1. Background
Nosocomial infections are one of the leading causes of morbidity and mortality, affecting 10% to 13% of hospitalized patients (1). Three-quarters of these infections are related to four factors, including surgical site infection, catheter-related bloodstream infection, ventilator-associated pneumonia, and catheter-associated urinary tract infection (2). Patients admitted to intensive care units (ICUs) are more likely to develop these infections (3). The most common side effect of hospitalization in ICUs is nosocomial infection. More than 20% of all nosocomial infections occur in ICUs and the resulting mortality rate is 10% to 30% (4).
About 40% of patients hospitalized in ICUs for an average of five days or more develop a urinary tract infection (UTI) (5). Urinary tract infections can cause serious complications such as pyelonephritis, bacteremia, and endocarditis. In addition to prolonging hospitalization, they can increase mortality, cause psychological stress for patients and families, increase costs, and reduce the quality of health care (6). There are about two million cases of catheter-associated UTIs in the United States, and the cost of health care amounts to more than $400 million a year (7).
In the United States, more than 13,000 deaths yearly are estimated to be related to catheter-associated urinary tract infections (CAUTIs) (8). Urinary catheterization is the cause of 75% of UTIs. In addition, long-term catheterization is the most important risk factor for UTIs. The urinary catheter blocks the urethra and stimulates the bladder mucosa, and by creating an artificial pathway causes entering microorganisms to the urinary system (9, 10). In a study conducted in Iran, 30.9% of the patients in the ICUs with nosocomial infections had UTIs (11). Urinary tract infection is the most common infectious disease which occurs out of intestinal in women worldwide, with a prevalence of 53,067 per 100,000 women. Susceptibility of women to UTIs might increase due to anatomical (i.e., shortness of the urethra that makes an ideal bridge for pathogen invasion and its rapid progression towards the bladder), behavioral, and physiological factors that develop during a woman’s lifetime. These factors have made the incidence of UTIs more common in women than in men (12).
To prevent the incidence of UTIs in patients with urinary catheter, several strategies have been recommended including the use of a sterile closed system, emphasis on aseptic catheter insertion technique, catheter care, short-term antibiotic therapy, the use of antimicrobials around the urethra, addition of antimicrobial drugs to the urine bag, and application of catheters impregnated with antimicrobial agents (13). However, this complication, as an important health problem, threatens the health of patients. Colonized microorganisms in the perineal skin and around the urethra can move into the urinary system through the outer surface of the urinary catheter and cause infection (14). Therefore, interventions designed to prevent the colonization of pathogens around the urinary tract can be very important in controlling CAUTIs (15). One of these interventions is the proper care of the perineal area. For perineal care, the area is washed with a suitable solution. Washing the perineal area prevents catheter-associated urinary infections by reducing microbial colonization (16).
Numerous studies have been conducted on perineal care. Recommended methods include washing the perineal area with soap and water, normal saline solution, chlorhexidine, skin foams, and even just water (17-19). There is no consensus on what is the best material for washing and caring for the perineal area. Some nursing sources have suggested normal saline solution, some soap and water, and some others a disinfectant according to hospital policy (20-22).
Among the recommended methods, the most common method is using normal saline (23). The cleansing properties of normal saline are merely mechanical in removing contaminants from the perineal area (16). As this solution has no antimicrobial properties, the organisms can colonize the perineal area without clearly being visible and enter the urinary system, and consequently cause UTIs (24). Compared to normal saline, chlorhexidine solution is a disinfectant and a biguanide antiseptic, which affects all pathogenic microorganisms, including gram-positive and gram-negative bacteria, viruses, molds, yeasts, mycobacteria, and spores (25). Chlorhexidine is highly cationic, and one of its advantages is its binding and strong adhesion to most areas, which causes this substance to release gradually and slowly after consumption within a certain time frame to constantly provide an antimicrobial environment. This has resulted in a better and more lasting effect of chlorhexidine than other washing solutions used in ICUs (26). Concerning the mechanism of action, chlorhexidine has a positive electric charge while bacteria are negative; then, it binds to the body of bacteria and destroys their cytoplasm, or stops their growth. Thus, this solution is both bacteriostatic and bactericide (27). Chlorhexidine is active on the site for at least six hours, reducing both inhabiting and migrating skin bacteria, and is unique in this respect (28). It also works in a short time, is not toxic to tissues of the human body, has enough penetration power, and is cheap and easily portable (29). Numerous studies have been conducted on perineal care and washing with chlorhexidine solution. Michell et al. (30) compared the effect of washing the perineal area with 0.1% chlorhexidine and 0.9% normal saline on the reduction of asymptomatic bacteriuria in ICUs. The results showed that the rate of bacteriuria in the chlorhexidine group decreased statistically compared to the normal saline group. In the above study, 0.1% chlorhexidine mouthwash was used only to clean the meatal area during catheterization. Also, a study by Plantier et al. (31) assessed the effect of chlorhexidine on the prevention of CAUTIs in ICUs, and the results showed that the use of chlorhexidine before catheterization significantly reduced CAUTIs. It should be noted that they used chlorhexidine only for disinfection during catheter insertion, without performing daily washing.
