1. Background
End-stage renal disease (ESRD) is a major public health problem, and its incidence increases with age (1, 2). According to a 2014 report by the United States Renal Data System (USRDS), over 80% of patients with ESRD worldwide choose hemodialysis (HD) as their preferred and first renal replacement therapy. Therefore, reliable vascular access is essential for adequate hemodialysis and maintaining a satisfactory quality of life in these populations. Impaired vascular access is one of the most important factors contributing to the hospitalization of hemodialysis patients, as well as their intoxication and overall mortality (3).
Clinical guidelines for vascular access recommend arteriovenous fistula (AVF) as the preferred method for dialysis due to its long-term efficacy and low complications. However, AVF also has a number of disadvantages, including the need for more time to mature and a higher rate of initial failure. In a recent study, the initial estimate of AVF failure and its initial 1-year recurrence were reported 23% and 60%, respectively (4).
The first evidence of a link between chronic kidney diseases and cardiovascular diseases dates back more than 40 years ago (5). Cardiovascular (CV) events are the leading causes of mortality and morbidity in patients with ESRD, with an incidence rate of 10 to 30 times higher than the general population. In addition to the usual risk factors of these events, certain uremic disorders, including vascular calcification, are also responsible for the high prevalence of CV events in patients with ESRD, which may include arterial media abnormalities, atherosclerotic plaques, and heart valves calcification (6). In addition, aortic arch calcification (AAC) is an independent predictor of CV-related mortality in ESRD patients (7) and may also be a predictor of the loss of initial AVF efficiency (8).
According to studies, 26 to 78% of the patients undergoing dialysis have different degrees of AAC in chest X-ray (CXR), which in 34 to 60% of them, the disease progresses after 1- to 5-year of follow-up (9). Therefore, Chest radiographs, nearly universally available in dialysis patients, are inexpensive, involve low-radiation dose, and is a strong independent predictor of CV events in hemodialysis patients (10).
2. Objectives
Due to the fact that the evaluation of arterial calcification to examine the prognosis of hemodialysis patients is not routinely performed, and also due to the importance of this issue, this study aimed to ascertain the rate of one-year AVF failure and assess its related factors in patients with ESRD in Golestan province.
3. Methods
3.1. Study Design
This descriptive-analytical cross-sectional study was performed on patients (age > 20 yrs) with ESRD who were candidates for AVF and referred to the Shahid Sayad Shirazi hospital of Gorgan, as the referral center in the Golestan province of Iran.
Demographic and clinical data of participants were collected using a checklist. Posterior-anterior chest X-ray was performed as soon as AVF was placed, and the graphs were classified by a radiologist who had no knowledge about the patients’ clinical conditions. For ACC classification, we followed the criteria described by Zhang et al. (10).
According to the rate of patient referral, the required sample size was expected to be completed within about six months, and then the patients were followed up for one year. Overall, the process of data collection lasted from August 2018 to the December 2019. (approx. 20 months). A total of 112 patients were included in the study and followed up until December 2019.
During the 1-year follow-up period, AVF maturation time, AVF failure, and in efficiency, the incidence and types of cardiovascular events, and mortality were evaluated (Arteriovenous fistula failure was detected when that fails within two months of use, but the patient was alive during the 12-month follow-up).
Exclusion criteria included FF during the first month after placement, being followed up less than one month after surgery (due to death or lack of cooperation), and already having AVF but no CXR. After collecting the patients’ data from clinical archives in the ward, their radiographic data was sent to a radiologist, and the graphs of ACC classification were collected and recorded.
After one month and then in the sixth and twelfth months, each patient was called separately, and questions were asked to determine either treatment failure or its success, as well as the occurrence of cardiovascular events. If necessary, the patient was requested to visit for an examination to ensure the incidence of the outcomes. Other patients were followed up in the same way until either the first failure or the end of the one-year period. At each follow-up checkpoint (i.e., the first, sixth, and twelfth months), required information was gathered by a questionnaire. Three questionnaires were used in this study; one questionnaire for the time of fistula placement, one questionnaire for one month after fistula placement, and another questionnaire for follow-up. The duration of the initial efficiency of the arteriovenous fistula was regarded from the time of AVF placement to the first occlusion or any other obstacle causing the return of the blood flow, including inadequate AVF blood flow, hypertension, narrow cannulation, site-limited cannulation, and other complications rendering AVF inaccessible.
