1. Background
Malnutrition is common in patients undergoing hemodialysis and is observed in approximately 20% - 70% of this group (1-4). Malnutrition is a serious predictive factor for mortality and morbidity accompanied by an increase in the rate of hospitalization, less physical activity, lower quality of life, and dialysis adequacy (5). An imbalance between energy and protein gain and food metabolism, metabolic acidosis, dietary restrictions, anorexia and poor appetite, protein and nutrient loss during dialysis, underlying diseases, such as cardiovascular problems, infection, poor nutrition management, inadequate dialysis, etc. are among influencing factors on the nutrition of hemodialysis patients (6). According to the results of a study, patients undergoing hemodialysis receive less energy and protein than the recommended amount for these patients (energy: 35 kcal/kg for patients younger than 60 years and 30 kcal/kg for patients older than 60 years, and protein: 1.2 g/kg) (7). Among patients undergoing hemodialysis, 6% to 8% suffer from severe malnutrition and 30% - 65% from mild malnutrition. The results of some studies have shown that one of the important causes of malnutrition is low dialysis adequacy in patients undergoing hemodialysis (5).
Evaluating the adequacy of dialysis in patients undergoing hemodialysis is important, and one of the significant goals of the health care team is high adequacy of dialysis (8). Dialysis adequacy affects appetite, intake of nutrients, and nutrition, while dialysis inadequacy is an important factor in patients’ malnutrition and mortality (9). To determine the adequacy of dialysis, urea reduction ratio (URR) and kt/v (k: filter urea clearance used, t: dialysis duration, and v: volume of urea distribution or volume of water distribution are calculated. Determination of kt/v is currently preferred to the URR (10). According to the Renal Physician Association (RPA) instruction in 1993, at least URR > %65 and kt/v > 1.2 are considered for the adequacy of dialysis. The National Kidney Foundation (NKF)-Dialysis Outcomes Quality Initiative (DOQI) also identified this criterion in 1997 and changed the kt/v value to 1.4 in 2006, and identified kt/v > 1.2 as the acceptable minimum (11).
The nutritional status of hemodialysis patients affects their clinical conditions. The nutritional status evaluation has been an important therapeutic method for this group (12). Different methods are used to screen patients regarding malnutrition (13). The following nutrition evaluation methods are currently used for assessing the nutrition status of patients: anthropometric measurements, including patients’ height and weight, triceps skinfold thickness (TSF), mid-arm circumference (MAC), body mass index (BMI), biochemical evaluations, including serum albumin, pre-albumin, hemoglobin, transferrin, total iron-binding capacity (TIBC), total lymphocyte count (TLC), C-reactive protein (CRP ), nitrogen balance, and routine blood testing to measure sodium, potassium, calcium, phosphor, urea, keratin, etc., and nutrition questionnaires, such as Subjective Global Assessment (SGA), Malnutrition-Inflammation Score (MIS), Dialysis Malnutrition score (DMS) (14).
SGA is a common semi-quantitative method that determines malnutrition status in hemodialysis patients. It is a valid and reliable method that can predict mortality independently. This is a simple, non-invasive, and inexpensive method that evaluates patients’ nutrition status mentally with no need for performing laboratory tests (15, 16). El-Sheikh and El-Ghazaly (17) claimed that dialysis dose positively correlates with serum albumin concentration, and increased albumin level can lead to lower mortality. Hemayati et al. (18) assessed 38 patients and showed that dialysis adequacy is linked to nutritional status; however, there is no significant relationship between dialysis adequacy and BMI and albumin levels.
2. Objectives
Due to the discrepancy between the results of studies and the limitations of studies with large sample size, this study was done to investigate the relationship between nutritional status based on SGA and dialysis adequacy and albumin levels in 300 patients undergoing hemodialysis.
3. Methods
3.1. Study Setting
This cross-sectional descriptive study was conducted in Tehran, Iran, in 2019. In this study, 300 qualified patients aged 18 to 75 were selected.
3.2. Sample Size
The sample size was calculated based on the following formula (
3.3. Inclusion and Exclusion Criteria
Inclusion criteria were the age of 18 to 75 years, performing hemodialysis at least twice a week, and starting hemodialysis at least three months before the study. Patients with a history of malignancy, hepatitis B, AIDS, or other acute infectious diseases, those unable to perform anthropometric measurements, and also those with episodes of hemodynamic instability following hemodialysis were excluded. Sampling was done by random clustering. First, hemodialysis centers in Tehran, Iran, were identified as clusters in the north, south, west, and east parts of the city. Eight centers were selected by the simple random method, and then all patients referring to the centers were studied. Informed consent was obtained from each participant.
