1. Background
Sexually transmitted diseases (STDs), such as gonorrhea, chlamydia infection, syphilis, genital herpes, and the human immunodeficiency virus/acquired immunodeficiency syndrome, are common and serious health problems worldwide (1). The STDs impose a heavy burden on health care systems and are attributed to serious health conditions in both genders. The importance of STDs is such that the World Health Organization lists Neisseria gonorrhoeae as one of twelve organisms on the “global priority list of antibiotic-resistant bacteria” (2).
Approximately 126 million new cases of STDs annually occur; nevertheless, two-thirds of STDs cases are reported or diagnosed among adolescents and young adults (3). Global statistics show that annually one-third of new cases of STDs are under 25 years of age (4). The STDs also account for most male urethritis; nonetheless, the symptoms include urethral discharge, irritation, and dysuria (5). In men younger than 35 years of age, Chlamydia trachomatis is the most common cause of epididymitis (6). Furthermore, comorbidities are common among STD pathogens. For instance, epididymitis, which causes pain and swelling almost always unilateral, can be accompanied by inflammation in the testes, especially viral orchitis (7, 8).
Despite the magnitude and seriousness, the implementation of primary and secondary prevention against STDs is not straightforward in many settings. For example, the primary prevention of STDs is typically orchestrated by training and educating on the most important mode of transmission (i.e., sexual relationship) (9). Nevertheless, educating on safe sex is not socially acceptable occasionally and might arise various social and even political confrontations. Despite this obstacle, STDs can be potentially controlled by several well-established activities, such as partner notification, which involves interviewing individuals diagnosed with STDs, obtaining information about their sexual partners, and locating these partners so that they can be referred for testing and treatment (10, 11).
Regarding secondary prevention, the emergence of antimicrobial resistance and inherent behaviors of some STD pathogens to cause asymptotic infection, especially in men, might obstruct the early detection and timely treatment of STDs. A survey conducted on 16 sexual health clinics in England reported a gender difference in treatment-seeking behavior following the contraction of asymptotic STDs; accordingly, seeking treatment by asymptotically infected men with STDs is expected only when there was a symptomatic disease or diagnosis in their partners (12).
Undoubtedly, sexual health has great importance on the human quality of life; however, scientific evidence on sexual health and morbidities from developing countries is scarce. On the other hand, the prioritization of reproductive health problems and resource allocation to address priority issues require valid epidemiological information. For the provision of such data, a comprehensive nationwide project was carried out to identify the prevalence and contributory factors of three reproductive morbidities (namely infertility, STDs, and sexual dysfunction) in the male population within the age range of 25 - 60 years in Iran. The present study used a part of the aforementioned data to estimate the prevalence of STDs and determine important related factors to this problem.
2. Methods
This cross-sectional study used the data from a nationwide project entitled “National Survey On Reproductive Morbidities Among Males in Iran in 2007”, conducted by the Men’s Health and Reproductive Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran, in cooperation with the United Nations Population Fund and the Iranian Ministry of Health. The study population consisted of all men within the age range of 25 - 60 years residing in four provinces across the country, including Golestan in the north, Hormozgan in the south, Kermanshah in the west, and Isfahan in the center of Iran. The selected provinces were randomly chosen from 31 provinces in Iran; however, three cities were selected from each province, and the sample size was assigned proportionally to the census population of 25 - 60-year-old males stratified on residence area (i.e., urban or rural).
Subject recruitment was carried out by systematic cluster sampling. For reaching the final sample size of 2296, 328 cluster heads (each with a size of 7) were defined based on the registered household number in healthcare centers. After the selection of households within each cluster, one male subject from each household within the age range of 25 - 60 years was invited to visit the healthcare center. The inclusion criteria were defined as the age range of 25 - 60 years and residence in the study area for at least 3 months before conducting the study. The exclusion criteria were defined as hospitalization during the study course and unwillingness to participate in the study.
The data were collected using structured questionnaires by trained interviewers who were local general practitioners. Clinical examination included the measurement of height, weight, and blood pressure. Laboratory findings included semen analysis, urethral smear, follicle-stimulating hormone, and testosterone level. Ethical approval was granted by the Review Board of Shahid Beheshti University of Medical Sciences. Verbal informed consent was sought from the respondents before the interview.
A structured checklist, including demographic information, was filled out by the subjects. Furthermore, the data on the symptoms of STDs, including genital secretion, pushing out, itching or genital ulcers, and lymphadenopathy of the inguinal area after sexual contact, were collected by trained urologists. Interviews were performed by trained interviewers who received one training session at the Men’s Health and Reproductive Health Research Center in February 2007 in Tehran. Data analysis was carried out using SPSS software (version 18.0, Chicago, IL, USA). The independent samples t-test and Chi-square test were used for data analysis.