3.2. Ethical Issues
This study was conducted after obtaining approval from the Research Ethics Committee of Golestan University of Medical Sciences (Registration code: IR.GOUMS.REC.1398.042). Informed consent was also obtained from patients. All patient information was kept confidential by the researcher until the end of the study. All the procedures taken on patients were parts of diagnostic and therapeutic processes and did not cause any loss or damage to the subjects. The participants were free to discontinue at any stage if they wanted.
3.3. Data Analysis
The data were analyzed using SPSS 19 software. The subjects were divided into two groups of ≥ 58 years and < 58 years. The Chi-square test was used to assess the relationship between AVF failure and mortality with different variables. A P value less than 0.05 was considered statistically significant.
4. Results
In this study, a total of 112 individuals were studied, of whom 63 (56.2%) were males, and 49 (43.8%) were females. The mean (standard deviation) age of the subjects was 56.83 (15.01) years.
Out of 112 patients, six were excluded from the study during the first month due to AVF failure. From 106 participants who remained in the study and were included in the final analysis, 12 (11.3%) died within two to 12 months and were excluded from the AVF failure analysis. Of a total of 94 patients who were successfully followed for 12 months, five (5.3%) developed AVF failure.
According to Table 1, the frequency of FF was not significantly associated with gender (P = 0.27). Also, the frequency distribution of one-year AVF failure in terms of AAC and its grades showed no statistically significant relationship (P > 0.05).
| Variables | Total | AVF Failure | P-Value | Mortality | P-Value | ||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | ||||
| Age group | 0.65 | 0.28 | |||||
| 58 > | 54 | 2 (4.3) | 45 (95.7) | 4 (7.8) | 47 | ||
| 58 ≤ | 58 | 3 (6.4) | 44 (93.6) | 8 (14.5) | 47 | ||
| Gender | 0.27 | 0.50 | |||||
| Female | 49 | 4 (7.5) | 49 (92.5) | 8 (13.1) | 53 | ||
| Male | 63 | 1 (2.4) | 40 (97.6) | 4 (8.9) | 41 | ||
| Aortic arch calcification | 0.86 | 0.12 | |||||
| Yes | 96 | 4 (5.1) | 92 (94.9) | 12 (13.3) | 78 | ||
| No | 16 | 1 (6.2) | 15 (93.8) | 0 (0) | 16 | ||
| Aortic arch calcification (grade) | 0.91 | 0.01 | |||||
| 0 | 17 | 1 (6.2) | 15 (93.8) | 1 (2.3) | 43 (97.7) | ||
| 1 | 28 | 1 (3.7) | 26 (96.3) | ||||
| 2 | 35 | 1 (4) | 24 (96) | 11 (17.7) | 51 (82.3) | ||
| 3 | 32 | 2 (7.7) | 24 (92.3) | ||||
| Diabetes | 0.70 | 0.02 | |||||
| Yes | 60 | 3 (6.4) | 44 (93.6) | 9 (16.1) | 47 (83.9) | ||
| No | 47 | 2 (4.5) | 42 (95.5) | 1 (2.2) | 44 (97.8) | ||
| Hypertension | 0.23 | 0.1 | |||||
| Yes | 73 | 2 (3.4) | 57 (96.6) | 9 (13.2) | 59 (86.8) | ||
| No | 34 | 3 (9.4) | 29 (90.6) | 1 (3) | 32 (97) | ||
| Cardiovascular disease | 0.21 | 0.00 | |||||
| Yes | 44 | 3 (9.7) | 28 (90.3) | 8 (20.5) | 31 (79.5) | ||
| No | 63 | 2 (3.3) | 58 (96.7) | 2 (3.2) | 60 (96.8) | ||
| Dialysis | 0.73 | 0.62 | |||||
| Yes | 106 | 5 (5.6) | 85 (94.4) | 11 (10.9) | 90 (89.1) | ||
| No | 1 | 0 (0) | 2 (100) | 0 (0) | 2(100) | ||
| Open heart surgery | 0.28 | 0.32 | |||||