3.4. Data Collection
Patients’ weight was measured carefully with a calibrated Seca digital scale (with the accuracy of 100 g). BMI was calculated based on the weight (kg)/height (m2) formula, and participants were divided into underweight (BMI < 18.5), normal weight (BMI), overweight (BMI = 25 - 30), and obese (BMI = 30) groups according to the World Health Organization category (20). After patients lied on the bed and before they were connected to the dialysis machine, 4 ml of blood samples was taken from them to measure albumin, TIBC, BUN, and Cr. Next, demographic information was collected from patients, and the SGA form was completed.
SGA form consists of two categories: medical history (including five sections: weight change, dietary intake, gastrointestinal symptoms, functional capacity, and disease and comorbidity data, such as physical injuries, burn, inflammatory diseases, and infection) and physical examination (including three sections: loss of subcutaneous fat, muscle wasting, and the presence of edema or ascites) (21). Normal parts are scored A, being influenced mildly or moderately will lead to obtaining B score, and being affected significantly will lead to gaining a C score. Finally, the total score will be as follows (Table 1) (16):
| SGA Final Score | Nutrition Status |
|---|---|
| Most parts are scored A | well-nourished |
| Most parts are scored B | mild to moderately malnourished |
| Most parts are scored C | severely malnourished |
Score A indicates normal nutrition, score B indicates moderate malnutrition, and score C represent severe malnutrition.
To confirm the reliability, the SGA form was repeated for 20 patients at a 30-day interval, and the agreement coefficient was 0.85 for two measurements. At the end of the dialysis session, the second sampling was performed, and patients were weighed again, and the results were recorded in data collection forms.
Kt/v is a ratio without a unit of measurement and shows the volume of cleaned plasma divided by the volume of urea distribution. Calculations are as follows (9):
Daugirdas II: kt/v = -Ln (R - 0.008t) + (4 - 3.5R) UF.W
Where, Ln: natural logarithm, R: the ratio of BUN (mg/dL) after dialysis to BUN (mg/dl) before dialysis (BUN2/BUN1), T: duration of each dialysis session (hour), UF: the volume of ultra-filtration (liter), and W: weight after dialysis (kg).
3.5. Statistical Analysis
Data were analyzed using SPSS 21 software. Based on the variables and distribution of data, parametric and nonparametric statistical tests, including descriptive statistics (mean, standard deviation, and absolute and relative frequency) and inferential statistics, such as paired t-test, Mann-Whitney test, chi-square test (to assess the homogeneity of the demographic characteristics of the intervention and control groups before the intervention), Wilcoxon test (to compare the mean changes in blood pressure among the patients before and after the intervention), and Mann-Whitney test (to compare the mean of blood pressure between the intervention and control groups) were used. A P-value of less than or equal to 0.05 was statistically significant.
3.6. Ethical Consideration
This study is part of a Master’s thesis in critical care nursing that was approved by the Ethics Committee of Baqiyatallah University of Medical Sciences (ethical code: IR.BMSU.REC.1393.3). Ethical considerations of the Helsinki declaration and Committee on Publication Ethics (COPE) were observed by the researchers in this study.
4. Results
In this research, 300 patients (170 male (56.7%) and 130 female (43.3%)) with an average age of 61.15 + 13.06 years and an average dialysis duration of 27.76 (+31.45) months were studied. The majority (87%) of patients reported hemodialysis three times a week for four hours, and 13% reported hemodialysis twice a week. Polysulfone filters were used for all patients.
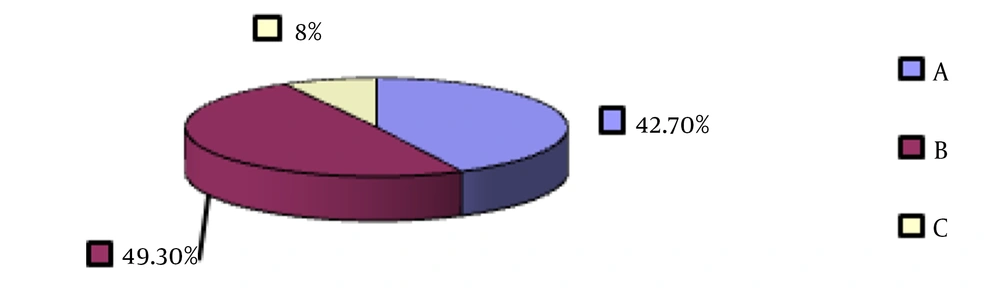
The mean albumin concentration and TIBC were 3.55 (± 0.43) and 268.18 (± 65.24). The patients’ mean dialysis adequacy was reported to be 1.07 (+ 0.27), which is lower than the acceptable minimum. Figure 1 shows the frequency of malnutrition based on the SGA index.