2. Objectives
Although significant advances have been made in the treatment and prevention of nosocomial infections, UTIs are a major health problem. Catheter-associated urinary tract infections play a major role in the development of nosocomial infections. Despite all advances made in urinary catheter care and closed urinary collection systems, patients with CAUTIs still have frequent problems. A suitable solution for washing the perineal area can help the clinical staff to prevent such problems. Therefore, this study was conducted to determine the effect of perineal care using normal saline and 2% chlorhexidine solution on the incidence of CAUTIs in women hospitalized in the ICU of Khatam Al-Anbia Hospital in Zahedan in 2019.
3. Methods
The current two-group quasi-experimental study was conducted after receiving the approval of the Vice-Chancellor for Research and Technology and the Ethics Committee of Zahedan University of Medical Sciences in the ICU of Khatam Al-Anbia Hospital of Zahedan between June and December 2019.
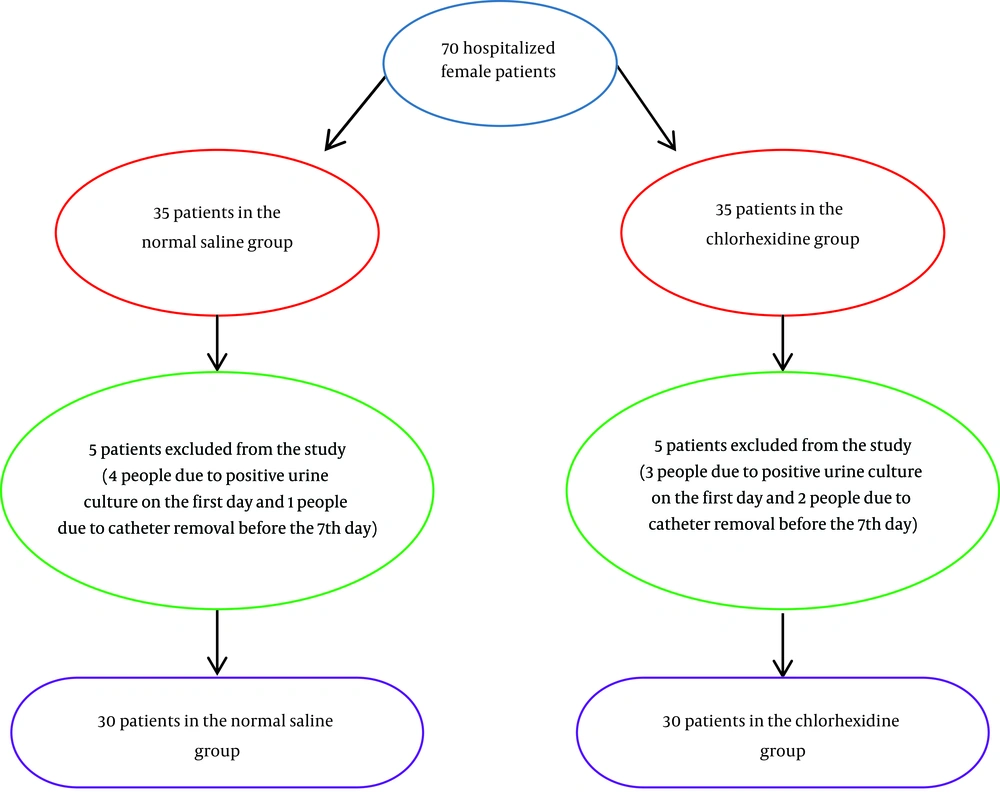
Eligible patients with the inclusion criteria were selected through convenience sampling and were randomly assigned to two intervention groups of normal saline and chlorhexidine (n = 35 in each) using shuffling cards. To randomize the selection, 70 color cards were used, including 35 blue cards for the normal saline group and 35 green cards for the chlorhexidine group. Upon admission, the cards were picked up by patients’ legal guardians to place the patient in the appropriate group based on the color of the chosen card. The card was returned to the box to keep the number 70 for the next selection. A two-digit code was assigned to each patient to make it easier to follow up and blind the laboratory.
