1. Background
Chronic internal non-infectious diseases are hard to treat and chronic prostatitis is one of them. Among middle-aged men, prostatitis/chronic pelvic pain syndrome (CP/CPPS) is the leading cause of urological counseling and outpatient clinic visits (1). As young and middle-aged men are more likely to develop chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) the use of surgical procedures is not recommended (2). Therefore as a prostate cannot be operated and there are no drugs that can reach this organ easily, it is a common view that patients with CP/CPPS should get phenotype drive therapy (3).
The lack of effective medical therapy for CP/CPPS, like nonsteriodal anti-inflammatories, alpha-blockers, antimicrobial therapy, and 5a-reductase inhibitors, has led to various attempts to use alternative therapies, phytotherapy, cannabis, acupuncture, physical therapy, and psychosocial factors (4, 5). Spicy food, coffee, alcoholic beverages and strong tea can exacerbate the symptoms CP/CPPS while other nutrients, such as psyllium, water, herbal teas, and polycarbophil, can improve condition of patients with this disorder (6). Eating habits such as “frequency of eating fast food” may lead to significant negative impact on the symptoms of CP/CPPS (7). However, there is no association has been found between major lifestyle factors (obesity, smoking and hypertension) and CP/CPPS disease risk (8).
Chinese herbal medicine for chronic prostatitis is used frequently and more importantly this mono-therapy is safe (9). Shoskes (10) in his review in 2002 has noticed that among plentiful herbal treatments the promising include zinc, cernilton (bee pollen), quercetin, and saw palmetto. About 69% of pollen extract patients showed a 25% improvement compared to 48.5% of placebo patients has shown the clinical trial published in 2009 (11). Thus, pollen extracts (Cernilton) compares favorably to other phytotherapeutics agents: quercetin, and saw palmetto (Serenoa repens) (12).
Physical therapies for CP/CPPS have shown that patients responded to myofascial physical therapy (MPT) and global therapeutic massage (GTM), 57% vs. 21% accordingly. Furthermore it was noticed that men with CP/CPPS responded in a more positive fashion to GTM provided by female physical therapists (13). Different psychosocial factors may play substantial role on men with CP/CPPS, such as stress, personality factors, social aspects as well as different psychiatric co-morbidities (depression, anxiety and trauma-related disorders, somatization disorder, substance abuse); and affect their quality of life - QoL (14).
Thermobalancing therapy (TT) enabled by physiotherapeutic device has demonstrated improvement of QoL in men with CP/CPPS (15). TT has been implemented for termination of “micro-focus” of hypothermia following the constriction and spontaneous expansion of capillaries in the prostate tissue, i.e., the main trigger of chronic prostatitis. This described changes lead to increased pressure in the prostate gland, thereby causing the symptoms of CP/CPPS (16).
There were reported positive outcomes after acupuncture that can decrease pain, improve quality of life and potentially modulate inflammation (17). The review of published randomized control trials that compared the efficacy of acupuncture with sham acupuncture or standard medical treatment for patients with CP/CPPS observed that it has better efficacy (18). However different studies have found specific effects associated with acupuncture last at least over the short term, so acupuncture has relatively short-term physiological effects (19, 20).
Dr. Allen’s therapeutic device (DATD) that provides TT has shown its efficacy in men with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia decreasing prostate volume and LUTS by improving blood circulation in prostate (21, 22).
2. Objectives
The aim of this study is to confirm that TT is a unique independent treatment for CP/CPPS by assessing the dynamics of pain and QoL, PV, and Qmax.
3. Methods
3.1. Ethical Approval of the Study Protocol
The ethics committee of Yerevan State Medical University (Yerevan, Armenia) approved the study protocol. All participants provided written informed consent to be included in the study.
