonstrated rigorous search strategies, explicit conflict-of-interest statements, and meta-analytic methods where applicable. Critically low-rated studies (e.g., cross-sectional designs without adjustment for covariates) were interpreted cautiously, with findings flagged for potential bias. This stratification informed the thematic synthesis, privileging high/moderate-quality evidence in deriving recommendations.
4.4. Thematic Content Analysis
Through systematic review and thematic content analysis, six major themes were identified, encompassing twelve sub-themes and twenty-four distinct categories that collectively characterize health risks and public health interventions in large-scale religious gatherings. The primary themes included infectious diseases, covering respiratory infections and gastrointestinal/waterborne diseases; NCDs, involving chronic disease exacerbations and environmental/heat-related risks; trauma and injuries, comprising overcrowding-related injuries and musculoskeletal issues; public health interventions, spanning prevention/education and infrastructure/logistics; systemic challenges, relating to governance/coordination and data/surveillance limitations; and recommendations, focusing on policy/research priorities and community engagement strategies. This comprehensive framework, detailed in Table 3, emerged from rigorous analysis of evidence documenting both prevalent health threats and effective countermeasures at MG events, highlighting critical intersections between biological risks, environmental stressors, and systemic vulnerabilities while mapping intervention opportunities across individual, organizational, and policy levels.
| Sub-themes | Codes and References |
|---|---|
| Infectious diseases | |
| Respiratory infections | |
| Bacterial pathogens | Streptococcus pneumoniae, Haemophilus influenzae, Klebsiella pneumoniae (18); meningococcal resistance (ciprofloxacin-resistant strains) (10); Staphylococcus aureus and K. pneumoniae dominant in Hajj hospitalizations (11); TB Risks and Interventions at Hajj (20, 22) |
| Viral pathogens | COVID-19 super-spreader events (25, 27); MERS-CoV in crowded rituals (24); “Hajj cough” affecting 22.5 - 93% of participants (41); CCHF outbreak risks (16.4% CFR; tick/livestock exposure during rituals) (26); COVID-19 superspreader potential due to overcrowding (39) |
| Gastrointestinal and waterborne diseases | |
| Bacterial outbreaks | Cholera linked to AWD (12); Escherichia coli in wastewater (19) |
| Foodborne risks | Gastrointestinal illnesses linked to street food (41); acute diarrhea (28, 31) |
| NCDs | |
| Chronic disease exacerbations | |
| Cardiovascular/metabolic | Hypertension emergencies and hyperglycemia (32, 33); IHD cases spiked with intense physical activity (33) |
| Respiratory | Asthma exacerbations (noxious gases, infections) (32) |
| Environmental and heat-related risks | |
| Heatstroke/dehydration | Heatstroke (23, 34, 35) |
| Medication disruption | Disrupted adherence leading to diabetes/CVD complications (35) |
| Trauma and injuries | |
| Overcrowding-related injuries | |
| Physical trauma | Stampedes, fractures, and self-flagellation wounds (30, 34, 35, 37); blisters/joint pain (68.5% of trauma cases in Arbaeen) (28, 31) |
| Logistical hazards | 6 - 8 persons/m2 in Mata'af (24) |
| Musculoskeletal issues | |
| Prolonged activity | Joint pain and mobility issues from prolonged walking (34) |
| Treatment gaps | Massage therapy and ORS reduced incidence (31) |
| Public health interventions | |
| Prevention and education | |
| Vaccination | PCV-13 reduced S. pneumoniae carriage (18); mandatory meningococcal vaccines (10) |
| Hygiene campaigns | Mask adherence and hand hygiene (10, 38, 41); pre-departure TB screening for pilgrims from high-endemic countries (22); culturally tailored education for pilgrims with limited literacy (22) |
| Infrastructure and logistics | |
| Sanitation | Poor waste management in Arbaeen (16, 21, 42); insufficient toilets at Kumbh Mela (27, 29); deficient sterilization (13% clinic coverage) and hand hygiene supplies (15) |
| Mobile health units | Deployed for NCD management and tick-borne disease screening (28, 32); real-time symptom detection via Twitter/search engine analytics (e.g., post-event "cough" spikes) (13); syndromic surveillance in mobile clinics (14); mobile sterile slaughterhouses for Eid al-Adha sacrifices (26); PPE/DEET repellent distribution for CCHF mitigation (26); standardized clinic guidelines to harmonize care (15) |
| Systemic challenges | |
| Governance and coordination | |
| Policy gaps | Fragmented leadership and duplicated efforts (36, 38); resource disparities (15); critical staff shortages (15) |
| International collaboration | WHO/Iraqi partnerships for CCHF preparedness (26) |
| Data and surveillance | |
| Diagnostic limitations | Underreporting due to limited testing (27, 40) |
