1. Background
Although many studies have been conducted on the outcome of COVID-19 in different populations to determine risk factors, the effect of COVID-19 on dialysis patients is still under investigation (1). It has already been suggested that the kidney is one of the organs that can be targeted by SARS-CoV-2. Acute kidney injury can occur in nearly 30% of hospitalized COVID-19, which is higher than the incidence of acute kidney injury in similar airborne infectious diseases such as influenza (2, 3). Furthermore, SARS-CoV-2 has been isolated from podocytes that are proximal tubules, indicating a direct invasion of tubular cells by this virus (4, 5). Patients with end-stage renal disease (ESRD) are considered vulnerable to severe forms of infectious diseases. Dialysis patients mostly consist of the elderly population with various comorbidities and metabolic and endocrine imbalances (6). Managing dialysis patients with COVID-19 can also be challenging since many treatments need to be adjusted or removed from their regiment due to their impaired kidney functions. Furthermore, practicing social distancing is almost impossible for dialysis patients since they regularly visit and spend many hours in dialysis centers (1). In addition to these problems, patients on dialysis who are in line for a kidney transplant are usually immune-compromised and at risk of fastidious infections. Although dialysis centers take many protective measures to reduce these patients’ exposure to COVID-19 in dialysis centers, an outbreak of COVID-19 in dialysis centers seems inevitable, and all centers must be prepared for an internal outbreak (7, 8).
The outcome and course of COVID-19 in dialysis patients are still debatable. COVID-19 can have a different course in dialysis patients. For instance, studies suggest that dialysis patients are at risk of prolonged viremia (9). Mortality rates in the literature vary from 16% to 60%. Although studies from China indicated lower mortality rates at the beginning of the pandemic, similar reports from Europe and the USA suggested much higher mortality rates. Some of this inconsistency in studies can be attributed to the studies’ methodology, confounding factors, local SARS-COV-2 variants, and ethnic variations (10).
After the official report of the first COVID-19 case on the 19th of February in Iran, many protective measures were employed to provide a safe environment for dialysis patients and reduce infection risk in these patients. In addition to protective measures, one of the critical components of these programs was to gather information regarding COVID-19 infection and contact tracing to avoid COVID-19 outbreaks in dialysis centers. Herein, we report experiences of 4 dialysis centers, with a total of 309 patients from the beginning of the COVID-19 pandemic until the end of 2020. Two dialysis centers were in general hospitals (Baqiyatallah Hospital Dialysis Center and Besat Nahaja Hospital Dialysis Center), and the other 2 dialysis centers were in charitable clinics (Seyed al-Shohada Clinic and Imam Ali Clinic).
2. Objectives
This study aimed to compare mortality rates and associated factors that contribute to mortality in dialysis patients in the Iranian population.
