1. Background
The management of urolithiasis has been remarkably transformed over the years. Nowadays, open surgery for nephrolithiasis is almost replaced by percutaneous nephrolithotomy (PCNL), introduced in the 1970s. The evolvement of mini PCNL has further led to the more frequent use of percutaneous methods, even for calculi of < 2 cm. Mini PCNL has lower morbidity rates due to decreased bleeding and postoperative pain. However, its value is under continuous deliberation (1-3).
Extracorporeal shock wave lithotripsy (ESWL), the first treatment of choice for small-to-medium-sized kidney stones, has a questionable charm owing to patient reluctance for repeated treatments and hospitalizations since ESWL has a reduced stone-free rate (SFR). This has led to considering a potentially less invasive option of percutaneous methods such as retrograde intrarenal surgery (RIRS), initially used to treat lower calyceal stones resistant to ESWL (1). The RIRS modality is used as a primary technique to treat lower calyceal calculi, and it may potentially obtain higher SFR than ESWL with lower morbidity rates than percutaneous techniques, especially for low-volume calculi.
2. Objectives
The present study compared ESWL, mini PCNL, and RIRS for managing lower pole renal calculi of < 1.5 cm.
3. Methods
This hospital-based observational study encompassed all patients with renal stones < 1.5 cm diameter and < 1000 HU density who underwent mini PCNL, RIRS, or ESWL in the Department of Urology and Renal Transplant from January 2020 to July 2021. The study was approved by the Institutional Ethics Committee affiliated with the Dr. Ram Manohar Lohia Institute of Medical Sciences (code: IEC 49/19).
Inclusion criteria were lower pole renal calculi of < 1.5 cm without prior intervention and willingness to participate in the study. On the other hand, the following patients were excluded from the study: Patients with lower pole renal calculi of > 1.5 cm, those with upper/mid pole calculus, ASA III/IV patients, patients with comorbidity, including uncontrolled hypertension/diabetes/coronary artery diseases, and morbidly obese patients (BMI > 40).
3.1. Procedures
Data were collected from all the patients undergoing standard mini PCNL, RIRS, or ESWL in our department. The patient's detailed history and physical examination were recorded, and all routine investigations, including Hb%, TLC, DLC, ESR, RBS, Urine-R/M, Urine-C/S, blood urea, serum creatinine, serum electrolytes, BT, CT, ECG, and Chest X-ray were carried out. A CT urogram was performed on all the patients before the procedure. They were also informed of the procedures and voluntarily participated in the study; hence, their informed consent was obtained.
Mini PCNL was performed using a 12F nephroscope (Karl Storz) and an 18 F sheath. A Holmium achieved stone fragmentation: YAG 200 µm laser fiber at the settings of the 0.5 Joules x 15 Hertz frequency rate for dusting and the 1 Joule x 10 Hertz frequency rate for fragmenting. Intra-operative parameters (e.g., operative time, blood loss during surgery, pneumothorax, hydrothorax, hemothorax, and adjacent organ injury) and postoperative parameters (e.g., wound infection, urinary leakage, bleeding, septicemia, length of hospital stay, and analgesic requirement) were recorded. Moreover, X-ray KUB and NCCT KUB were performed on the first POD and after one month, respectively.
All RIRS cases were pre-stented 14 days before the procedure and performed under general anesthesia. The 8.5 Fr URF-V2R & V3R flexible scope of Karl Storz was primarily used in all cases. Fragmentation was achieved using Ho: YAG Laser with 200 µm fiber until all calculi were considered clinically insignificant fragments. Double J stent 6F 26 cm was deployed in all patients. If the postoperative period was uncomplicated, the patient was sent home on the second day with oral antibiotics.
In the ESWL group, pre-procedure preparation consisted of Dulcolax 2 tablets, charcoal 4 tablets the night before post-dinner, and analgesic medication in the form of diclofenac 100 mg intramuscular injection 30 minutes before the ESWL session. Dornier Compact Sigma lithotripter, a third-generation electromagnetic lithotripter, was used, and ultrasound performed stone focusing and monitoring. The standard focal length of the lithotripter was 14 cm, and the focal zone was 4.7 × 5.7 mm. The shock wave was set at a rate of 60 shocks/minute, with the intensity starting at level 1 and gradually increasing to the next level after 500 shocks as long as it reached level 3. The treatment protocol included 3000 shockwaves in each session or until the stone was completely fragmented, whichever occurred earlier. Post-ESWL instructions included physical rest for one day and plenty of oral fluids to pass urine through a strainer to collect stone fragments. The patients were explained about possible complications. Appropriate analgesics, antibiotics, and alfa-blockers were routinely prescribed to all patients. All patients were instructed to report any treatment-related complications, which were meticulously recorded.