The chi-square test showed a significant statistical relationship between educational level and BMI of hemodialysis patients and their nutrition status, while this was not significant for gender (Table 2).
| Parameter | Frequency (Relative Frequency) Based on SGA | Total | Chi-Square Test | ||
|---|---|---|---|---|---|
| A | B | C | |||
| Gender | χ2 = 2.32; df = 2; P-value = 0.31 | ||||
| Male | 78 (29.5) | 81 (47.6) | 11 (6.5) | 170 | |
| Female | 50 (38.5) | 67 (51.5) | 13 (10) | 130 | |
| Education | χ2 = 34.7; df = 4; P-value < 0.001* | ||||
| Primary and lower | 33 (29.5) | 67 (59.8) | 12 (10.7) | 112 | |
| Diploma | 39 (36.1) | 59 (54.6) | 10 (9.3) | 108 | |
| University | 56 (70) | 22 (27.5) | 2 (2.5) | 80 | |
| BMI, kg/m2 | χ2 = 13.7; df = 6; P-value = 0.03* | ||||
| Under weight | 4 (20) | 11 (55) | 5 (25) | 20 | |
| Normal | 80 (48.2) | 75 (45.2) | 11 (6.6) | 166 | |
| Over weight | 29 (39.7) | 38 (52.1) | 6 (8.2) | 73 | |
| Obesity | 15 (36.6) | 24 (58.5) | 2 (4.9) | 41 | |
| Total | 128 (42.7) | 148 (49.3) | 24 (8) | 300 | |
a*, statistical significance, score A is normal nutrition status, score B is moderate malnutrition, score C is severe malnutrition.
One-way analysis of variance (ANOVA) showed that the concentration of albumin and TIBC is significantly higher in hemodialysis patients with normal nutrition compared to those with mild to moderate or severe malnutrition (Table 3).
| Parameter | Nutritional Status | Mean ± SD | Confidence Interval (95%) | ANOVA |
|---|---|---|---|---|
| Age, y | A | 60.69 ± 14.24 | 58.20 - 63.18 | F = 0.260; Df = 297; P-value = 0.77 |
| B | 61.70 ± 11.92 | 59.76 - 63.63 | ||
| C | 60.29 ± 13.64 | 54.53 - 66.05 | ||
| Total | 61.15 ± 13.06 | 59.76 - 62.64 | ||
| hemodialysis duration, mon | A | 27.30 ± 34.99 | 21.18 - 33.42 | F = 1.01; Df = 297; P-value = 0.36 |
| B | 26.74 ± 26.49 | 22.43 - 31.04 | ||
| C | 36.5 ± 38.99 | 20.03 - 52.97 | ||
| Total | 27.76 ± 31.45 | 24.18 - 31.33 | ||
| Albumin, mg/dL | A | 3.78 ± 0.35 | 3.72 - 3.84 | F = 78.64; Df = 297; P-value < 0.001 |
| B | 3.46 ± 0.33 | 3.40 - 3.51 | ||
| C | 2.85 ± 0.44 | 2.66 - 3.04 | ||
| Total | 3.55 ± 0.43 | 3.50 - 3.60 | ||
| TIBC, mg/dL | A | 279.98 ± 53.68 | 270.59 - 289.37 | F = 11.25; Df = 297; P-value < 0.001 |
| B | 266.83 ± 70.54 | 255.37 - 278.29 | ||
| C | 213.58 ± 60.96 | 187.84 - 239.33 | ||
| Total | 268.18 ± 65.24 | 260.77 - 275.60 | ||
| Dialysis adequacy | A | 1.17 ± 0.21 | 1.13 - 1.21 | F = 43.72; Df = 297; P-value < 0.001 |
| B | 1.03 ± 0.23 | 1 - 1.07 | ||
| C | 0.69 ± 0.37 | 0.53 - 0.85 | ||
| Total | 1.07 ± 0.27 | 1.03 - 1.1 |
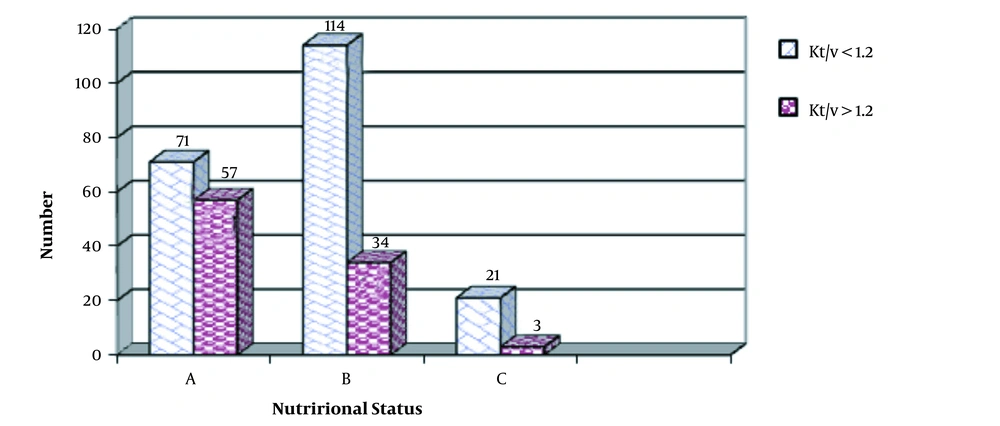
The results showed that dialysis adequacy was higher in patients with normal nutrition status; however, mean dialysis adequacy was lower than the acceptable minimum even in this group (Figure 2).