3. Results
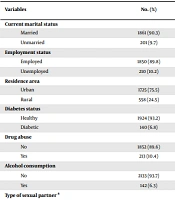
In total, 2296 men with a mean age value of 39.95 ± 10.3 years were interviewed in this study. Two-thirds of the subjects (75.5%) resided in urban areas. Most subjects (90.8%) were married; however, the mean age value at first marriage was 24.22 ± 3.94 years (range: 16 - 54 years). Moreover, the mean length value of marriage was 16.92 ± 10.5 years. Among those who reported being single (n = 210), 42 subjects (20%) reported having sexual intercourse, mainly with a fixed partner. Extramarital relationship, mainly with a fixed partner, was reported by 81 married subjects (4%). Two-thirds of all the subjects (75%) were aware of using condoms in suspected sexual relationships; nonetheless, only 69% of the aforementioned subjects used condoms in those circumstances.
Most subjects (80%) were reported as employed; nevertheless, the highest (9.2%) and lowest (3.6%) unemployment rates were observed in Kermanshah and Isfahan provinces, respectively. Regarding cigarette smoking, 7 and 25% of the subjects smoked occasionally and daily over the preceding year, respectively. Daily and occasional exposures to cigarette smoking were reported by 9 and 18.5% of the subjects, respectively. Additionally, 10.4% of the subjects reported any drug abuse in occasional (7%) and daily (4%) forms. No history of STDs, including secretion from the duct, burning duct, and testicular swelling and pain, was reported by 1.4, 4.9, and 1.6% of the subjects, respectively.
3.1. STD Referral and Treatment
Based on the medical decision by the study interviewers as certified general practitioners, a total of 14 subjects (0.6%) had one type of STDs at the study time. Furthermore, 110 subjects (4.7%) answered “yes” to the question of whether they were referred to a physician for sexual problems, only 27% (n = 30) of whom sought medical treatment. Delayed referral, defined as seeking medical treatment at least 2 weeks after the appearance of symptoms, was reported by 56.7% of symptomatic cases (n = 17).
The prevalence of STDs was higher among unmarried (1%) and employed (0.8%) subjects. The differences in the prevalence of STDs according to marital and employment status were not statistically significant. On the other hand, a significantly higher proportion (0.8%) of urban respondents reported having STDs, compared to that (0.2%) of rural respondents (P = 0.032). Moreover, a significantly higher proportion (17.8%) of respondents with multiple sexual partners reported having STDs, compared to that (0%) of respondents with a single sexual partner (P = 0.012). Nearly 1% of the subjects with enough knowledge of using condoms and 1% of subjects who were condom users during suspected sexual intercourse were observed to have STDs, which was significantly higher, compared to that (0%) of subjects with insufficient knowledge of the issue (P = 0.033; Table 1).
| Variables | No. (%) | STDs | P-Value | |
|---|---|---|---|---|
| Absent; No. (%) | Present; No. (%) | |||
| Current marital status | 0.403 | |||
| Married | 1861 (90.3) | 1849 (99.3) | 12 (0.7) | |
| Unmarried | 201 (9.7) | 199 (99) | 2 (1) | |
| Employment status | 0.206 | |||
| Employed | 1850 (89.8) | 1836 (99.2) | 14 (0.8) | |
| Unemployed | 210 (10.2) | 210 (100) | 0 (0) | |
| Residence area | 0.032 | |||
| Urban | 1725 (75.5) | 1712 (99.2) | 13 (0.8) | |
| Rural | 558 (24.5) | 557 (99.8) | 1 (0.2) | |
| Diabetes status | 0.627 | |||
| Healthy | 1924 (93.2) | 1911 (99.3) | 13 (0.7) | |
| Diabetic | 140 (6.8) | 139 (99.2) | 1 (0.8) | |
| Drug abuse | 0.570 | |||
| No | 1852 (89.6) | 1839 (99.3) | 13 (0.7) | |
| Yes | 213 (10.4) | 211 (99.5) | 1 (0.5) | |
| Alcohol consumption | 0.633 | |||
| No | 2133 (93.7) | 1909 (99.3) | 13 (0.7) | |
| Yes | 142 (6.3) | 141 (99.3) | 1 (0.7) | |
| Type of sexual partner a | 0.012 | |||
| Multiple | 45 (60) | 37 (82.2) | 8 (17.8) | |
| Fixed | 30 (40) | 30 (100) | 0 (0) | |
| Knowledge of using condoms | 0.033 | |||
| Absent | 455 (21.9) | 455 (100) | 0 (0) | |
| Present | 1620 (78.1) | 1606 (99.1) | 14 (0.9) | |
| Condom use in suspected sexual intercourse | 0.021 | |||
| No | 517 (25.5) | 517 (100) | 0 (0) | |
| Yes | 1510 (74.5) | 1497 (99.1) | 13 (0.9) | |
Abbreviation: STDs, sexually transmitted diseases.
a Among those with reported extramarital sexual relationships.