3. Methods
3.1. Study Population, Protective Measures, Data Gathering, and Study Design
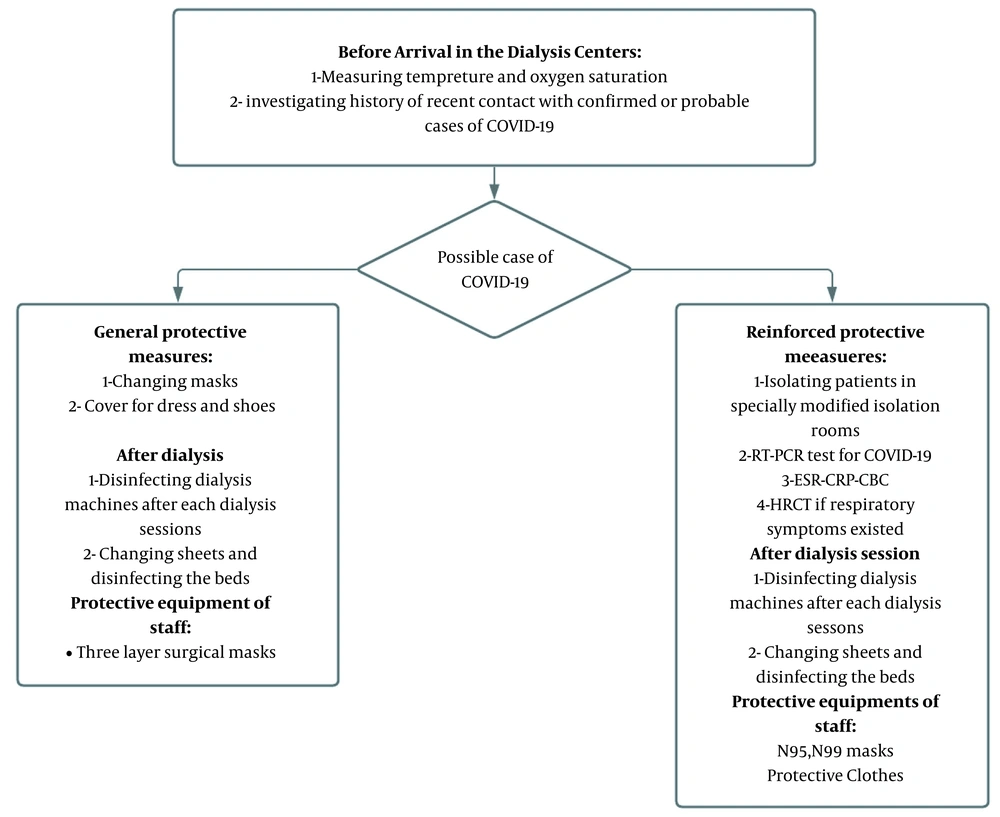
This cross-sectional study was conducted on 4 dialysis centers: Baqiyatallah Hospital Dialysis Center, Besat Nahaja Hospital, Imam Ali Clinic, and Seyed al-Shohada Clinic from February 2020 until the end of the year. This study was approved by the Ethics Committee of Baqiyatallah Hospital. During the pandemic, all COVID-19-related information, including the condition of patients and staff, symptoms, and history of contact with cases of COVID-19, was recorded because of the disease’s unknown nature. Confirmation of the first COVID-19 case in Iran resulted in an increase in the working hours of dialysis centers and the alternation of these centers’ schedules to avoid overcrowding of dialysis centers and unnecessary contacts during the pandemic. All staff and patients were obligated to wear masks and protective dresses during the dialysis session, and disinfectants were made available. Furthermore, the space between dialysis beds increased, and plastic covers separated the beds. Moreover, to prevent the spread of infection by hospital staff, each patient was assigned to only 1 nurse. The hospital beds and dialysis machines were disinfected after each session. All staff members were equipped with 3 layers of surgical masks and gloves. Furthermore, all staff members of the Baqiyatallah Hospital Dialysis Center were screened regularly for COVID-19 using polymerase chain reaction (PCR). In the case of symptom appearance, a positive COVID-19 test, or a history of contact in staff members, they would be sent home on leave. Before arriving at dialysis centers, the patients were questioned regarding the existence of any respiratory symptoms, fever, or fatigue. Furthermore, the O2 saturation and temperature were measured before entering the center. In the case of abnormal findings in medical examination or history of recent contacts with possible cases of COVID-19, patients were isolated in specially modified isolation rooms, and nasopharyngeal samples were tested for COVID-19. Blood samples were also tested for an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels and abnormal findings of blood count for lymphopenia. Patients with respiratory or other clinical symptoms with negative PCR also underwent high resolution computed tomography (HRCT) to confirm or rule out the diagnosis. Figure 1 summarizes protective measures and guidelines in the dialysis centers. All dialysis patients with confirmed COVID-19 were admitted to the hospital to prevent adverse outcomes of the disease. Most of these patients were referred and hospitalized in Baqiyatallah Hospital, which had turned into a COVID-19 center. The data of this study were collected from medical records in the dialysis centers and hospital documents of the patients.
3.2. Case Definition
Confirmation of COVID-19 was done according to the Iran Ministry of Health and Medical Education case definition. To confirm COVID-19 in patients, samples from nasopharyngeal swabs were tested for SARS-CoV-2 using PCR.