3.2. Study Design
This was an observational clinical controlled study undertaken in 2013 - 2015 that measured national institute of health chronic prostatitis symptom index (NIH-CPSI) scores for pain and quality of life (QoL), prostate volume (PV), and maximum urinary flow rate (Qmax) in 6-month, in one group of 45 patients who underwent TT and a control group of 45 patients that did not have such treatment, and compared these parameters between the two groups.
3.3. Participants
Over a 2-year period, 45 males (age < 55 years) with CP/CPPS (NIH category III) were selected for a clinical trial. Patients were selected in conjunction with urologists. Inclusion criteria were men with CP and NIH-CPSI pain score ≥ 1. Exclusion criteria were acute prostatitis, urethral stricture, neurogenic bladder, and comorbidities (e.g., impaired renal function, diabetes mellitus). We included patients with levels of prostate-specific antigen (PSA) in serum > 4 ng/mL for whom biopsy of the prostate gland showed no evidence of cancer. Medical treatments at the time of study enrolment were not taken into consideration.
3.4. Evaluation
Effectiveness of TT was studied by comparing men with CP/CPPS who received DATD as monotherapy with the control group (who received no treatment). Baseline evaluations comprised complete physical examination, medical history, digital rectal examination, serum biochemistry, PSA measurement, electrolyte levels, urinalysis and renal function tests. Evaluations were made at baseline and 6 months after treatment. At baseline assessment, patients were evaluated for various scores (NIH-CPSI pain/QoL), PV (mL) and uroflowmetry (Qmax; mL/s).
Dynamics of the symptoms and indicators in each group were assessed at the beginning and end of treatment using NIH-CPSI scores. Uroflowmetry was undertaken using a Sanuro2UL system (Santron Meditronic, Maharashtra, India). Ultrasound was used to determine the volume of the prostate gland by employing a US-9000E2 ultrasound scanner (Rising Medical Equipment, Beijing, China). The standard ellipsoid formula length × width × height × 0.52 was used to determine PV.
3.5. Statistical Analyses
The independent-samples t-test and paired-samples t-test are suitable only for interval and ratio data, so the Wilcoxon signed-rank test was employed. P < 0.05 was considered significant. Statistical analyses were carried out using SPSS v22 (IBM, Armonk, NY, USA).
3.6. Endpoints
Primary endpoints were changes in pain score and QoL score after 6 months of treatment. Secondary endpoints were changes in PV and Qmax after 6 months of treatment.
3.7. Thermobalancing Natural Treatment With DATD
DATD provides a method of treating an affected prostate gland by application of a special mixture of waxes (“thermoelement”) topically upon its projection. This thermoelement can accumulate the emitted body heat, and thus turn into a source of energy itself. In this way, DATD applies the thermoelement tightly to the coccyx, thereby overcoming the skin barrier and spreading heat energy towards the prostate gland (Figure 1).
Men who met the inclusion criteria of the study had treatment for CP/CPPS using DATD. In April 2010, DATD was registered at the Medicines and Healthcare Products Regulatory Agency as a class-1 medical device (23, 24).
4. Results
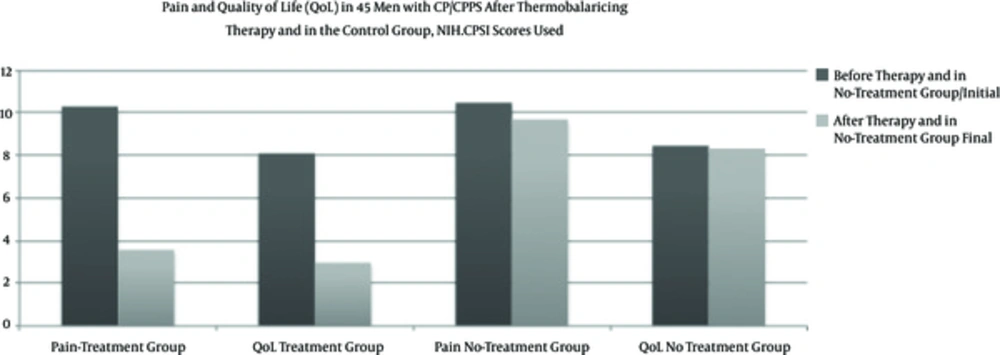
4.1. Pain Score and QoL
In the treatment group, the mean pain score decreased from 10.38 ± 2.53 to 3.58 ± 2.54 by the end of the study period at a significance level of P < 0.001. In the control group, the mean pain score decreased from 10.49 ± 2.46 to 9.71 ± 2, so slightly over the same period. Hence, there was a significant decrease in pain in the treatment group, whereas in the control group pain score decreased slightly.
