1. Background
Oral health is a major branch of public health that has a great impact on people’s overall health (1). According to the World Health Organization, oral health refers to the health of the mouth and related organs, enabling people to eat, speak, and socialize without difficulties and embarrassments and contributing to their overall health (2). Oral health goes beyond having healthy teeth and is an integral part of general health so that the mouth is a mirror that reflects one’s overall health (1).
Patients admitted to Intensive Care units (ICUs) develop oral problems rapidly for a variety of reasons, including endotracheal intubation, malnutrition, and fluid loss due to fever, diarrhea, and decreased fluid intake (3). The mouth’s natural flora contains 350 types of bacteria, mainly including Gram-positive streptococci and a variety of viruses and fungi, with different species tending to accumulate in different parts of the oral cavity (4). Within 48 hours of admission to an ICU, the mouth’s natural flora changes in favor of gram-negative organisms that have greater pathogenicity (5). These changes cause bacteria to accumulate and proliferate opportunistic pathogens in the oral cavity, causing local and general complications such as stomatitis, tooth decay, peripheral tissue infection, and the subsequent systemic spread of infection, bacteremia, respiratory infections, such as pneumonia, and even infection of the joints and heart (6). Patients in ICUs are more prone to dental plaque and oral lesions due to immunosuppression, underlying diseases, endotracheal and gastric tubes, medication side effects, decreased fluid intake, lack of spontaneous tongue movements, and lack of swallowing (7).
However, ICU patients are often unable to perform oral hygiene procedures such as brushing their teeth. Therefore, they are completely dependent on nurses for oral health needs. It is generally accepted that "good and frequent oral care" is more important for these patients and can be provided by several separate or combined methods such as mouthwash, gel use, toothbrush, and secretion suction (8). Safarabadi et al. (9) quotes Grap and Munro that oral health and care should be considered as one of the most significant components of nursing care.
There are two main ways to take care of the mouth and remove dental plaque and oral microbes, including “mechanical intervention” and “pharmacological intervention” (10). Brushing is considered as a mechanical intervention and a major method to remove plaque as a potential source of infection in ICU patients. During the hospitalization period, using toothbrushes for oral care is less considered by the nursing staff than other measures (11). Pharmacological procedures also include the removal of plaque and microorganisms using bactericidal agents. Moreover, research has revealed the effect of topical antibiotics on rinsing and oral care, although they are not used due to microbial resistance (12). Chlorhexidine is a detergent that acts on a wide range of microorganisms (13), and so far, no microbial resistance and carcinogenic effects have been reported for it (14). Chlorhexidine is an oral disinfectant solution that reduces the amount of dental plaque and is preferred in patients under mechanical ventilation (15).
Oral care is vital for patients admitted to ICUs and can have a significant impact on clinical outcomes and these patients’ health. It decreases the microbial colonization and aspiration of infected saliva (16). However, research has shown that there is no specific protocol for how to do it, how often and what equipment is needed, and nurses use different methods and tools depending on, depending on their experiences or commonly used methods inwards (12).
On the other hand, the evidence is limited on the effect of a combination of different oral care methods on oral health. Due to this limitation and the discrepancy of the results, further research is recommended on the combined effects of different oral care aspects compared to routine methods (17).
2. Objectives
Therefore, considering the above-mentioned issues and the fact that nurses do not currently perform oral care in ICUs in a uniform and regular manner, the present study was conducted to compare the effects of a comprehensive oral care program and a combined toothbrush and mouthwash program with chlorhexidine 0.2% on oral health in patients under mechanical ventilation admitted to ICUs.
3. Methods
This single-blind clinical trial was carried out on 90 patients (in three groups) with mechanical ventilation admitted to ICUs of medical centers affiliated to the Zahedan University of Medical Sciences in 2020. The sample size was calculated to be 12.8 for each group based on Seguin et al.’s study results (18), with a 95% confidence level and 90% statistical power. Since there were three groups in the study, the number of participants in each group was multiplied by 1.4, and 18 people were calculated in each group. However, we considered 30 people in each group and a total of 90 people in the three groups to ensure the adequacy of the sample size. The patients were selected using convenience sampling. Then, they were randomly allocated to three groups, with those receiving a comprehensive oral care program, those receiving a combined program of toothbrush and mouthwash, and controls using permutation blocks based on the inclusion criteria. Written consent was obtained from the patients’ legal guardians. Since three groups were considered in the study, the patients were assigned to 15 cases of six blocks: the group A receiving the comprehensive oral care program, the group B receiving toothbrush and mouthwash with 0.2% chlorhexidine, and the group C as controls (e.g., AABBCC, ABABCC, and BBAACC). There were two people in each block from each group. The order of the blocks was determined randomly using a random number table, and then, the patients were included in the comprehensive care program group, the combined program of toothbrush and mouthwash with 0.2% chlorhexidine group, and the control group based on the blocks. One of the researchers with no role in data collection performed a random block assignment sequence. The researcher performing the oral health assessment had no knowledge of patients in the study groups to observe blindness.