The inclusion criteria were an age between 18 and 55 years, having GCS of 8 or lower, having a urinary catheter for at least seven days, no history of UTI, no congenital urinary tract disorders, no malignancy and immune deficiency, no diabetes, no history of urinary system manipulation in the past six months, no vaginal infection, no genital sores, and no sensitivity to chlorhexidine solution. To assess the sensitivity to chlorhexidine before its administration, an area of the patient’s forearm with a 5-cm diameter was immersed in the chlorhexidine solution and monitored for 15 to 20 min; if no hypersensitivity reaction occurred such as itching and redness, the patient was allowed to enter the study. The exclusion criteria were as follows: the lack of willingness of the patient’s family or legal guardian to continue participating in the study, positive urine culture on the first day, death of the patient, transfer of the patient to other wards before completing the study, catheter removal before the seventh day, abdominal or pelvic surgery, allergy to chlorhexidine solution, and wound formation in the genital area. The patient’s medical records were used to extract clinical information.
The sample size was calculated according to the study by Samimi et al. (32) with a confidence interval of 95% and a statistical power of 95%. Accordingly 29 patients were in each group (P1= 0.3; P2 = 0.73). To consider possible attrition and ensure the adequacy of the sample size, 35 patients in each group, and 70 patients in total were finally investigated (32).
The instruments used included demographic and clinical data collection forms (age, marital status, level of education, medical diagnosis, presence of underlying disease, use of antibiotics, intake of fluids, and urinary output) and laboratory culture results. The diagnosis of CAUTI was made based on the result of the urine culture test. According to reliable sources (33, 34), in case the number of colonies was 105 per milliliter or more, it was considered a positive infection.
The procedure was performed by the researcher in the emergency ward of the hospital. Patients who met the inclusion criteria to enter the study were selected through convenience sampling. After explaining the purpose of research and the method of work, the written consent forms were completed by the patients’ legal guardians. The selected patients were then randomly placed in two groups of chlorhexidine and normal saline. The catheterization was performed by the researcher according to standard guidelines (21). To ensure that there is no urinary tract infection at the beginning of the study, a sterile urine sample was obtained for the first culture through the urinary catheter. After 48 hours, the urine culture was evaluated, and patients who had a positive urine culture were excluded from the study. The washing of the perineal area was performed for seven consecutive days, once every 12 hours, with normal saline solution 0.9% in the normal saline group and chlorhexidine solution 2% in the chlorhexidine group. To wash the perineal area, a private environment was prepared, the patient was placed in the lithotomy position while the body was covered with sheets, and only the perineal area was exposed. After wearing clean gloves, the researcher washed the perineum, which started from the clean area and moved to the contaminated part.
The procedure continued by washing the labia majora, labia minora, clitoris, and finally urethra from top to bottom. A new gauze was used for each part. The meatus (urethral opening) and the outer five centimeters of the urinary catheter were also cleaned with a separate gauze. If the patient had defecation, the anal area was first cleaned with water and dried, and then the perineum was washed. During perineal care, the urinary catheter was not moved or displaced. In the end, the area was dried and the patient was placed in the initial position. For the second culture, a urine sample was prepared again on the seventh day and sent to the laboratory. To do this, the urinary catheter was clamped for 20 - 30 min, and then the site of the connection of the urinary catheter to the urine bag was disinfected with 70% alcoholic cotton. After disconnecting the catheter from the urine bag, a sample was taken from the end of the catheter, and then the patient’s urine catheter was removed. Next, urinary catheterization was performed by the medical staff, and the patient was excluded from the study.