4. Results
Of 309 patients in the dialysis centers, 58 patients (31 males and 27 females with an average age of 60.94 years with an SD of 15.58) contracted the disease (18.7%) at the time of this study. Unfortunately, 24 of the 58 patients died due to COVID-19 (41.4% mortality rate as demonstrated in Table 1).
| Dialysis Center | Total Patients (N = 309) | Patients Who Contracted COVID-19 (n = 58); No. (%) | Number of Patients Who Did Not Survive (n = 24) | Mortality Rate (%) |
|---|---|---|---|---|
| Seyed al-Shohada Clinic | 35 | 7 (20) | 1 | 14.3 |
| Imam Ali Clinic | 120 | 28 (23.3) | 17 | 60.7 |
| Besat Nahaja Hospital | 44 | 5 (11.3) | 2 | 40 |
| Baqiyatallah Hospital | 110 | 18 (16.3) | 4 | 22.2 |
| Total | 309 | 58 (18.7) | 24 | 41.4 |
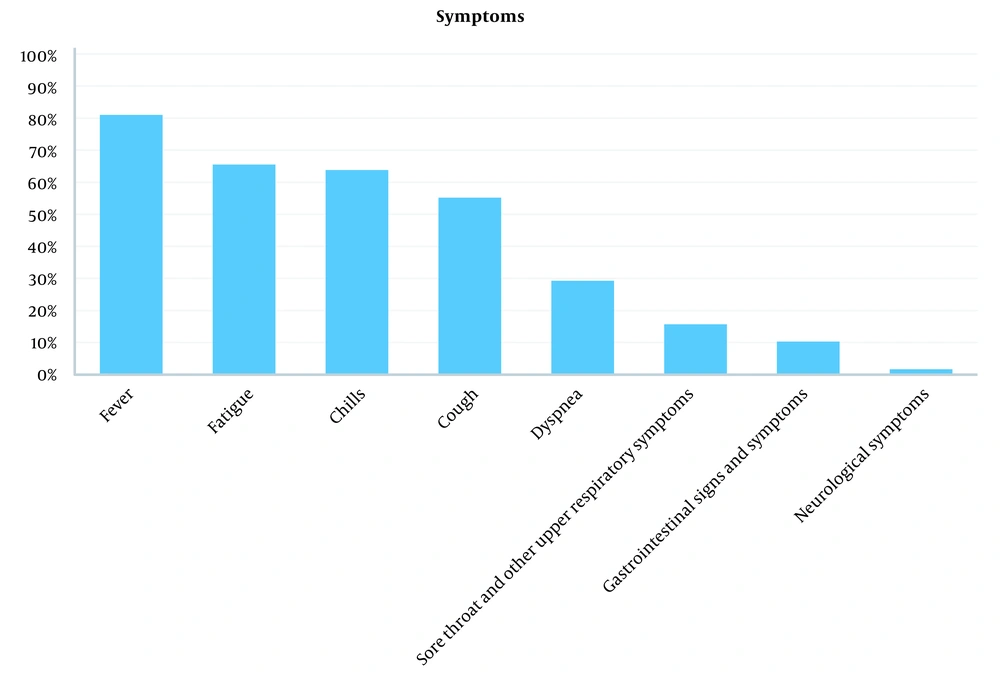
As demonstrated in Figure 2, the most common symptom in the patients was fever (81%), followed by fatigue (65.50%), chills (63.80%), dry cough (55.2%), dyspnea (29.30), and upper respiratory symptoms such as sore throat (15.70%). Furthermore, 15.70% of patients experienced gastrointestinal symptoms. In 1 patient, the most prominent symptoms were headache and vertigo.
Table 2 demonstrates the characteristics that can influence the mortality rates in dialysis patients. It was observed that patients who did not survive COVID-19 were significantly older than the other dialysis patients. Furthermore, it was observed that dialysis vintage and sex are not significantly associated with higher mortality rates. These results can be due to the low sample size of the study and can change in observations with higher sample sizes. To evaluate the effect of multiple comorbidities on the severity of the disease, we selected the Charlson comorbidity index (CCI), which has been widely used to compare the effect of different comorbidities in various studies, including COVID-19-related studies (11). It was observed that CCI is significantly higher in patients who did not survive (P < 0.05).
a Values are expressed as mean ± SD.
b Independent t-test.
c Mann-Whitney test.
