1. Background
The survival rate of premature infants has soared thanks to the advancement of science and technology in the early detection of complications and their timely treatment (1-4). In parallel with the increased survival of premature and low birth weight infants, the rates of developmental disabilities, cognitive impairments, and sensorineural problems are also on the rise in these babies. Adverse effects, such as cerebral palsy and behavioral problems in premature infants are considered to be one of the biggest socio-economic issues (4, 5). Numerous studies have linked these problems to the effects of the environment on the central nervous system of these infants (6). Most preterm babies, especially those with very low birth weight, have to stay in a Neonatal Intensive Care Unit (NICU) for weeks or months due to various problems related to respiration, nutrition, temperature, jaundice, and other disorders (7). In addition to environmental stressors, many clinical factors, including chronic pulmonary disease, apnea, recurrent bradycardia, jaundice, nutritional problems, impaired heart rate, skin discoloration, hypoxia, decreased arterial oxygen saturation, apnea attacks, increased need for mechanical ventilation, abnormal sensory development, loss of hearing and vision, speech problems, irritability and crying, nutritional intolerance, and delayed weight gain in the baby can increase the length and cost of hospitalization (8, 9).
Another important issue in these infants is their nutrition. Breastfeeding satisfies the nutritional needs of premature infants and facilitates their expected development (10). Oral nutrition is a golden standard for discharging a premature baby from the NICU, and breastfeeding has fewer challenges for premature infants. However, most of these infants are fed formula milk, and achieving full oral nutrition in this population remains a challenge (11). This issue could be resolved when there are behaviors in the infant to start oral nutrition and coordinate sucking, swallowing, and breathing. The lack of oral feeding skills is associated with long-term hospitalization, increased health care, and higher costs. The onset of nutrition in premature infants is affected by the development of the nervous system; thus, as brain cells are myelinated, from the 35th week, the baby can do fine coordinated oral movements (12). Nutritional adequacy reflects the infant’s nutritional skills, which are vital to the success of oral feeding and the maintenance of the infant’s physiological stability (11).
The smell of breast milk is one of the stimuli that trigger sucking, which, in turn, stimulates the trigeminal and facial nerves in the medulla oblongata and strengthens this innate behavior (13, 14). One of the objectives of therapy in NICUs is to enhance the nutritional skills of these infants. Frequent exercises and interventions aimed at improving oral motor skills are very effective in this regard due to the high learning capabilities of preterm infants. Aromatherapy refers to the application of aromatic oils to promote physical and mental health and the general sense of well-being and quality of life. It is a complementary treatment that is increasingly gaining popularity as a therapeutic method in nursing care (15). Neonates have a strong and evolved sense of smell and, unlike what is the case for other senses, they show valid behavioral and physiological responses to olfactory stimuli in the face of desirable and unpleasant odors. Taking advantage of the sense of smell and its stimulation for the growth and development of premature infants are important nursing measures in the NICU that can increase weight gain and reduce both energy consumption and the length of hospitalization (16).
Premature infants in modern NICU are often exposed to stress caused by painful procedures and high levels of ambient light and noise. Excessive light in the unit reduces visual activity and impairs attention, visual memory, and recognition. Better respiratory stability and reduction of heart rate, respiratory distress, motor activity, and ventilation time are some of the benefits of reducing light in the NICU (17). On the other hand, reduced lighting increases the infant’s sleep time and weight gain. Therefore, all medical and nursing care should be performed in an environment analogous to the uterus, and the light in the unit should be set between 101 - 600 lux, but maximum light in the UNIC is usually 646 lux (9). As a result, to reduce the negative impact of these stimuli, researchers have proposed a wide range of interventions to mitigate noise and lighting (18). The best way to reduce direct light is to use an incubator cover or apply pads over the baby’s eyes (19).
In a longitudinal study, 214 neonatal units in the UK were surveyed between 2005 and 2008 for developmental care activities, and the results suggested that the administered light and sound was decreased by up to 80% and incubator cover use was increased (20). Reyhani et al. (21) investigated the effect of incubator cover on physical parameters and observed its effectiveness in creating a suitable environment to help these infants grow better and curb the effects of premature birth. There is a relatively small body of literature that has assessed the effect of breast milk odor and incubator cover on nutritional adequacy and physiological parameters.
2. Objectives
The purpose of this study was to determine the effect of breast milk odor and incubator cover on nutritional adequacy and oxygen saturation of premature infants admitted to the NICU of Ali Ibn Abi Taleb Hospital in Zahedan in 2018.