4. Discussion
STDs are considered health problems in most parts of the world. The so-called term of STDs refers to a variety of clinical syndromes caused by pathogens that can be acquired and transmitted mainly through sexual activities. STDs are among the first 10 causes of unpleased diseases in young male adults. It is estimated that each year 340 million cases of STDs occur in men and women aged 15 - 49 years worldwide. More than 1 million sexually transmitted infections are acquired every day worldwide (13). The STDs have been reported from all over the world, and Iran is no exception in this regard; however, 61% of the Iranian population are in a sexually active life period (age range: 15 - 49 years) (14).
The results of the present study showed that 0.8% of employed participants had STDs; nonetheless, none of the unemployed subjects was observed to have STDs; however, the difference was not statistically significant. Regarding the relationship between occupation and STDs, Alemu et al., in a study conducted on 628 individuals aged 25 - 64 years suggested that unemployment is an underlying factor for high-risk sexual behaviors, which might lead to the contraction of STDs (15). The present study showed that there was no relationship between STDs and alcohol consumption; accordingly, an equal proportion of subjects, stratified based on alcohol consumption, were observed to have STDs (0.7%).
Another well-known risk factor for STDs contraction is having multiple sexual partners. In the current study, a significantly higher proportion (18%) of subjects with multiple sexual partners reported having STDs, compared to that (0%) of subjects with a single sexual partner (0%). Several reports across the world have also indicated a relationship between the use of condoms and the risk of STDs. Koss et al. conducted a systematic review on 12 studies focusing on condom use and syphilis risk, indicating a lower probability of syphilis contraction following condom use in sexual intercourse (16). Nevertheless, further studies are needed to determine the association between condom use and syphilis prevalence.
The present study showed that the prevalence of STDs was significantly higher in individuals who used condoms in suspected sexual intercourse and had enough knowledge of condom use in suspected sexual intercourse. This finding is in contrast to the finding of previous reports showing that the consistent and correct use of male condoms is the primary method preventing the acquisition or transmission of STDs (17-19). This inconsistency might be due to the fact that condom use was reported only by subjects who reported having multiple sexual partners. In other words, condom use during sexual intercourse was not reported by any of the respondents who had a single sexual partner. This result is consistent with the results of a qualitative study reporting that condom use by men greatly depends on relationship duration. In other words, men feel that their role should be to support and communicate with their partners in a stable relationship with a single sexual partner. Therefore, an unlikely use of condoms is frequently reported in this regard. On the other hand, occasional sexual intercourse with multiple partners impose the feeling of self-protection, which leads to more likelihood of condom use by men (20).
Effective interventional programs to eliminate STDs require systematic monitoring of disease incidence and high-risk behavior prevalence, especially in young individuals. This monitoring should be accompanied by the consistent application of well-designed and reliable epidemiologic methods, metrics, and progress indicators. Additionally, it is required to design accurate, precise, and easily understood monitoring tools. Based on this perspective, the implementation of primary prevention programs to educate the population, especially young individuals, on protection against STDs and the provision of safety measurements (e.g., mechanical contraception devices) are highly warranted. Based on an epidemiologic perspective, the surveillance of STDs should be strengthened to detect inherent biases, allow for fast-tracking schemes, and act and respond timely and properly. One desired attribute of such a surveillance system would be using a combination of relative and absolute measures, such as rate ratios, rate differences, and population-attributable proportions instead of any single measure in assessing the progress of prevention programs (21).
This study demonstrated that overall 0.6% of the subjects (n = 14) had at least one type of STDs at the study time. The estimated prevalence of STDs was mainly reported among specific subpopulations, such as homosexual men, homeless individuals, and individuals with high-risk sexual activities. To the best of our knowledge, a limited number of studies have been performed to estimate the prevalence of STDs in the general population, which is one of the strengths of the present study. On the other hand, the measurement of STDs was assessed by general physicians, where some detailed examination to detect STDs might be missed. Furthermore, due to the executive inability to use laboratory diagnostic kits, it was not possible to detect the co-infections of sexually transmitted pathogens in respondents.
4.1. Conclusion
The prevalence of STDs is still low among the male population in Iran. Careful and well-designed surveillance systems to monitor the incidence of STDs and proper preventive measures to restrict the spread of sexually transmitted pathogens are among the proposed recommendations.