4. Results
Out of 160 cases, 111 (69.30%) were males, including 44 (73.3%) in the mini PCNL group, 26 (65%) in the RIRS group, and 41 (68.3 %) in the ESWL group. Of the 49 female patients, 16 (26.7%) were in the mini PCNL group, 14 (35%) in the RIRS group, and 19 (31.7%) in the ESWL group. The RIRS, mini PCNL, and ESWL groups included 40, 60, and 60 patients, respectively. There was no significant difference in mean age among the groups (42.12 ± 11.02 years in the RIRS group, 41.5 ± 13.20 years in the mini PCNL group, and 38.9 ± 15.32 years in the ESWL group) (Table 1).
| Characteristics | ESWL (n = 60) | Mini-PCNL (n = 60) | RIRS (n = 40) | P-Value |
|---|---|---|---|---|
| Age, y | 38.9 ± 15.32 | 42.12 ± 11.02 | 41.5 ± 13.20 | 0.095 |
| Male/female | 41/19 | 44/16 | 26/14 | 0.19 |
| Left side | 31 (51.7) | 34 (56.7) | 18 (45) | 0.121 |
| BMI | 26.35 ± 4.13 | 26.99 ± 4.56 | 25.52 ± 3.51 | 0.111 |
| Stone size | 10.93 ± 3.13 | 12.99 ± 3.56 | 10.62 ± 2.51 | 0.854 |
Patients' Characteristics a
All three groups had similar numbers of right and left stones. Regarding the 40 patients in the RIRS group, the left-side procedure was performed in 18 (45%) patients and the right-side procedure in 22 (55%). Considering the 60 patients in the PCNL group, the left-side procedure was performed in 34 (56.7%) patients and the right-side procedure in 26 (43.3%). Regarding the 60 patients in the ESWL group, 31 (51.7%) were left-sided. There were no significant differences in BMI among the mini PCNL, RIRS, and ESWL groups (Table 1).
The mean sizes of the stone in the mini PCNL, RIRS, and ESWL groups were 12.99 ± 3.56 mm, 10.62 ± 2.51 mm, and 10.93 ± 3.13 mm, respectively. There was no significant difference in the stone size among the groups (Table 1).
In our study, stone density was 866.41 ± 352.3 HU in the mini PCNL group, 830.22 ± 298.25 HU in the RIRS group, and 808.3 ± 321.2 HU in the ESWL group; however, the difference was not significant (P = 0.055) (Table 2).
| Characteristics | ESWL (n = 60) | Mini PCNL (n = 60) | RIRS (n = 40) | P- Value |
|---|---|---|---|---|
| Duration of procedure, min | 136.40 ± 19.3 | 32.3 ± 12.65 | 51.2 ± 8.63 | 0.013 |
| Stone density, HU | 808.3 ± 321.2 | 866.4 ± 352.3 | 830.2 ± 298.3 | 0.055 |
| Reduction in Hb, mg/dL | 0.21 ± 0.17 | 0.61 ± 0.10 | 0.27 ± 0.15 | 0.058 |
| Ancillary procedure | 11 (18.33) | 1 (1.7) | 6 (10) | 0.031 |
| Duration of hospital stay, days | 0.13 ± 0.05 | 3.07 ± 1.6 | 3.02 ± 0.65 | 0.041 |
Operative Parameters a
The operative time was 32.3 ± 12.65 min in the mini PCNL group, 51.2 ± 8.63 min in the RIRS group, and 136.40 ± 19.3 min in the ESWL group. In this regard, the difference was significant (P = 0.013) (Table 2).
In our study, the hemoglobin decrease was 0.61 ± 0.10 mg/dL in the mini PCNL group, 0.27 ± 0.15 mg/dL in the RIRS group, and 0.21 ± 0.17 mg/dL in the ESWL group. The difference between the three groups was significant, though it was borderline (Table 2).
Out of 60 patients in the mini PCNL group, only one (1.7%) required an ancillary procedure; out of 40 patients in the RIRS group, only six (10%) required an ancillary procedure, and out of 60 patients in the ESWL group, 11 (18.33%) required ancillary procedure (Table 2). In this regard, the difference was significant (P = 0.031).
In our study, hospital stay was 3.07 ± 1.6 days in the mini PCNL group, 3.02 ± 0.65 days in the RIRS group, and 0.13 ± 0.05 days in the ESWL group (Table 2).