The inclusion criteria were 18 - 65 years of age, the second day of intubation, no severe facial and oral injury, no chronic disease and immune deficiency, no removable dentures, no pregnancy, and normal coagulation status. The exclusion criteria included performing a tracheostomy procedure during the study, discharge from the ward, sensitivity to chlorhexidine, legal guardian’s unwillingness to continue the study, and patient’s death.
Data collection tools included a demographic information form (age, gender, marital status, education, and disease-related variables including history of ICU admission, underlying disease, endotracheal suction frequency, level of consciousness based on GCS, and smoking history) and the Beck Oral Assessment scale (BOAS). This scale has five subscales (evaluation of lips, mucous membranes and gums, teeth, tongue, and saliva), and it is scored based on a 4-point Likert scale, with its overall score being between 5 - 20. The highest score on the scale indicates the most severe disorder. Thus, a score of 5 means no disorder, 6 - 10 means a mild disorder, 11 - 15 means a moderate disorder, and 16 - 20 means a severe disorder. Safarabadi et al. (9) confirmed the scale’s validity and reliability using the test-retest method with a Pearson correlation coefficient of 0.92. In the present study, the scale’s reliability was confirmed using the inter-rater reliability method with a coefficient of 0.93. The oral health status of patients in all three groups was assessed and recorded by BOAS before the intervention.
In the two groups of the comprehensive oral care program and the combined program of toothbrush and chlorhexidine, the intervention started from the second day of hospitalization and continued for five consecutive days. In the control group, routine care was performed by nurses as mouthwash with chlorhexidine solution. The frequency of oral care in the intervention groups was determined based on the score obtained from BOAS. In patients without disorder, oral care was done every 12 hours. Also, oral care was performed in mild disorder every 8 hours, in moderate disorder every 6 hours, and in severe disorder every 4 hours (19). Due to the fact that the oral health assessment scores in the groups before the intervention were in the mild range, oral care was performed for patients in both intervention groups for five consecutive days, once every 8 hours and each time for 5 minutes.
The intervention in the comprehensive oral care program group was executed by reviewing previous studies and performing the following measures for 5 minutes: washing hands and wearing gloves, controlling the cuff pressure of endotracheal tube less than 25 mmHg, raising the head of the bed by 30 to 45 degrees, brushing the inner and outer surfaces of the teeth, gums, and tongue for 2 minutes using a baby toothbrush and toothpaste with rotating movements, deep throat and mouth suction for 30 seconds while 0.9% normal saline was poured into the patient’s mouth and teeth, rinsing the mouth with 0.2% chlorhexidine antibacterial solution with a swab, moistening all surfaces of the patient’s oral mucosa, gums, and tongue using a swab and distilled water, and using vitamins A-D to lubricate the lips. If there is an oral pharyngeal airway, it is removed, cleaned, and re-placed in the patient’s mouth (12, 19, 20).
In the intervention group with the combined program of toothbrush and mouthwash with chlorhexidine 0.2%, oral care was performed during the 5 days of the study, each time for 5 minutes. The intervention in this group was performed by gently brushing all the outer and inner surfaces of the teeth and gums and then the tongue and palate surfaces with a baby toothbrush and antimicrobial toothpaste containing fluoride by making rotating movements or moving from the back to the front of the mouth. After brushing, each part of the mouth was cleaned with sterile distilled water. The mouth, tongue, and teeth were then rinsed with a chlorhexidine-soaked swab. The control group received routine oral care, including mouthwash with chlorhexidine 0.2%, which was performed by nurses. In addition to measuring oral health before the intervention, it was measured and recorded during the 5 days of the study in patients of all the three groups with the help of an uninformed researcher to the groups in the morning shift. IBM SPSS Statistics software version 26 was used for data analysis. Descriptive statistics (frequency distribution tables, mean, and standard deviation) were used to describe the data, and analysis of variance was used to examine the mean of quantitative variables in the study groups. Also, the chi-square test was used to examine the relationship between the variables, and analysis of variance was used to evaluate underlying variables in the groups for quantitative variables. Moreover, the Shapiro-Wilk test was used to evaluate the data normality. The significance level in the present study was considered less than 0.05.
4. Results
The Shapiro-Wilk test results showed that the research data had a normal distribution. Thus, parametric tests were used to analyze the data.