3. Methods
Following the approval of the Ethics Committee of Zahedan University of Medical Sciences (code: IR.ZAUMS.REC.1397.437), a quasi-experimental study was performed in 2018 at Ali Ibn Abi Taleb Hospital in Zahedan. A total of 105 infants admitted to the NICU were selected based on the inclusion criteria and were randomly assigned to three groups of 35 members: Incubator cover (IC), breast milk odor (BMO), and control. Three cards marked with letters A, B, and C were used on which words BMO, IC, and control had been written. Then, they were selected by some nurses to determine the group of each infant. The eligibility criteria included a gestational age of 30 - 34 weeks, birth weight of 1,500 - 2,200 g, 5-min APGAR (appearance, pulse, grimace, activity, and respiration) score above 6, no congenital anomalies, no head and face abnormalities, oral feeding, and no asphyxia. The exclusion criteria, on the other hand, were infant’s death, exacerbation of neonatal problems, the occurrence of other acute illnesses, and the unwillingness of the infant’s parents to continue the study.
The sample size was estimated at 18 for each group based on a study by Kucuk et al. at a confidence interval of 95% and a statistical power of 95%. To account for possible attrition, we finally allocated 35 infants to each of the three groups.
The instruments used in this study included a form for collecting personal and clinical information (gestational age, birth weight, gender, APGAR score, and height) and the volume of breast milk intake. To assess nutritional adequacy, the prescribed amount of breast milk was poured into the syringe (Supa Co.) and then orally fed to the infant. The amount of milk taken in the first 10 minutes was noted, and the process was video-recorded (11).
The first group (A) was exposed to breast milk smell. First, the fresh breast milk of mothers was prepared at 8:15 AM. Next, 1.5 mL of milk was placed on a small (4 cm) gauze in an incubator at a distance of 1.5 cm from the baby’s nose for 15 min (from 8:45 to 9:00 AM). In the second group (B), a cover was placed on the incubator for two hours (from 7:00 to 9:00 AM). The cover was a dark-colored fabric, one side of which was dark, and the other side was light; it was open in the middle so that the baby’s skin color could be seen and evaluated. All three groups were provided with standard care, including the reduction of light and noise, kangaroo mother care, and the presence of parents in the unit. At 9:00 AM, for all the three groups, the same amount of milk was poured into a syringe (Supa Co.) to orally feed the infants for 10 min. It should be mentioned that the best duration to measure oral feeding is 10 min, after which the baby gets tired.
Nutritional adequacy in the context of the present study refers to the amount of milk, calculated in milliliters per minute (mL/min), that a baby is fed during the first 10 minutes of feeding. This process was video-recorded. The recordings were reviewed and evaluated by two researchers after the intervention. Data were analyzed in SPSS-22 using the chi-square test, independent t-test, and paired t-test at a significance level of P < 0.05.
4. Results
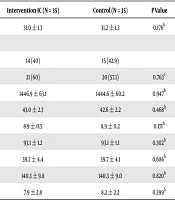
Initially, to ensure the normal distribution of quantitative variables, we used the Kolmogorov-Smirnov test and the Shapiro-Wilk test. Depending on the normal or abnormal distribution of these variables, we used the appropriate parametric or non-parametric tests to match the three groups in terms of background and confounding variables (Table 1). The results exhibited that the height of infants in all the three groups and infants’ respiration rate in the BMO group had normal distributions, but other quantitative variables did not have a normal distribution in the three groups. Based on the results of the one-way Analysis of Variance (ANOVA), there was a statistically significant difference in the mean scores of nutritional adequacy between the three groups after the interventions (P < 0.001). In this regard, Tukey’s post hoc test displayed significant differences between the BMO and control groups (P = 0.001) and the IC and control groups (P < 0.001). Meanwhile, nutritional adequacy did not differ significantly between the two intervention groups (P = 0.102) (Table 2).
| Variable | Intervention-BMO (N = 35) | Intervention-IC (N = 35) | Control (N = 35) | P Value |
|---|---|---|---|---|
| Gestational age | 30.7 ± 1.2 | 31.0 ± 1.3 | 31.2 ± 1.3 | 0.176b |
| Gender | 0.763c | |||
| Female | 17 (48.6) | 14 (40) | 15 (42.9) | |
| Male | 18 (51.4) | 21 (60) | 20 (57.1) | |
| Weight | 1442.9 ± 71.5 | 1446.9 ± 63.1 | 1444.6 ± 60.2 | 0.947b |
| Height | 42.4 ± 2.6 | 43.0 ± 2.3 | 42.6 ± 2.2 | 0.468b |
| APGAR score | 9.1 ± 0.5 | 8.9 ± 0.5 | 8.9 ± 0.2 | 0.171b |
| O2 saturation | 93.5 ± 1.5 | 93.1 ± 1.2 | 93.1 ± 1.1 | 0.302b |
| Respiratory rate | 39.4 ± 4.5 | 39.2 ± 4.4 | 39.7 ± 4.1 | 0.686b |
| Heart rate | 3139.8 ± 8 | 140.3 ± 9.8 | 140.3 ± 9.0 | 0.820b |
| Nutrition rate | 37.2 ± 2 | 7.9 ± 2.8 | 8.2 ± 2.2 | 0.399b |
aValues are expressed as No. (%) or mean ± SD.
bANOVA.
cChi-square test.