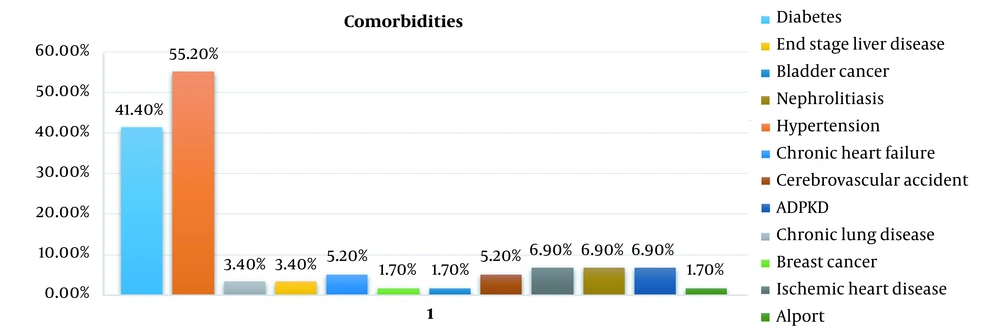
The most common comorbidity among these patients was hypertension (55.20%), followed by diabetes (41.40%). The comorbidities of dialysis patients are presented in Table 3 and Figure 3. Seven patients had an abnormal heart condition (heart failure and coronary artery disease), 2 patients had liver cirrhosis, 2 patients had chronic lung disease, 3 patients had a previous history of cerebrovascular accident, and 4 patients had a previous history of autosomal dominant polycystic kidney disease (ADPKD) and nephrolithiasis. Furthermore, 2 patients were under treatment for malignancies (breast cancer and bladder tumor). As demonstrated in Table 3, mortality rates were significantly higher in dialysis patients with diabetes than in other patients. Furthermore, it was observed that hypertension also could be associated with a higher mortality rate in dialysis patients, but it was not significant enough to come up with a decisive conclusion.
| Comorbidities | Patients Who Did Not Survive | Survived Patients | Significance a (P Value < 0.05) | Odds Ratio | CI (95%) | ||
|---|---|---|---|---|---|---|---|
| Had Comorbidity | Did Not Have Comorbidity | Had Comorbidity | Did Not Have Comorbidity | ||||
| Hypertension | 16 | 8 | 16 | 18 | 0.139 | 2.25 | 0.76 - 6.6 |
| Diabetes | 15 | 9 | 9 | 25 | 0.006 | 4.6 | 1.5 - 14.2 |
| Chronic heart failure and ischemic heart disease | 3 | 21 | 4 | 30 | - | - | - |
| End-stage liver disease | 2 | 22 | 0 | 34 | - | - | - |
| Chronic lung disease | 1 | 23 | 1 | 23 | - | - | - |
| Cerebrovascular accident | 2 | 22 | 0 | 34 | - | - | - |
| Nephrolithiasis | 1 | 23 | 3 | 31 | - | - | - |
| Autosomal dominant polycystic kidney disease | 1 | 23 | 3 | 31 | - | - | - |
| Breast cancer | 1 | 23 | 0 | 34 | - | - | - |
| Bladder cancer | 1 | 23 | 0 | 34 | - | - | - |
a Chi-square test.
5. Discussion
According to the results of this study, the mortality rate was significantly higher in dialysis patients than in the general population. This study’s mortality rate was 41%, while official reports in Iran indicate that the general population’s mortality rate is near 4.7%. Understanding the current situation regarding dialysis patients requires understanding the course of COVID-19 in Iran. Although the first COVID-19 case was officially reported on the 19th of February in Qom, several unofficial reports in mid-February suggested that the COVID-19 had already been entered the country. The first surge in the COVID-19 epidemic in Iran began in early March and continued until the middle of April. Restrictions from the 20th of March to the third of April resulted in a significant decline in the number of cases. The second wave of the COVID-19 pandemic, which caught the Iranian health care system off-guard, began in June and continued until mid-August. In September 2020, the burned-out health care system was challenged by the third wave of the pandemic. This wave was far more immense than the second and first wave of the pandemic, resulting in a 2-week lockdown in several Iran cities. Even before the outbreak of the COVD-19 pandemic in Iran, many dialysis centers, including the 4 centers studied in this study, had already prepared for the COVID-19 outbreak by composing internal guidelines and equipping staff with protective equipment. Furthermore, many dialysis patients, especially patients on the transplant list, had already been alerted regarding their condition and early signs of the disease. To prepare dialysis centers for an internal outbreak, at the beginning of the pandemic, extreme restrictions had been deployed to prevent the spread of COVID-19. It is worth noting that all of the COVID-19 cases in these 4 dialysis centers occurred in the pandemic’s third wave. This delay can be attributed to the advanced planning of dialysis centers. Furthermore, no major internal outbreaks occurred in these dialysis centers. To prevent the adverse outcomes of COVID-19, all the dialysis patients with COVID-19 were hospitalized without considering the severity of the disease.