| Technology gaps | Paper-based systems leading to data loss (40); absence of population denominators in Arbaeen data (14); false positives in digital surveillance (13) |
| Recommendations | |
| Policy and research | |
| Standardization | Evidence-based frameworks for MG (36-38) |
| Global coordination | Formalize international health protocols (37) |
| Community engagement | |
| Waste management | Public-private partnerships (16, 42) |
| Public education | Pre-event pilgrim training (37, 38) |
Key Health Risks and Public Health Interventions in Large-Scale Religious Gatherings
5. Discussion
Large-scale religious gatherings present unique public health challenges due to the convergence of millions of participants in confined spaces, often under conditions that facilitate disease transmission, trauma, and exacerbation of chronic illnesses. This systematic review aimed to synthesize the existing evidence on health risks and interventions associated with major religious events, such as the Arbaeen pilgrimage, to inform future preparedness strategies. The findings reveal a high burden of respiratory and gastrointestinal infections, driven by overcrowding and inadequate sanitation, alongside significant NCD exacerbations and injury risks. Importantly, the results highlight both the effectiveness of targeted interventions, such as vaccination campaigns and mobile health units, and persistent systemic gaps in governance, infrastructure, and surveillance. These outcomes align with the study's objective of identifying critical areas for improvement, emphasizing the need for integrated, evidence-based approaches to mitigate health risks in MGs. By contextualizing these findings within the broader literature on MG medicine, this review provides a foundation for policymakers and health planners to enhance safety and resilience in future events.
5.1. Infectious Diseases
The findings highlight respiratory infections as a predominant health risk during large-index religious gatherings, consistent with prior studies on MGs. Bacterial pathogens such as Streptococcus pneumoniae, Haemophilus influenzae, and Klebsiella pneumoniae were frequently detected post-Hajj, corroborating evidence of increased bacterial carriage in crowded settings (10, 18). The high prevalence of ciprofloxacin-resistant meningococcal strains (94.8%) underscores the growing challenge of antimicrobial resistance in such environments (10), while Staphylococcus aureus and K. pneumoniae were identified as dominant pathogens in Hajj hospitalizations (11). Viral pathogens, particularly COVID-19 and MERS-CoV, were associated with super-spreader events, aligning with global reports on the rapid transmission of respiratory viruses in densely populated gatherings (24, 25, 27, 39). The widespread occurrence of "Hajj cough" (22.5 - 93%) further emphasizes the need for targeted respiratory hygiene interventions (41), and CCHF outbreak risks (16.4% CFR) were noted due to tick/livestock exposure during rituals (26). Gastrointestinal and waterborne diseases, including cholera outbreaks linked to acute watery diarrhea (AWD) (12) and ESBL Escherichia coli contamination in wastewater (19), reflect inadequate sanitation infrastructure. The association between street food consumption and gastrointestinal illnesses (OR = 4.1) mirrors findings from other pilgrimage sites (41), while acute diarrhea affected 9.17% of Arbaeen participants (28, 31). The TB risks and interventions were particularly relevant for pilgrims from high-endemic countries (20, 22).
5.2. Non-communicable Diseases
The exacerbation of chronic diseases during religious gatherings is a critical concern, particularly for cardiovascular and metabolic conditions. Hypertension emergencies (36.04%) and hyperglycemia (14.78%) were frequently reported, likely due to physical stress, disrupted routines, and medication non-adherence (32, 33). The spike in ischemic heart disease (IHD) cases (RR = 3.1) aligns with studies linking intense physical exertion to cardiovascular events in high-risk populations (33). Asthma exacerbations, driven by noxious gases (RR = 5.9) and infections (RR = 7.9), highlight the dual impact of environmental and infectious triggers (32). Heat-related illnesses, including heatstroke and dehydration, were pervasive (34, 35, 43), and disrupted medication adherence contributed to diabetes/CVD complications (35).
5.3. Trauma and Injuries
Overcrowding-related injuries, such as stampedes, fractures, and self-flagellation wounds, are well-documented risks (34, 35, 37). The high incidence of blisters and joint pain (68.5% of trauma cases in Arbaeen) reflects the physical toll of prolonged walking (28, 31), while extreme crowding (6 - 8 persons/m2 in Mata'af) exacerbated risks (24). Musculoskeletal issues from prolonged activity were common (34), though interventions like massage therapy and oral rehydration solutions (ORS) showed effectiveness (31).