5. Discussion
The results of the current study showed an improvement in the nutrition of premature infants in the two intervention groups. Similarly, Beker et al. (22) explored the impact of breast milk odor on promoting the nutrition of premature infants and observed that the intervention group began oral feeding and experienced total oral feeding earlier than did the control group. In another study, Diosun et al. (23) examined the effect of stimulation with breast milk odor on time required for passing through gavage to oral nutrition, and the results suggested that this intervention could accelerate oral nutrition. Chailangka et al. (24) found that expressed breastmilk on the lips during application of the premature infant oral motor intervention (PIOMI) versus PIOMI alone improved feeding efficiency. Aoyama et al. (4) reported that breast milk odor, compared to the smell of formula milk, boosted oxygen in the frontal orbital region and had a greater effect on the oxygenation of brain tissues. Munakata et al. (25) conducted a study on olfactory stimulation and its association with total parenteral nutrition (TPN) and the duration of using a gastric tube.
The above studies confirm that the smell of breast milk plays an important role in the oral feeding of premature infants. The receptors of the gastrointestinal tract and olfactory perception are formed and developed at 18 and 24 weeks of gestation, respectively, such that the infant’s neural system responds to the smell of amniotic fluid. In premature infants, like other humans, the odor has a major role in the physiological responses of the body. Aromatic stimulation before feeding triggers peristaltic movements and the secretion of gastric enzymes and gastrointestinal hormones (2, 19, 21, 26, 27). When the breast milk smell reaches the baby’s nose, the salivary glands (amylase and lipase) begin to secrete, which, in turn, leads to secretions from gastrointestinal glands, making it easier and more pleasing for the baby to suck. In this study, the infants were monitored while being fed with a syringe, which did not cause any disturbance in their respiratory rate, heart rate, and the percentage of oxygen saturation.
Regarding incubator cover, Reyhani et al. (21) found that the creation of artificial night has a positive impact on stabilizing the physiological status of premature infants and providing them with a salutary environment. It improves the growth of these infants and prevents the adverse effects of incubator cover. Possible factors explaining the effect of incubator cover on the promotion of infants’ nutritional adequacy include attention to circadian rhythm and the improvement of infants’ sleep and wakefulness rhythm. This is because the standard light of the incubator cover helps regulate the secretion of both growth and stress hormones; this cover also mitigates oxygen saturation changes and ultimately helps regulate the baby’s metabolism and nutrition. The results of the present study support this suggestion (28).
Recently, Jane studied the effect of incubator cover on the sleep and wakefulness rhythm of premature infants two hours before oral feeding (29). It was found that infants that experienced a less deep sleep and shorter wakefulness showed less progress in acquiring oral feeding skills compared to the control group. In the present study, however, although the incubator cover was applied two hours before oral feeding (which led to a deeper sleep in the infants), placing a syringe containing breast milk near the mouth and nose of the infants helped to awaken them. Consequently, those infants exposed to this intervention orally received a higher amount of breast milk than did the control group. Nurses in the NICU generally underestimate the significance of deep sleep and conscious wakefulness for premature infants. In this regard, Mahmoodi et al. (30) reported that nurses were mostly unaware of infants’ sleep and circadian rhythm.
In the present study, a statistically significant difference occurred between the control group and the two intervention groups (incubator cover and breast milk odor). Also, the BMO group showed higher nutritional adequacy than did the control group. It can be concluded that both incubator cover and breast milk smell are effective in promoting the nutritional adequacy of preterm infants.
5.1. Conclusions
Considering that breast milk odor and incubator cover improved infants’ nutritional adequacy, it is suggested that this non-pharmacological nursing intervention be adopted as an effective measure by the healthcare system. Thanks to the proposed interventions, the infants received more milk through the mouth. Since one of the basic criteria for discharge from the hospital is the development of oral feeding skills in premature infants, speeding up this acquisition reduces hospital costs for both parents and the healthcare system. Besides, infants are, thus, enabled to enter the warm and intimate environment of their family where they undergo much less stress. Therefore, neonatal intensive care units can integrate this accessible, safe, and cost-effective intervention in their care programs. However, it is suggested that more studies be carried out in this area.