1. Introduction
Lumbar interbody fusion (LIF) is a type of surgery performed to treat spinal disorders such as spondylolisthesis, trauma, infection, and neoplasm (1). There are various approaches proposed for LIF, among which posterior lumbar interbody fusion (PLIF) is a minimally-invasive surgery. However, several complications have been reported for PLIF, including ureteral injuries (2-6). The most common predisposing agents of ureteral injury during PLIF are patient’s leanness, anterior annulus weakness, retroperitoneal scars or adhesions, the limited exposure of the retroperitoneal space, extra manipulating of the retroperitoneal fat layer, and surgical instruments used during discectomy or PLIF that may induce injury (4, 7, 8). One of these ureteral injuries is the obstruction, the signs and symptoms of which depend on the location of the blockage, complete or partial blockage, growth rate, and its effect on one or both kidneys (9). Moreover, the signs and symptoms of ureteral obstruction include flank or abdominal pain, abdominal ileus with distention, nausea, vomiting, and loss of appetite. The flank pain is created by both hydronephrosis and retroperitoneal urinoma (7). In the literature, ureteral injury following spinal surgery has been mostly reported to happen after posterior approaches such as laminectomy and discectomy (4, 5, 7). The purpose of this report was to inform surgeons and physicians of a rare case of ureteral injury by passing five years from PLIF. As well, the non-specific clinical signs of ureteral injury after PLIF surgery were considered; however, a long time has passed.
2. Case Presentation
The patient is a 51-year-old 70 kg‑weighted woman who has referred gastroenterologist about one month ago due to flank pain, fever, anorexia, vomiting, and nausea when eating fluids especially watermelon. Firstly, the pain engages the abdomen, then localizes to the right flank, and lastly is drawn into the inguinal. An endoscopy is performed for the patient and everything is reported to be normal.
In the patient's history, she has referred to a neurosurgeon five years ago due to lower limb pain, with a diagnosis of spondylolisthesis (grade 2) that eventually underwent L4-L5 PLIF surgery. During the surgery procedure, laminectomy, discectomy, and foraminotomy were performed and four pedicular screws and two rods were implanted for the patient.