The samples were labeled and transferred to the laboratory inside a cold box along with the relevant forms. The time interval between taking a urine sample and culture was less than two hours. The laboratory technician and data analyst were blinded to the study groups. Urine samples were cultured using calibrated loops in blood agar and EMB media. After culture, plates were labeled and incubated for 48 hours in an incubator at 37°C. If no colony grew a negative result, was reported. In plates with colony growth, the number of colonies was counted and multiplied by the reverse coefficient of loop volume. If the number of colonies was more than 105 per milliliter or more, it was considered positive. To identify the type of bacteria, the colonies were sampled and diluted with a drop of saline. Smear was prepared from the obtained liquid. After drying, the Smear was fixed with a gentle flame heat. The slides were Gram-stained and checked under a microscope. The data were analyzed using SPSS version 21 via independent t-test, chi-square test, and Fisher’s exact test at a significance level of less than 0.05.
4. Results
A total of 70 people entered the study. During the study, 10 people were excluded for various reasons, and finally, 60 participants completed it (Figure 1).
The results of statistical tests showed that the two groups did not have a statistically significant difference in terms of variables such as age, marital status, level of education, cause of hospitalization, antibiotic use, underlying diseases, amount of intake of fluids, and urinary output (Table 1).
| Variable | Chlorhexidine Group | Normal Saline Group | P Value |
|---|---|---|---|
| Age | 40.17 ± 11.52 | 38.71 ± 13.38 | 0.627b |
| Intake of fluids | 672 ± 3632 | 633 ± 3385 | 0.22b |
| Urinary excretion | 583 ± 3298 | 3164 ± 672 | 0.37b |
| Level of education | 0.08c | ||
| Illiteracy or elementary | 17 (56.6) | 20 (66.6) | |
| Middle or high school | 6 (20) | 9 (30) | |
| University | 7 (23.4) | 1 (3.4) | |
| The cause of hospitalization | 1c | ||
| Trauma | 17 (56.6) | 17 (56.6) | |
| Other | 13 (43.4) | 13 (43.4) | |
| Underlying diseases | 0.36c | ||
| Hypertension | 11(36.6) | 5 (16.7) | |
| Kidney disorders | 1 (3.3) | 3 (10) | |
| Other diseases | 5 (16.7) | 5 (16.7) | |
| None | 13 (43.4) | 17 (56.6) |
aValues are expressed as No. (%) or mean ± SD.
bIndependent t-test.
cChi-square.
At the end of the seventh day after the intervention, the results showed that the incidence of urinary tract infection was significantly lower in the chlorhexidine group (13.3%) than in the normal saline group (76.7%) (P = 0.001) (Table 2). In terms of the type of bacteria grown, Escherichia coli (43.3%) had the highest prevalence in the normal saline group while Staphylococcus epidermis (13.3%) had the highest prevalence in the chlorhexidine group. Other pathogens that grew in the normal saline group included Staphylococcus epidermis (16.7%), Enterobacter (13.3%), and Klebsiella (3.4%), but no other pathogens grew in the chlorhexidine group.
| Group | The Second Culture | ||
|---|---|---|---|
| Normal Saline | Test Result | Chlorhexidine | |
| Negative | 7 (23.3) | P = 0.001 | 26 (86.7) |
| Positive | 23 (76.7) | 4 (13.3) | |
| Total | 30 (100) | 30 (100) | |
aValues are expressed as No. (%).
bFisher’s exact test.
5. Discussion
This study aimed to compare the effect of perineal care with normal saline solution and chlorhexidine solution 2% on the rate of CAUTIs in women hospitalized in ICUs. The results showed that the incidence of UTI was significantly lower in the chlorhexidine group than in the normal saline group on the seventh day. Other studies have reported similar results.
Azadmanesh et al. (35) conducted a study to compare the effect of washing the meatus with chlorhexidine and povidone-iodine solutions on bacteriuria in patients with brain stroke. The patients had an indwelling urinary catheter and were hospitalized in a neuro-internal ward. In this study, the patient’s meatus area was washed with chlorhexidine 2% in the first group, while the washing was carried out with povidone-iodine for the second group and normal saline for the control group. Cleansing lasted five minutes each day and continued at most for 10 days. Finally, the results of the study showed that compared to normal saline, chlorhexidine and povidone-iodine used for washing the meatus area of hospitalized patients who were expected to have Foley catheter for more than five days led to the further reduction in the rate of UTI (35). In a clinical trial, Vahabi et al. (36) investigated the effect of cleaning the perineal area with 10% povidone-iodine and 2% chlorhexidine on bacteriuria and pyuria in hospitalized women before fixing indwelling urinary catheters. It was concluded that immediately three and five days after catheterization, no significant difference in bacterial growth was observed between betadine and chlorhexidine, but the rate of pyuria (the presence of pus in the urine) was significantly higher in the povidone-iodine group than in the chlorhexidine group (36).