| Yes | 8 | 1 (14.3) | 6 (85.7) | 0 (0) | 7 (100) | ||
| No | 99 | 4 (4.7) | 82 (95.3) | 12 (12.2) | 86 (87.8) | ||
| Drug history (statin therapy) | 0.85 | ||||||
| Yes | 30 | 2 (8.3) | 22 (91.7) | ||||
| No | 15 | 1 (6.7) | 14 (93.3) | ||||
| Serum calcium (adjusted for serum albumin) | 0.81 | ||||||
| 8.6 > | 21 | 1 (5.3) | 18 (94.7) | ||||
| 8.6 - 10.3 | 90 | 3 (4.1) | 71 (98) | ||||
| Serum phosphorus | 0.22 | ||||||
| 5 ≥ | 63 | 1 (2) | 50 (98) | ||||
| 5 < | 48 | 3 (7.1) | 39 (92.9) | ||||
| Serum albumin | 0.00 | ||||||
| 3.5 ≤ | 21 | 0 (0) | 22 (100) | ||||
| 3.5 > | 90 | 4 (4.4) | 86 (95.6) | ||||
| BMI | 0.33 | ||||||
| 18 > | 10 | 2 (20) | 8 (80) | ||||
| 18 - 25 | 58 | 3 (5.1) | 42 (94.9) | ||||
| 25 - 30 | 42 | 1 (3) | 32 (97) | ||||
| 30 < | 2 | 0 (0) | 0 (100) | ||||
aValues are expressed as No. (%) unless otherwise indicated.
Patients with a history of cardiovascular disease (9.7%), dialysis (5.6%), and open-heart surgery (14.3%) had a higher one-year fistula failure rate than those without these risk factors (P < 0.05). Although the one-year FF rate was higher in patients with serum calcium levels of < 8.6 mg/dL (5.4%) compared to those with calcium levels of 8.6 to 10.3 (3.6%), the difference was not statistically significant (P = 0.67).
Also, the one-year FF rate was not significantly different comparing patients with adjusted serum calcium levels of < 8.6 mg/dL or between 8.6 mg/dL and 10.3 mg/dL (P = 0.81).
Moreover, the frequency of mortality was higher in the patients aged ≥ 58 years (14.5%, P = 0.28), in men (13.1%, P > 0.05), and those with AAC (13.3% vs. 0% in patients without this complication, P = 0.12). Likewise, the mortality rate was lower in patients with a low AAC grade (grades 0 and 1) (2.3%) compared to those with a high AAC grade (grades 2 and 3) (17.7%), which was statistically significant (P = 0.01).
The mortality rate was also higher in patients with a history of cardiovascular disease, diabetes, hypertension, dialysis, and open-heart surgery, but it was significantly associated only with past histories of cardiovascular disease and diabetes (P < 0.05). Regarding the between AAC and age, our results showed that patients aged ≥ 58 years old had a higher degree of calcification, which was statistically significant (P = 0.001) (Table 1).
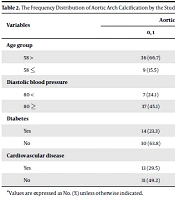
Compared with patients without these comorbidities, the degree of calcification of the aortic arch was significantly higher in patients with a history of diabetes (76.7% vs. 23.3%, P = 0.001) and cardiovascular disease (70.5% vs. 29.5%, P = 0.042) (Table 2).
| Variables | Aortic Arch Calcification (Grade) | P-Value | |
|---|---|---|---|
| 0, 1 | 2, 3 | ||
| Age group | 0.00 | ||
| 58 > | 36 (66.7) | 18 (33.3) | |
| 58 ≤ | 9 (15.5) | 49 (84.5) | |
| Diastolic blood pressure | 0.04 | ||
| 80 < | 7 (24.1) | 22 (75.9) | |
| 80 ≥ | 37 (45.1) | 45 (54.9) | |
| Diabetes | 0.00 | ||
| Yes | 14 (23.3) | 46 (76.7) | |
| No | 30 (63.8) | 17 (36.2) | |
| Cardiovascular disease | 0.04 | ||
| Yes | 13 (29.5) | 31 (70.5) | |
| No | 31 (49.2) | 32 (50.8) | |
aValues are expressed as No. (%) unless otherwise indicated.
