1. Background
Chronic kidney disease (CKD) includes a range of various pathological processes along with abnormal kidney function and a gradual reduction in glomerular filtration rate, whose last stage is End-Stage Renal Disease (ESRD) (1). In fact, ESRD is a kidney condition where about 90% of the kidney function is lost (2). The annual incidence of the disease is reported to be 53 cases per one million people (3). The prevalence of CKD is 8.66% in Africa, 13.10% in India, 13.74% in Japan, 14.71% in Australia, 15.45% in the USA, and 18.38% in Europe (4-6).
In case the kidney function reaches 10 to 15% of its normal function, alternative methods will be needed (7). Hemodialysis is one of the most successful alternative therapies for kidney function (3, 8). The purpose of hemodialysis is to remove waste products, stabilize the internal environment of the body, and remove toxins to prevent permanent injury or death (9-11). There are more than 13,000 dialysis patients in Iran, and about 150,000 dialysis sessions are held every month to treat these patients. The number of patients undergoing hemodialysis increases by about 15% annually (12). Cardiovascular diseases and inadequacy of dialysis are the main determinants of disability and mortality in dialysis patients (3, 4).
Inadequate dialysis can increase the disease complications, duration of hospitalization, and the costs incurred on the patients (13, 14). Hence, dialysis adequacy affects the long-term prognosis of chronic hemodialysis patients, and its evaluation and enhancement are extremely important in reducing mortality in dialysis patients (15, 16)
If dialysis adequacy is better, the complications of uremia on various organs of the body will be less, and mortality will reduce (17, 18). About 11% of patients do not meet the minimum standard of dialysis adequacy (19). Increasing the efficiency of dialysis adequacy is of great significance as it can enhance health and increase life expectancy (20, 21).
Presently, the most reliable method of measuring and evaluating dialysis adequacy is the Kt/V, K is filterability to purify urea, T is the duration of hemodialysis, V the volume of urea distribution in body fluids. According to the American Association of Kidney Patients, 1.2 < Kt/V shows hemodialysis adequacy (19, 20).
Urea reduction ratio (URR) is another method for measuring the dialysis adequacy. This method is expressed as a percentage (22). In the studies conducted so far, the standard value of Kt/V in patients undergoing dialysis three times a week has been determined to be 1.2, below which the number of uremic complications increases (23). Previous studies have reported a 0.7 reduction in mortality per 0.1 increase in Kt/V and an 11% decrease in mortality per 5% increase in URR (24). The results of a study by the Dallas Dialysis Center show that with an increase in Kt/V from 1.18 to 1.46, the mortality rate decreased from 22.5 to 18% (25).
Different elements like the ability of the filter to remove and transport waste products, the duration of dialysis sessions, and the rate of blood flow and dialysis fluid have a significant role in achieving effective and efficient dialysis (26). Despite this increase in the dialysis time, for economic reasons and patient intolerance are not always possible. Moreover, the increase in the dialysis flow rate is not practical given the difficulty in achieving the appropriate speed and imposing complications and consequent patient intolerance for a long time (26, 27). Thus, other parameters affecting the quality of dialysis, like the ability of the filter membrane, should be considered; however, obstruction of the pores of fine filters by different materials, like small clots formed during hemodialysis, could hinder reaching effective and efficient dialysis (26). Clot formation during dialysis is a common and unavoidable phenomenon. Owing to the turbulence of blood flow, high blood pressure, and contact of blood with artificial surfaces, the possibility of clot formation increases, and thus dialysis adequacy will decrease (28, 29).
A common mechanism for coping with this complication is using anticoagulants during hemodialysis (29). Heparin continues to be used as a preferred medicine by physicians (30, 31).
To prevent clots, heparin is used in different ways, such as using minimal heparin and heparin-free method with high serum flow (32). Low cost, easy administration, monitoring of the drug, and its short biological half-life have led to its widespread use during hemodialysis (33). The proper use of anticoagulants is of high importance in minimizing the risk of bleeding (34). The normal saline solution, hyperchloremic and hypertonic (with an osmolality of 309 mmol) such that it is recommended as the optimum solution in advanced renal patients (26, 35).