The results of these studies indicated that several factors could contribute to the severity of the disease. It was observed that older age was significantly associated with higher mortality rates. CCI was significantly higher in dialysis patients who did not survive. Also, we observed that diabetes could be associated with higher mortality rates. Although the percentage of hypertension and male sex was higher in patients who did not survive, it was not significant. Even though not significant, the percentages of hypertension and male sex were higher in patients who did not survive. The overall incidence ratio of COVID-19 in the 4 dialysis centers was 18.7%, and the highest ratio was 23%. The incidence ratio of COVID-19 in this study’s dialysis centers was similar to that reported in many other studies. In a French dialysis center with 200 patients, 38 contracted the disease, and the mortality rate was 21% (12). In another study in 4 dialysis centers in Brescia, 94 of the 643 patients contracted the disease (15%), and the mortality rate was 29% (13). Furthermore, in another study in the UK, 300 of the 1530 patients contracted the disease (14). As mentioned, the mortality rate in dialysis patients was near 40% (which was much higher than the general population), but additional comorbidities and patients’ age also contributed to high mortality rates. Reports from Japan have indicated that the mortality rate in dialysis patients is near 30%, which is 1.6 times higher than the general population. The high mortality rates of this study were also attributed to older age and comorbidities (15). Interestingly, no dialysis patients succumbed to the disease in the early stages of the pandemic. Some studies have suggested that due to COVID-19 phobia and lower rates of burn-out in the early stages of the pandemic, more people followed the preventive guidelines (16, 17). In the study by Goicoechea et al, the mortality rate among 36 patients was also near 36% (18). Furthermore, in this study, dialysis vintage was associated with higher mortality rates. However, in our study, no significant association between dialysis vintage and higher mortality rates was found. The relatively small sample sizes of these studies can be the reason for this disagreement. Further studies with a larger sample size in this area must be conducted. In another study, among 419 ESRD patients, the mortality rate was 31.7%, and comorbidities such as diabetes, hypertension, and male sex were associated with higher mortality rates (19). The French national end-stage kidney disease epidemiology and information network (REIN) tracked the record of patients on dialysis who were infected with SARS-CoV-2. These data suggested that comorbidities such as diabetes were also associated with higher mortality rates in COVID-19 patients. In the REIN database, the mortality rate among 1621 infected patients was around 21% (20). The database of European Renal Association - European Dialysis and Transplant Association (ERA-EDTA) has also suggested that the patient in line for kidney transplants have higher mortality rates than the dialysis patients. In this study, the mortality rate in dialysis patients was about 21% (21).
In the current study, the mortality rate of the dialysis patients was higher than the general population, which is in line with many other similar reports. Although several vaccines have been developed, with the emergence of new COVID-19 variants (such as omicron) and obstacles in developing a proper treatment agent, the number of patients with COVID-19 is still rising daily. Patients on dialysis are one the most susceptible groups to infectious disease. Since ESRD is more common in the elderly, dialysis patients have several risk factors that make them one of the most vulnerable groups in pandemics. Furthermore, several protective measures, such as isolation at home, cannot apply to these patients. Thus, conducting studies and sharing experiences can be an excellent tool for composing future guidelines for future pandemics based on our experience in the current pandemic. It is also worth mentioning that chronic kidney disease (CKD) has already been associated with higher mortality rates in patients with kidney disease (22). However, it has been suggested that the mortality rates can be higher in patients with CKD than in patients under renal replacement therapy (23). These findings suggest that other risk factors can contribute to high mortality rates in patients on dialysis. This study had several limitations. Due to the nature of the study, the sample size was not large enough. Further studies in this area are needed to provide a full picture of the possible effect of COVID-19 on kidneys.
5.1. Conclusions
The current study suggests that although mortality rates are higher in dialysis centers than in the general population, these rates could be quite different in various dialysis centers. Furthermore, it was observed that although many of the dialysis patients were exposed to COVID-19, the incidence ratio in dialysis centers was lower than what was expected. The reasons could be that the dialysis patients had already been familiar with many protective measures, and many dialysis centers had already been equipped with isolation rooms and other protective equipment. Furthermore, regular screening for all staff members for COVID-19 can also be effective in reducing the chance of transmission of the disease from asymptomatic staff. In conclusion, the results of this study emphasize the preventive measures for dialysis patients since they are one of the more susceptible groups to COVID-19.