Mohammadnia et al. (37) compared the effect of washing the perineal area with normal saline solution, povidone-iodine 10%, and chlorhexidine 0.2% on the incidence of bacteriuria and the type of microorganisms in patients admitted to ICUs. The results showed that on the fifth and seventh days, the incidence of bacteriuria in the three groups was significantly different. The researchers concluded that compared to betadine and normal saline, washing the perineal area and the initial part of the urinary catheter with 0.2% chlorhexidine solution reduced the incidence of bacteriuria in the first week of catheterization (37). Comparing the effect of bladder irrigation with 0.2% chlorhexidine solution and sodium chloride on preventing bacterial infection in patients with persistent urinary catheter, Samimi et al. (32) found that the irrigation of the bladder with chlorhexidine 0.2% reduced the incidence of CAUTIs compared to the normal saline solution in the first nine days of catheterization.
Huang et al. (38) conducted a study to assess “the effect of decolonization on bacteriuria and candiduria in patients admitted to ICUs” in the United States. The intervention included cleansing the perineal area and the proximal 15 cm of the urinary catheter with chlorhexidine. The findings showed that preventing the colonization of hospitalized patients in ICUs with chlorhexidine baths once a day along with mupirocin could be a potential preventive strategy for male patients, as it significantly decreased candiduria and bacteriuria (38). Also, Wikstrom et al. (39) aimed to assess the effect of bladder irrigation with chlorhexidine on reducing the incidence of bacteriuria in patients with spinal cord injury. They investigated 50 patients from two populations of hospitalized patients and patients living at home by random sampling from four rehabilitation centers in Sudan. The intervention was the irrigation of the bladder with chlorhexidine twice a day, in the morning and in the evening. The solution was kept in the bladder for 15 min and then drained. The urine samples were taken for the first urine culture three hours after irrigation. The results showed that irrigating the bladder with chlorhexidine alternately decreased bacteriuria in the majority of the patients with spinal cord injury (39).
Compared to our findings, some studies have reported differently. Jeong et al. (18) compared the effects of four different agents on the incidence of CAUTIs. They used soap and water in the first group, skin cleansing foams in the second group, povidone-iodine 10% in the third group, and normal saline in the fourth group. The results showed that the type of perineal care did not affect the incidence of CAUTIs. For further confirmation, they suggested that the study be conducted on a larger patient population to determine the preferred factor for perineal care (18). However, the study did not use chlorhexidine.
In a study entitled “does the instillation of chlorhexidine into the bladder of catheterized geriatric patients help reduce bacteriuria?”, Davies et al. (40) investigated the irrigation of the bladder with 100 cc of normal saline or 0.2% chlorhexidine solution twice a day for three weeks. The fluid was discharged in an hour. The results showed that the rate of bacteriuria was the same in the two groups of normal saline and chlorhexidine (40). The results of their research are not consistent with the present study findings. The difference can be attributed to inconsistency between the participating samples and the methods of work. The study involved people over the age of 60 who lived in nursing homes and who had a closed urinary catheterization system opened twice a day for chlorhexidine or normal saline injection. Opening the urinary tract system may increase the chance of entering bacteria to the bladder, and is contrary to scientific protocols for perineal care. The type of perineal care was also not mentioned in this study.
5.1. Conclusions
The findings of the study showed that perineal care with 2% chlorhexidine solution, as compared to normal saline, significantly reduces CAUTIs among women admitted to intensive care units. Antiseptic chlorhexidine enjoys unique properties such as a high level of antimicrobial activity and a strong tendency to bind to the skin and mucous membranes. Also, the application of this solution is simple, safe, and cost-effective. Therefore, it is recommended that more extensive studies be performed to prevent and reduce the incidence of catheter-associated urinary tract infections (CAUTIs) in patients admitted to Intensive Care units.