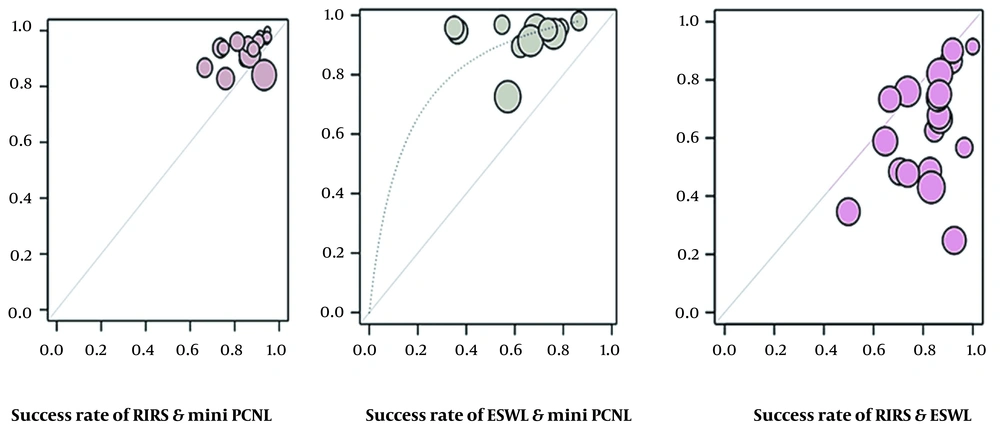
In our study, the SFR of the mini PCNL group was significantly higher than those of the other groups: 59 (98.3%) in the mini PCNL group, 34 (85 %) in the RIRS group, and 46 (76.7%) in the ESWL group. In this regard, the difference was significant (P = 0.002) (Table 3, Figure 1).
| Groups | Number of Patients | Stone-free Rate; No. (%) | P-Value |
|---|---|---|---|
| Mini PCNL | 60 | 59 (98.3) | 0.002 |
| RIRS | 40 | 34 (85 ) | |
| ESWL | 60 | 46 (76.7) | |
| Total | 160 | 139 (86.9) | - |
Stone-free Rates Among the Groups
Regarding complications, out of 60 patients in the mini PCNL group, 41 (68.3%) had no complications, 14 (23.3%) were in grade 1, and five (8.4%) were in grade 2. Out of 40 patients in the RIRS group, 33 (82.5%) had no complications, four (10%) were in grade 4, two (5%) were in grade 2, and one (2.5%) was in grade 3. Out of 60 patients in the ESWL group, 50 (83.3%) had no complications, and 10 (16.7%) were in grade 1 (Table 4).
5. Discussion
The comparison of the mini PCNL, RIRS, and ESWL is quite interesting, especially for solitary lower pole renal stones of 10 - 20 mm. In this regard, our comparative study analyzed patient characteristics, stone parameters, and procedure-related factors. This goal was achieved by balancing all the above-mentioned parameters.
Aboutaleb et al. (4) and El-Nahas et al. (5) suggest that ESWL has some advantages, such as being an outpatient procedure, better patient acceptance, and minimal anesthesia requirement, making it the most preferred treatment technique for lower pole renal stones of < 20 mm. Sener et al. (6) and Shah (7) concluded that with improved fiber optics and the availability of small-sized instrumentation developing, i.e., RIRS, relying on the advantages of a higher stone-free rate (SFR) with less bleeding and lower risk of renal damage for renal calculi smaller than 20 mm has gained more popularity. Our study also showed the SFRs of 98.3%, 85%, and 76.7 % (P = 0.002) for mini PCNL, RIRS, and ESWL, respectively (Table 3). In our study, stone density was 866.41 ± 352.3 HU in the mini PCNL group, 830.22 ± 298.25 HU in the RIRS group, and 808.3 ± 321.2 HU in the ESWL group; however, the difference was not significant (P = 0.055) (Table 2).
Our study showed that the operative time was 32.3 ± 12.65 min in the mini PCNL group, 51.2 ± 8.63 min in the RIRS group, and 136.40 ± 19.3 min in the ESWL group, with their difference being significant (P = 0.013) (Table 2). Similarly, a review study by Schuster et al. (8) indicated that the operative time of PCNL was shorter than that of RIRS. In contrast to our findings, Havel et al. (9) reported that ESWL offered the shortest operative time among the three therapies because of its non-invasive nature, as it was considered only for a single session.
In our study, the hemoglobin decrease was 0.61 ± 0.10 mg/dL in the mini PCNL group, 0.27 ± 0.15 mg/dL in the RIRS group, and 0.21 ± 0.17 mg/dL in the ESWL group. The difference among the three groups was significant, though mild (Table 2).