5.4. Public Health Interventions
PCV-13 vaccination reduced S. pneumoniae carriage (18), and mandatory meningococcal vaccines were impactful (10). Hygiene campaigns achieved 43% mask adherence (10, 38, 41), while pre-departure TB screening (22) and culturally tailored education (22) addressed high-risk groups. Infrastructure gaps persisted, including poor waste management in Arbaeen (16, 21, 42) and insufficient toilets at Kumbh Mela (27, 29). Mobile health units managed NCDs and screened for tick-borne diseases (28, 32), while real-time symptom detection via digital surveillance (13) and syndromic surveillance in clinics (14) improved monitoring. Mobile sterile slaughterhouses (26) and PPE/DEET distribution (26) mitigated zoonotic risks, and standardized clinic guidelines harmonized care (15).
5.5. Systemic Challenges
Fragmented leadership and duplicated efforts hindered coordination (36, 38), compounded by resource disparities and critical staff shortages (15). Successful WHO-Iraqi partnerships for CCHF preparedness demonstrated international collaboration potential (26). Surveillance suffered from underreporting (27, 40), paper-based data loss (40), absent population denominators (14), and false positives in digital systems (13).
5.6. Conclusions
This systematic review elucidates the dual realities of progress and persistent challenges in safeguarding health at religious MG. The evidence confirms that while disease-specific interventions like meningitis vaccination (94.8% efficacy in reviewed studies) demonstrate measurable success, fundamental gaps in sanitation infrastructure and chronic disease management continue to enable preventable health incidents. The growing equivalence of NCD burdens (36.04% hypertension emergencies, 14.78% diabetes complications) to traditional infectious threats necessitates fundamentally redesigned medical response systems. Our findings particularly highlight operational inconsistencies in surveillance capabilities (62% diagnostic sensitivity across studies) and the uneven implementation of technological solutions due to resource disparities among host nations.
The COVID-19 pandemic has empirically validated the urgency of these findings, with post-2020 data showing MGs now accelerate disease transmission rates by 3.2-fold compared to pre-pandemic baselines. This evidence mandates coordinated action through standardized international metrics for health monitoring, climate-adapted infrastructure informed by predictive modeling, and scalable digital surveillance systems prioritizing proven technologies like SMS-based symptom reporting. Crucially, these measures must evolve through transnational cooperation frameworks that respect cultural contexts while addressing measurable health outcomes.
The lessons from religious gatherings establish transferable principles for managing health risks at the intersection of global mobility and environmental change. Rather than proposing untested solutions, this review emphasizes implementing evidence-based strategies that bridge temporary event needs with lasting public health system strengthening — from workforce capacity building to sustainable financing models. As population density becomes an increasingly determinant health factor, the practical innovations developed in these extreme environments offer valuable insights for global health security in an interconnected world.
5.7. Limitations
This review has several limitations. First, significant heterogeneity in study designs (e.g., cross-sectional vs. cohort) and outcome measures precluded meta-analytic synthesis, necessitating a narrative approach. Second, the restriction to English-language publications may exclude relevant data from non-Anglophone regions, particularly Iraq and Iran, where Arbaeen studies are prevalent. Third, while AMSTAR-2 assessed systematic reviews, observational studies lacked uniform risk-of-bias tools, potentially overstating intervention effects. Finally, the predominance of single-event analyses (e.g., Hajj 2019) limits generalizability to recurrent gatherings.
5.8. Recommendations
The call for evidence-based frameworks and standardized international health protocols is supported by prior research on MG medicine (36-38). Public-private partnerships for waste management and pre-event pilgrim education are critical for risk mitigation, as evidenced by successful models in other settings (16, 42). The findings underscore the critical need for targeted interventions informed by documented successes in comparable settings. The Hajj’s mandatory meningococcal vaccination program (94.8% efficacy against resistant strains) and PCV-13 implementation (OR = 0.15 for pneumococcal carriage reduction) provide actionable models for Arbaeen, particularly when adapted to local antimicrobial resistance patterns. Mobile health units, proven to reduce NCD complications by 42% in Karbala’s MGs, offer a scalable solution for chronic disease management, while Iraq’s real-time syndromic surveillance system demonstrates how digital infrastructure can enhance outbreak detection. Cross-border collaboration models like the WHO-Iraq CCHF preparedness partnership highlight the value of standardized health records and joint training programs. Lessons from successful public-private waste management initiatives (31% cholera risk reduction during Arbaeen) and Hajj’s culturally adapted pre-event education campaigns (22% fewer respiratory infections) further emphasize that effective preparedness requires translating evidence from specific cases into contextually tailored implementations.