After the computed tomography (CT) of the abdomen and pelvis and visit by the general surgeon, there was no particular problem except for brief hydronephrosis in the left kidney. So that even asked the patient psychiatric counseling with a diagnosis of the neuro-functional disorder. The psychologist confirmed the neuro-functional disorder concerning family problems, mood disorders, anorexia, sleep disorders, and a history of postpartum depression.
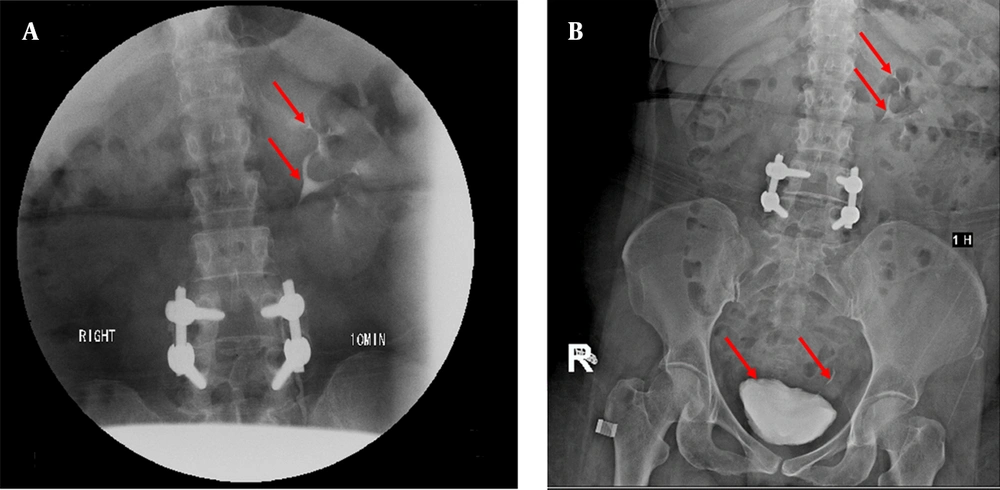
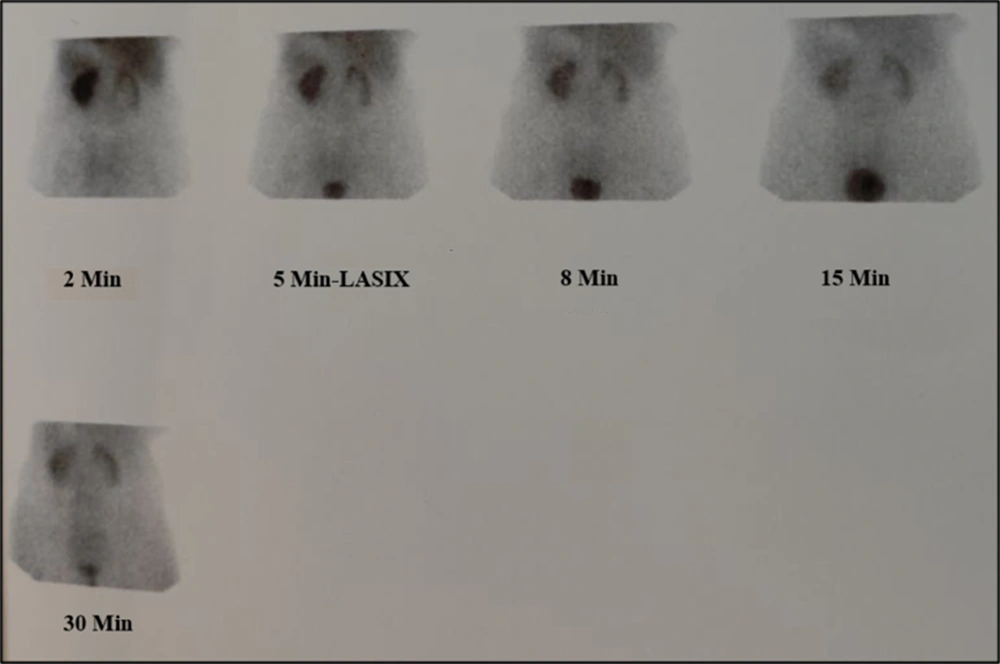
Finally, after the referral to the urologist, an intravenous pyelogram (IVP) was performed that no evidence of contrast of the right pyelocaliceal system and ureter was observed (Figure 1). Also, a nuclear scan was done that decreased perfusion and right kidney function were observed with evidence of mechanical obstruction (Figure 2). These points can suggest ureteral obstruction due to hydronephrosis and lack of stone in the right kidney. Finally, the patient was a candidate for surgery with a possible diagnosis of ureteral obstruction.
A CT with contrast after IVP. Contrast injection after 10 minutes, the left kidney has a proper secretion and the pyelocaliceal system is normal (arrows) and without dilation. The left kidney has no enhancement contrast (A). Contrast injection after 1 hour, the left kidney is normal and contrast material is seen inside the bladder (arrows), but still, the right pyelocaliceal system is not observed and the right kidney has a small amount of cortical enhancement, which indicates a delayed secretion and possibly obstruction in the right kidney (B).
The left kidney showed proper flow and cortical activity. Tracer accumulation in the pyelocaliceal system and ureter of this kidney responded well to Lasix injection. The right kidney showed severely decreased flow and cortical activity. Tracer accumulation in the pyelocaliceal system of this kidney didn’t respond to Lasix. DRF: RK = 34%, LK = 66%
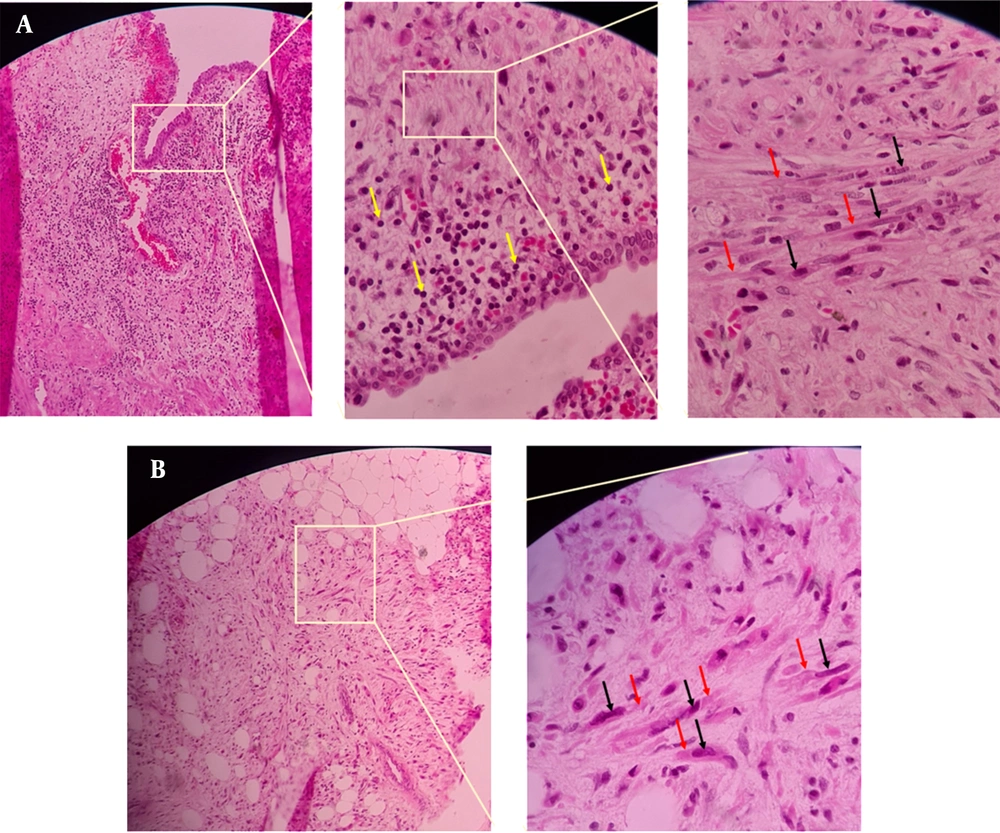
Open surgery was performed to repair the ureter. There were severe adhesions and fibrosis in the retroperitoneal adjacent to the implant of the lumbar vertebra so that even was engaged IVC. Fibrosis was isolated, also the 1.5 cm of upper ureteral stenosis was eliminated, and both were sent for pathology. Pathological results show fibrosis and inflammation of the ureter tissue and retroperitoneal fat (Figure 3). The right kidney was slightly released and was brought down to prevent tension. Then upper ureter was anastomosed end-to-end and Double J was placed. The ureteral anastomosis site was covered with a flap of perinephric adipose tissue to prevent re-fibrosis. The postoperative course was uneventful in follow-ups and the patient was discharged home on day 3 after the surgery.