Various prime dialyzer approaches have a positive effect on increasing dialysis adequacy (36).
2. Objectives
As the device primer with heparin administration and normal saline administration with recirculation methods have both been effective. In this study, we decided to evaluate their effect on dialysis adequacy.
3. Methods
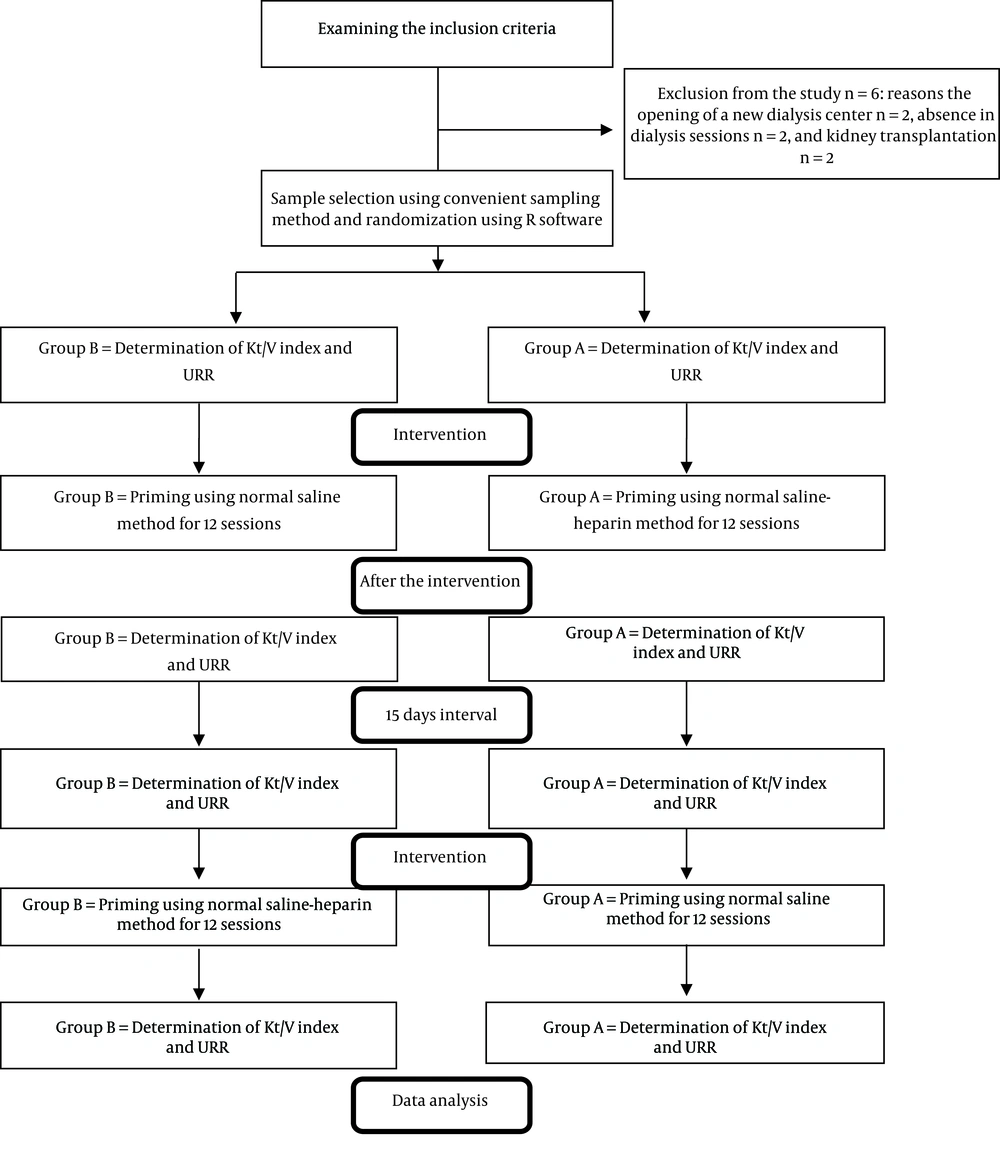
The purpose of this study was to determine the effect of normal saline-heparin prime on dialysis adequacy. The population was the patients undergoing hemodialysis admitted to the dialysis ward of educational and medical centers in Hamadan in the fall of 2019 Figure 1. The number of samples was estimated to be 36 people in each group (29). After selecting the samples, the patients were selected from all three shifts of morning, evening, and night using convenient sampling methods. The samples were randomized using the R software. The output of the software was intervention (normal saline method with heparin) for half of the samples (group A) for 12 sessions. After 15 days (interval) of washout, the control group (normal saline method alone) was performed on the same group for another 12 sessions. The opposite was done for the other half of the samples (group B).