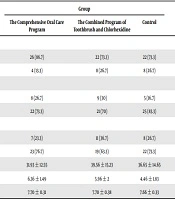
The analysis of variance test results showed no significant difference between the three groups regarding the mean of the quantitate variables, such as age, the GCS score, and endotracheal tube size (P > 0.05). Similarly, the chi-square test results showed no significant difference between the three groups in terms of gender, smoking, and underlying disease (P > 0.05) (Table 1).
| Variable | Group | P | ||
|---|---|---|---|---|
| The Comprehensive Oral Care Program | The Combined Program of Toothbrush and Chlorhexidine | Control | ||
| Gender | 0.35b | |||
| Male | 26 (86.7) | 22 (73.3) | 22 (73.3) | |
| Female | 4 (13.3) | 8 (26.7) | 8 (26.7) | |
| Smoking | 0.45b | |||
| Yes | 8 (26.7) | 9 (30) | 5 (16.7) | |
| No | 22 (73.3) | 21 (70) | 25 (83.3) | |
| Underlying disease | 0.49b | |||
| Yes | 7 (23.3) | 11 (36.7) | 8 (26.7) | |
| No | 23 (76.7) | 19 (63.3) | 22 (73.3) | |
| Age | 31.93 ± 12.55 | 39.56 ± 15.23 | 36.65 ± 14.65 | 0.11c |
| GCS score | 6.36 ± 1.49 | 5.96 ± 2 | 4.46 ± 1.83 | 0.52c |
| Endotracheal tube size, mm | 7.70 ± 0.31 | 7.70 ± 0.38 | 7.66 ± 0.33 | 0.91c |
aValues are expressed as mean ± SD or No. (%).
bChi-square.
cAnalysis of variance.
The mean oral health score on the first day of the study was 6.63 ± 0.96 in the comprehensive oral care program group, 6.5 ± 0.77 in the combined toothbrush and chlorhexidine program group, and 6.13 ± 0.77 in the control group. The ANOVA test results showed that the mean oral health score was not significantly different between the three groups on the first day of the study and before the intervention (P = 0.065) (Table 2). On the second day of the study, the score was 6.33 ± 0.66 in the comprehensive oral care program group, 6.33 ± 0.66 in the combined program group, and 6.23 ± 0.67 in the control group, which was not significantly different between the three groups (P = 0.799) (Table 2). The score on the third day of the study, was 5.53 ± 0.68 in the comprehensive oral care program group, 5.83 ± 0.79 in the combined toothbrush and chlorhexidine program group, and 7.03 ± 0.76 in the control group, which was significantly different between the three groups according to the ANOVA test results (P = 0.001). On the fourth day of the study, the score was 5.13 ± 0.34 in the comprehensive oral care program group, 5.23 ± 0.43 in the combined toothbrush and chlorhexidine group, and 7.40 ± 0.85 in the control group. According to the ANOVA test results, it was significantly different between the three groups (P = 0.001). The score on the fifth day of the study was 5.00 ± 00 in the comprehensive oral care program group, 5.16 ± .37 in the combined program group, and 7.76 ± 0.81 in the control group, which was significantly different between the three groups according to the ANOVA there results (P = 0.001) (Table 2).
| Day | Group | Pb | ||
|---|---|---|---|---|
| The Comprehensive Oral Care Program | The Combined Program of Toothbrush and Chlorhexidine | Control | ||
| Before the intervention | 6.63 ± 0.96 | 6.50 ± 0.77 | 6.13 ± 0.77 | 0.065 |
| The second day | 6.33 ± 0.66 | 6.33 ± 0.66 | 6.23 ± 0.67 | 0.799 |
| The third day | 5.53 ± 0.68 | 5.83 ± 0.79 | 7.03 ± 0.76 | 0.001 |
| The fourth day | 5.13 ± 0.34 | 5.23 ± 0.43 | 7.40 ± 0.85 | 0.001 |
| The fifth day | 5.00 ± 00 | 5.16 ± 0.37 | 7.76 ± 0.81 | 0.001 |
aValues are expressed as mean ± SD.
bAnalysis of variance.
5. Discussion
The current study aimed to compare the effects of a comprehensive oral care program and a combined program of toothbrush and chlorhexidine 0.2% on oral health in patients admitted to ICUs. The results showed the positive effects of the comprehensive oral care program and the combined toothbrush and chlorhexidine program on oral health in patients under mechanical ventilation. Accordingly, the oral health score of patients in the two intervention groups decreased during the study period, indicating an improvement in oral health. However, in the control group receiving routine care, including mouthwash with chlorhexidine 0.2%, the oral health score increased during the study period, confirming a worsening of the oral health status in this group. These results indicate that implementing comprehensive oral care programs and having a regular schedule to use mechanical and pharmacological methods for oral care, if implemented regularly and codified, can improve oral health in patients under mechanical ventilation.