Out of 60 patients in the mini PCNL group, only one (1.7%) required an ancillary procedure; out of 40 patients in the RIRS group, only six (10%) required an ancillary procedure, and out of 60 patients in the ESWL group, 11 (18.33%) required ancillary procedure (Table 2). In this regard, the difference was significant.
In this study, the SFR of the mini PCNL group was significantly higher than those of the other groups: 59 (98.3%) in the mini PCNL group, 34 (85 %) in the RIRS group, and 46 (76.7%) in the ESWL group. In this regard, the difference was significant (P = 0.002). De et al. (10) noted that SFR occupies a key parameter in estimating the efficacy of stone operation procedures. Some studies have estimated that the highest SFR in the renal pelvis or ureteropelvic junction for single calculus ranged from 80% to 88% (11, 12), and when stones were located in the lower pole, it dropped below 50 - 70% (13). Accordingly, it was pointed out that with ESWL for the lower pole renal stones, the SFR was dependent on anatomic features. However, SFR in the present study ranged from 48.6% to 77.9%, and others believed that PCNL reached the highest SFR for these stones; however, it was the most invasive technique among the three treatment techniques according to Sari et al. (14). Some other studies (15) also revealed that PCNL had a high success rate for all stone sizes in lower pole renal stones because of its high SFR (Table 3 and Figure 1).
Regarding complications, out of 60 patients in the mini PCNL group, 41 (68.3%) had no complications, 14 (23.3%) were in grade 1, and five (8.4%) were in grade 2. Out of 40 patients in the RIRS group, 33 (82.5%) had no complications, four (10%) were in grade 4, two (5%) were in grade 2, and one (2.5%) was in grade 3. Out of 60 patients in the ESWL group, 50 (83.3%) had no complications, and 10 (16.7%) were in grade 1 (Table 4). This result was in contrast to other studies, in which PCNL had a higher complication rate than RIRS at the expense of higher blood loss and longer hospital stays. In their review study, Zhang et al. (16) concluded that the overall rate of complications was quite comparable to the three management methods, consistent with the present study's findings. These inconsistencies in findings might have been caused by factors such as small sample sizes or the size of the participants' stones.
In our study, hospital stay was 3.07 ± 1.6 days in the mini PCNL group, 3.02 ± 0.65 days in the RIRS group, and 0.13 ± 0.05 days in the ESWL group (Table 2), and the difference was significant (P = 0.041). Similarly, Zhang et al. and De et al. (10, 16) reached the same findings in terms of hospital stay, while other researchers expressed the view that PCNL had the longest hospital stay and ESWL possessed the shortest hospital stay.
Srisubat et al. (17) presented a comparative Cochrane analysis of three management methods for nephrolithiasis. Although ESWL had the lowest success rate, the other two modalities were quite comparable. Also, ESWL patients had shorter hospital stays. In this study, it was found that making a patient SFR in one session was quite possible. This study was criticized for the low data quality of the stipulated studies, as only three were used for meta-analysis. Accordingly, our observations would profoundly affect decisions on managing lower pole renal stones, especially those of < 15 mm. However, there is still controversy on the optimum treatment of choice for lower pole calculus lingers, and further studies are required to reach a consensus. Well-designed RCTs and high-quality retrospective case-control series with less heterogeneity regarding patient factors and stone parameters would provide deeper insights in this regard.
5.1. Limitations of the Study
The study had a few limitations, including the small-sized and non-randomized sample; hence, bias can occur as the selection of cases was made by patients' choice. Also, ESWL is a non-invasive modality and a natural choice for most patients; however, the tolerance of each patient varies. Moreover, RIRS or mini PCNL is an operator/armamentarium-dependent procedure; hence, the findings may vary.
5.2. Conclusions
The present study concluded that, for lower pole renal calculi of < 1.5 cm, mini PCNL has the highest stone-free rate, followed by RIRS and ESWL. Also, ESWL offers a longer operative time than mini PCNL and RIRS. The ancillary procedure rate in the ESWL procedure was 18.33%, which is higher than those of mini PCNL (1.7%) and RIRS (10%). However, ESWL is confirmed to have the lowest SFR, a higher retreatment rate, and an ancillary procedure rate. This is because it has fewer complications and shorter hospital stays and is the procedure of choice by patients due to its non-invasive nature. In general, the complication rates among the three techniques are the lowest in the ESWL group, while it is comparable to those of the mini PCNL and RIRS groups. When urologists choose these treatments, they must individualize cases depending on patient characteristics and modality advantages, which are unique to each management modality.