A1, Group A in the intervention stage normal saline-heparin prime; A2, Group A in the control phase (normal saline prime); B1, Group B in the control phase (normal saline prime); B2, Group B in the intervention stage (normal saline-heparin).
Inclusion criteria were age 18 to 85 years old, suffering from ESRD, admission to the hemodialysis ward regularly three times a week, and dialysis each time for at least three hours, passing more than three months since the start of dialysis.
The tools used in this study included 1- demographic characteristics, 2- disease status, and 3- information related to hemodialysis sessions. It is of note that the conditions were the same for all patients in terms of dialysis characteristics, type of dialysis solution, temperature of dialysis solution, rate of ultrafiltration, blood flow rate, and dialysis fluid rate.
URR and Kt/V formulas were used to evaluate dialysis adequacy.
Dagdras formula II with the formula Kt/V was applied to determine dialysis adequacy. It was necessary to evaluate the BUN to calculate the URR. To this end, before the dialysis, a blood sample of 3 - 5 mL was prepared directly from the red plastic line (the arterial line) before the blood was impregnated with heparin and normal saline.
Then, hemodialysis was done. To prepare a blood sample to measure BUN after dialysis, 20 seconds after the following steps, a sample was taken from an arterial red plastic line: First, the blood flow during dialysis was reduced to (100 - 50 mL per minute) and then set ultrafiltration (UF) to zero for minimal dialysis effect. The project manager prepared all blood samples. All samples were tested in a laboratory by a technician and a method to evaluate the results. In the intervention group, after setting the blood tubes of the device, we started the ventilation of the tubes and dialyzer with 1 L of sterile isotonic 0.9% heparinized normal saline solution (for 30 min with a flow of 500 mL /min). The heparin added to 1 L of normal saline serum was 1,000 units (equivalent to 0.2 mL of heparin 5,000 units). In the control group, priming of the tubes and dialysis was done by passing only 1 L of normal saline by the researcher himself.
The study was approved by the Ethics Committee of Hamadan University of Medical Sciences with the code IR.UMSHA.REC.1398.329 and registered with the code 20160110025929N25 IRCT. The collected data were analyzed using SPSS 16 and at a 95% confidence level.
Descriptive tests, parametric analytical tests (paired t-test), crossover t-test, and one-way analysis of variance (ANOVA) were used for the data analysis.
4. Results
A total of 36 patients (16 men and 20 women) with a mean age of 57.97 (± 13.70) were studied. The youngest and oldest subjects were 29 and 80 years old, respectively. Moreover, 86.1% of the patients were married, 55.6% were females, and 80.5% had secondary education and less. Other demographic variables are presented in Table 1. In both groups of patients, mean Kt /V in normal saline treatment along with heparin was higher than that in normal saline treatment alone.
| Variable | Frequency | Percent |
|---|---|---|
| Gender | ||
| Male | 16 | 44.4 |
| Female | 20 | 55.6 |
| Marital status | ||
| Single | 1 | 2.8 |
| Married | 31 | 86.1 |
| Widow (er) | 4 | 11.1 |
| Education | ||
| Illiterate | 18 | 50 |
| Literate | 5 | 13.9 |
| Secondary | 8 | 22.2 |
| High school diploma | 3 | 8.3 |
| Academic studies | 2 | 5.6 |
| Address | ||
| City | 31 | 86.1 |
| Village | 5 | 13.9 |
| Comorbidities | ||
| High blood pressure | 8 | 22.2 |
| Diabetes | 6 | 16.7 |
| Anemia | 4 | 11.1 |
| Other kidney diseases | 3 | 8.3 |
| Urological problems | 2 | 5.6 |
| High blood pressure along with diabetes | 11 | 30.6 |
| Unknown underlying disease | 2 | 5.6 |
Demographic Information of the Patients
Crossover t-test, the effect of two treatments, normal saline alone and normal saline with heparin (two treatments):
n: Number of patients in each group
Using crossover t-test, the effect of two treatments, normal saline alone and normal saline with heparin, according to KT/V criteria, was statistically significant (P < 0.001). This means that the normal saline-heparin method has been more effective in the treatment process (Table 2).