Consistent with the present study’s results, Ames et al. (19) showed that oral health improved in patients after implementing a systematic oral care protocol. Also, Atashi et al. (3) showed a significant effect of a comprehensive oral care program on oral health in ICU patients.
Haghighi et al. (21), in their study, showed that regular oral care programs, brushing, oral suction with normal saline, rinsing the mouth with chlorhexidine, and moisturizing the oral mucosa with vitamin A-D significantly improved oral health in ICU patients. The similarity of Atashi et al. (3) and Haghighi et al.’s study (21) with the current study was in the type of intervention; both studies used a comprehensive care plan with the mentioned components, although the present study compared the comprehensive plan with a combined brush and chlorhexidine program. The results of the above studies are in line with those of the present study, emphasizing the major role of comprehensive care programs in improving intubated patients’ oral health and the significance of using combined methods in oral care.
Ildarabadi et al. (22) also reported the positive effect of using an oral care program on oral health in the elderly living in nursing homes. Although the sample and tools in Ildarabadi et al.’s study (22) were different from those in the present study, the consistent results of both studies showed the effectiveness of using a regular and codified program for oral care and its impact on oral health in patients.
In the present study, chlorhexidine was used as part of an oral care program. The use of chlorhexidine as a gold standard antiseptic has a wide range of antibacterial, antiviral, and antifungal effects (23). In the present study, oral health was improved in both groups of the comprehensive oral care program and the combined toothbrush and chlorhexidine program, but the difference was not significant between the two groups. Moreover, the mean oral health score during the five days of the study had a greater decrease in the comprehensive oral care program group than in the combined toothbrush and chlorhexidine program group. This finding indicates that a comprehensive oral care program can provide a clinically greater improvement than a combined toothbrush and chlorhexidine program in oral health in ICU patients, which appears logical considering the more components of this program.
Beraldo and Andrade (24) showed that brushing, when combined with chlorhexidine, was more effective in maintaining oral health in patients admitted to ICUs. The intervention in Beraldo and Andrade’s study (24) is similar to the combined program in the current study. Despite the importance of using combination methods, DeKeyser Ganz et al. (11) reported that only 34 percent of nurses used toothbrushes along with other oral care methods for intensive care patients. The use of a baby toothbrush, which was also used in the present study, has benefits, such as easy and good access to intubated patients’ oral cavity, which is almost closed, and also causes less damage and discomfort to be fragile and vulnerable tissues (25). Griffith et al. recommended the use of a small soft toothbrush to remove plaque in patients admitted to ICUs because of the possibility of brushing the back of the mouth, as well as cleaning the tongue, gums, and teeth, as quoted by Estaji et al. (7).
In their study, Kaya et al. (26) showed that the use of chlorhexidine mouthwash alone improved oral health. Inconsistent with the present study’s results, Anggraen et al. (27) showed that the oral care program had a deteriorating effect on oral health in intubated patients during the study period. Also, the results of Prendergast’s study (28) are inconsistent with the present study’s results. The reason for the discrepancy between the results of recent studies and the present study might be the type of intervention. Anggraen et al. (27) used chlorhexidine, and Prendergast used fluoride toothpaste for oral care. Another reason for the difference between the studies’ results is probably the small sample size. Anggraen et al. (27) studied one group of 18 people, while Prendergast studied two groups of 25 and 31 people.
Contrary to the above studies’ results, some studies confirmed the positive effect of mechanical methods on oral health status. Alone compared to pharmacological methods. For example, Estaji et al. (7) showed that using toothbrushes and chlorhexidine was effective in preventing oral lesions. However, they reported that using toothbrushes compared to chlorhexidine led to better improvement of the patient’s oral health and had a significant effect on reducing oral lesions (7).
In general, according to the reviewed studies and the present study, it can be mentioned that the implementation of a regular and codified program, as either a combination of mechanical and pharmacological methods or a comprehensive program that considers all aspects of oral care, has a positive effect on oral health in intubated patients under mechanical ventilation. The way the nurses performed routine care in the control group can be one of the present study’s limitations because we could not control the nurses’ performance and confirm that all the patients received the same care.
5.1. Conclusions
Overall, according to the present study’s findings, it can be concluded that both the comprehensive oral care program and the combined toothbrush and chlorhexidine program are effective in improving oral health in intubated patients admitted to ICUs. The comprehensive oral care program is simple and practical and can be used as a suitable care method by nursing staff to provide oral health in patients under mechanical ventilation admitted to ICUs.