5. Discussion
The present study was done to investigate the relationship between nutritional status based on the SGA scale and dialysis adequacy and albumin levels in hemodialysis patients. Dialysis adequacy was associated with nutritional status and decreased with an increase in malnutrition.
The relative frequency of mild to moderate and severe malnutrition based on SGA in this study was 57.3%, which agrees with previous studies in Iran and other countries (20, 22, 23). Todd et al. (24) reported moderate malnutrition in Australian hemodialysis patients, and Mazairac et al. (25), in a multicenter study, reported a malnutrition prevalence of 23% in a large cohort of 560 patients. According to different studies, insufficient intake of daily energy and protein, limitation in receiving special food groups, lack of appetite, and loss of water-soluble nutrients during hemodialysis, and also unnatural metabolism of nutrients can lead to unfavorable nutritional conditions (26-28).
A cohort study showed that gender has a significant relationship with the relative frequency of malnutrition based on the SGA index (6). This finding is in line with the present study and is in contrast to the results of Ashabi et al. (23).
In the present study, the relative frequency of malnutrition in hemodialysis patients showed no significant relationship with age; however, in a study Ashabi et al. (23), the relative frequency of malnutrition in patients younger than 60 years was 75%, and it was 45% in patients older than 60 years.
Different studies have shown that the relative frequency of malnutrition in hemodialysis patients is higher in patients with longer dialysis duration compared to those with shorter periods (29, 30). This contradicts the present study, which can be due to the number of samples, sampling method, geographical location, etc.
We found that higher education leads to better nutrition, which keeps the body weight in a healthy range and is associated with better BMI. de Mutsert et al. (31) declared that there is a significant relationship between BMI and nutritional status based on the SGA index.
One of the important mortality predictors in patients suffering from chronic renal failure is a reduction in albumin serum concentration (hypo-albumin). The risk of mortality is seven times more for each 1-g/dL decrease in albumin serum concentration. Albumin level is not the only indicator of the nutritional status and is decreased by inflammations; however, it is appropriate in identifying people at risk of malnutrition (31-33). The findings of this research showed that hypo-albumin is statistically related to malnutrition, which is consistent with the results of Cohort studies by Chan et al. (6) and de Mutsert et al. (31).
TIBC is also an indicator of nutritional status and is used in nutrition assessment scales, such as MIS (34). Some quantitative studies have been done on the relationship between TIBC and malnutrition status based on the SGA index. The present study showed that similar to albumin, TIBC has also a significant relationship with nutritional status and it is lower in hemodialysis patients with moderate and severe malnutrition.
The present study showed that the adequacy of dialysis in patients was lower than the standard value, which agrees with many studies (35, 36). Urea uptake in a dialysis session is an important factor for the adequacy of dialysis and dialysis adequacy is not related to plasma urea alone. Venous stenosis, arterial-venous fistula, failure to follow regular dialysis programs by patients, hemodynamic instability, cardiovascular diseases, and infections are among the proposed reasons for dialysis inadequacy (37, 38). According to the present study, malnutrition can be also considered as a factor leading to dialysis inadequacy, and there is a direct relationship between them.
There are several reasons for the difference in the prevalence of malnutrition and its associated factors, such as, such as the adequacy of dialysis in different studies can be due to differences in methods of assessing malnutrition, different age groups, duration of illness, and underlying diseases, drug use, and socioeconomic factors, including the patient’s level of education and knowledge about the disease, family support, the level of access to food, eating habits, and culture in each region, which can affect the nutritional status.
This research was a multicenter study in which participants from different backgrounds can be included, which is one of the strengths of this study. Decrease in dialysis time period due to patient intolerance, stopping or slowing down dialysis due to complications during dialysis, such as hypotension, muscle cramps, and angina, and finally filter k parameter less than what the company claimed, were among the limitations of the study.
5.1. Conclusions
The results showed a significant statistical relationship between nutritional status and education, BMI, albumin, TIBC, and dialysis adequacy. Therefore, training workshops for educating patients about proper hemodialysis, keeping weight at normal range, the use of nutritional supplements along with routine diet to receive nutrients, monthly check of dialysis adequacy, investigation of patients’ nutritional status through different methods, and the presence of a diet specialist are necessary for hemodialysis wards. We hope this study prepares backgrounds for future interventional studies.