| Patient Groups | Treatment Period | Treatment | KT/V, Mean ± SD | Crossover t-test | P-Value |
|---|---|---|---|---|---|
| Group B (n = 18) | Step B1 | Normal saline alone | 1.18 ± 0.34 | ||
| Step B2 | Normal saline with heparin | 1.39 ± 0.28 | 0.0002 a | ||
| Group A (n =18) | Step A2 | Normal saline alone | 1.14 ± 0.26 | -3.42 | |
| Step A1 | Normal saline with heparin | 1.31 ± 0.36 |
Comparison of KT/V Dialysis Adequacy Criteria Before and After the Treatment in Two ̄Groups of Normal Saline with Heparin and Normal Saline Alone
In both groups of A and B, the mean adequacy of URR dialysis in normal saline along with heparin treatment was higher than that of the normal saline treatment alone.
Using the crossover t-test, the effect of two treatments, normal saline alone and normal saline with heparin was significantly different concerning the adequacy of URR dialysis (P = 0.004) (Table 3).
| Patient Groups (N =18) | Treatment Period | Treatment | Mean ± SD | Crossover t-Test | P-Value |
|---|---|---|---|---|---|
| Group B | Step B1 | Normal saline alone | 0.62 ± 0.12 | -3.06 | 0.004a |
| Step B2 | Normal saline with heparin | 0.68 ± 0.08 | |||
| Group A | Step A2 | Normal saline alone | 0.61 ± 0.09 | ||
| Step A1 | Normal saline with heparin | 0.66 ± 0.10 |
Comparison of the Effect of Normal Saline Treatment Alone and Normal Saline with Heparin on URR Dialysis Adequacy Criteria
5. Discussion
The present study examined the effect of hemodialysis machine priming using the normal saline- heparin method on URR and Kt/V. The results showed that after priming the dialysis machine by the normal saline-heparin method, URR and Kt/V indices significantly increased in the intervention phase. This result is in line with the study of Dorson et al., who investigated the effect of various methods of dialysis machine priming on dialysis adequacy index, including URR (36) and the results of Farhadi et al. (37).
The study showed that when the patient’s device was primed with normal saline alone, Kt/V values were less than 1.2, and the URR was less than 65%, suggesting that hemodialysis was not adequate. These results are in line with the results of most of the studies conducted in Iran. For instance, in Shasti et al., only half of the patients had the desired adequacy and 46% had the appropriate URR (38). In Michelle Mukriziti et al., a prime protocol with normal saline led to blood clots and interrupted treatment, nursing interventions, blood loss, and costs without any safety or benefit (39).
The results showed that when patients were in the intervention phase (preparation with normal saline- heparin), Kt/V was more than 1.2 and URR was more than 65%, suggesting that the hemodialysis was adequate. Dominic Julie et al. obtained some results similar to our findings (40).
The results of the present study revealed that the normal saline-heparin priming method increases dialysis adequacy. However, the results of other studies indicate a degree of inadequacy of dialysis in each center. Thus, one should seek solutions to mitigate existing problems better. Given the facilities and dialysis beds available and the growing need for such equipment, it is necessary to maintain the required and sufficient dialysis rate of patients with effective treatment measures. In this regard, it is critical to consider dialysis adequacy in dialysis centers to reach this level of service delivery. One of the limitations of the study was the number of samples. Hence, doing similar research with more samples and evaluating the effect of this method along with training about diet therapy and type of vascular access in future studies are recommended.
5.1. Conclusion
The use of prime normal saline-heparin method increases dialysis adequacy regarding Kt/V and URR criteria.