5. Discussion
This study was performed on 112 patients with ESRD who were candidates for AVF and referred to the Shahid Sayad Shirazi hospital of Gorgan. The patients were followed up for one-year; 56.2% of the patients were males, and the mean age of the participants was 56.83 ± 15.01 years, which was close to the results of other studies (11, 12).
During one-year follow-up, 5.3% of the patients developed arteriovenous FF, and this rate was higher in men than in women, but the difference was not statistically significant. This observation was consistent with the findings of Choi et al. and Keshvati et al. (13, 14). However, in some studies, the rate of FF has been higher in women, suggesting the smaller vascular diameter in females as a possible reason for their higher rate of premature FF (15, 16).
Considering the overall prevalence of AVF failure, other studies have reported higher rates compared to our study (5.3%). In the studies conducted by Yap et al., Choi et al., and Alshaikh Ahmad et al., AVF failure rates were reported to be 19%, 39.5%, and 33%, respectively (13, 17, 18).
In our study, although the majority of AVF candidates had histories of diabetes, hypertension, cardiovascular disease, and dialysis, there were no significant relationships between these comorbidities and the rate of one-year FF, which was in line with the observations of Choi et al. In a prospective study on 283 AVF candidates, 29.3% and 40.3% of the patients were diagnosed with diabetes and hypertension, respectively, and a significant relationship was found between the success rate of AVF insertion and a history of diabetes and hypertension (13).
In line with our results, Rezapour et al. and Rezapour and Khavaninzadeh noted that, these two diseases were risk factors for AVF failure (19, 20).
In the present study, more than half of the patients had serum calcium levels of 8.6 - 10.3 mg/dL and phosphorus levels of < 5 mg/dL, but no correlation was found between serum mineral levels and the FF rate. This was similar to the results of Yap et al. (17).
We also assessed a possible relationship between the grade of AAC and the rate of arteriovenous FF. According to our findings, the highest percentage of calcification (7.7%) was observed in patients was AAC grade 3. However, no significant link was observed between the AAC grade and AVF failure rate. In the study of Yap et al., 79.2% and 54.2% of the subjects had AAC and high-grade AAC, respectively. In another study, AAC was initially observed in 60% of patients and increased to 77% during a four-year follow-up (17).
This study showed that AVF failure had no significant relationship with the history of comorbidities (including diabetes, hypertension, cardiovascular disease, and dialysis) and open-heart surgery, as well as serum calcium and phosphorus levels, consuming medications, and body mass index. On the other hand, lower albumin levels were associated with higher failure rates.
Yap et al., found that the AAC grade was significantly associated with an older age, a history of coronary artery disease, and a higher diastolic blood pressure. Also, serum calcium levels were significantly higher in patients with high-grade ACC (21). Also, serum calcium levels were significantly higher in patients with high-grade vs. low-grade ACC, but there was no significant difference comparing the serum levels of phosphorus and albumin between the two groups (21). In another study, the AAC grade increased with age, was higher in males, and was significantly associated with a history of hypertension, diabetes, and chronic kidney disease (22).
In the present study, patients with low-grade AAC also showed lower mortality rates., and severe AAC was found to be significantly associated with a diastolic blood pressure of higher than 80 mmHg. However, in the study of Yap et al., high-grade AAC was associated with a lower diastolic blood pressure (17). For explanation, it should be said that arterial stiffness is a common complication in patients with chronic kidney diseases, and aorta stiffness can increase systolic blood pressure and decrease diastolic pressure, leading to a rise in pulse pressure (13).
5.1. Conclusions
In this study, it was found that the rate of FF in patients with a history of chronic heart disease, diabetes, and hypertension was higher, which seems to be due to the impact of these diseases on vascular endothelium and changes in vascular resistance. The rate of vascular failure was not related to age and gender, and the AAC grade inversely correlated with the serum albumin level.