3. Discussion
This report explained a rare case of ureteral obstruction caused by retroperitoneal fibrosis that has been created by an injury via PLIF surgery after five years. In this patient, the ureteral obstruction was successfully treated by end-to-end anastomosis of the ureteral and then covered with a flap of perinephric adipose tissue.
Although PLIF has been introduced as a minimally-invasive surgery, the ureter is surrounded by retroperitoneal fat and protects against injury, so there are a limited number of reports of ureteral injury (2-6). For example, its first case was described by McKay et al. in 1954 (3). Moreover, Cho et al. in their study in 2008 have stated that posterior lumbar surgeries that involve the disk space such as discectomy and PLIF, have potential risks for ureteral injury (4). In another study, Hajiha et al. in 2017 have documented a case of ureteral injury following posterior lumbar discectomy. They introduced the patient's lean with lack of retroperitoneal fat as an effective factor on increasing the risk of ureteral injury during posterior discectomy (5). Additionally, Pillai et al. in 2013 have reported a case of ureteral injury after posterior lumbar discectomy with interbody screw fixation on postoperative day 10 (6). The timing of the diagnosis in most of the reported cases ranged from 3 days to 6 weeks after surgery (10, 11) while, in our case it has taken 5 years. In another research, Bjurlin et al. in 2009 have reported a case of iatrogenic ureteral injury after a thoracolumbar lateral fusion on postoperative day 14. In this regard, they have concluded that flank pain and urinoma after lateral thoracolumbar fusion should be considered as signs of ureteral injury (12). de Quintana-Schmidt et al. in 2011 have revealed a case of ureteral injury after L4-L5 microdiscectomy. Accordingly, they have observed deep bleeding during surgery process that was controlled well. After 36 hours, the patient showed an abdominal distend and pain associated with anemia as well as an increase in WBC count, suggesting the ureteral injury (2). Furthermore, Patel et al. in 2021 have presented a case of ureteral injury after transforaminal lumbar interbody fusion on day 8 post-operation (13). In a systematic review, Turgut et al. in 2020 have concluded that ureteral injury is a complication of posterior lumbar spine surgery especially reported during discectomy (14).
In lean people, the space between the vertebra and the ureter is very slender because the ureter anatomically and immediately places on the anterior longitudinal ligament of the spinal between the body of the vertebra and the psoas muscle (15). Therefore, the ureter is vulnerable to be injured during PLIF surgery. While in obese people, retroperitoneal fat tissue maintains the ureter away from the intervertebral space, so it is protected against injury (15). The patient in the present study lost 15 kg weight within five years after surgery, so the tips of the screws probably affected the connective tissue around the ureter and led to its fibrosis. Another possible explanation for the fibrosis may possibly be that at the time surgery, the fibrosis was caused by manipulations or surgical instruments simultaneously, and also by undiagnosed or delayed microvascular injury, which may have remained hidden in the retroperitoneal adipose tissue.
The patient’s clinical findings may appear either during and/or immediately after surgery or occur with a delay. As well, the signs and symptoms are nonspecific. The patient in this research showed flank and abdomen pain resulted from high-grade ureteral obstruction. Of note, signs of abdominal ileus developed with nausea, vomiting, anorexia, and fever. In addition, Hydronephrosis was created due to the ureter compression by retroperitoneal necrotized tissue. It is noteworthy that ureteral injuries should be diagnosed more quickly via performing accurate physical and radiological examinations, including nuclear scan and CT scan, in order to protect nephro-ureteral structures.
4. Conclusions
The surgeon should pay attention to non-specific symptoms and signs related to ureteral injury such as flank and abdomen pain, nausea, vomiting, anorexia, and fever, after PLIF surgery, even if a long time has passed since the surgery. Paying enough attention to these possible complications leads to timely diagnosis and consequently protect nephro-ureteral structures.