In the treatment group, the mean QoL decreased from 8.11 ± 2.00 to 2.98 ± 1.80 at a significance level of P < 0.001. In the control group QoL score decreased slightly from 8.47 ± 1.92 to 8.33 ± 1.72. These results suggested that TT improved QoL significantly, whereas in the control group no changes in QoL.
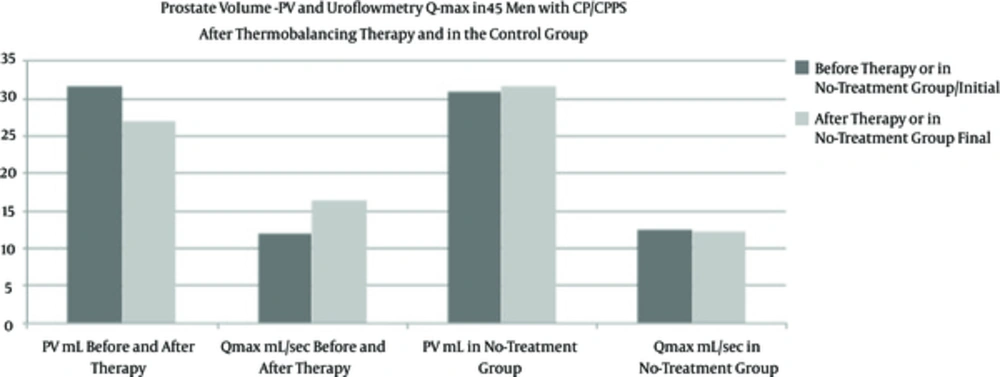
4.2. PV and Qmax
In the treatment group PV mL decreased from 31.75 ± 7 to 27.07 ± 4.52 at a significance level of P < 0.001. In the control group PV mL increased from 30.77 ± 6,43 to 31.58 ± 7.13 mL at the end of the study period. These data suggest that TT reduced PV significantly whereas, in the control group, PV increased.
In the treatment group Qmax mL/s, increased from 11.93 ± 4.344 to 16.45 ± 3.50 mL/s at a significance level of P < 0.001. In the control group Qmax decreased from 12.59 ± 3.57 to 12.20 ± 2.54 mL/s. These results suggest that TT increases Qmax significantly in CP/CPPS patients whereas, in the control group no changes in Qmax.
4.3. Side Effects TT and DATD
Side effects of TT with DATD were not observed in any patient.
5. Discussion
The present study showed that 6-month natural TT with DATD: (i) reduces pain and improves QoL; (ii) reduces PV and increases Qmax. We believe that TT is effective an independent treatment for CP/CPPS because treats the underlying cause of this chronic disease. DADT gradually reduces the size of inflamed prostate gland improving its functioning, decreases disturbing symptoms and increases urinary flow. Clinical improvement, including practical changes in the ultrasound/uroflowmetry parameters in patients with CP/CPPS who used DATD could be explained by changes in blood circulation at the capillary level. The continuous heat exposure from thermoelement that does not exceed the normal body temperature has terminated micro-focus of hypothermia and spontaneous expansion of capillaries. The similar positive effect has been seen while clinical trial on TT in men with enlarged prostate (25). DATD removes the vicious cycle of spontaneous growth of capillaries, thereby relieving pressure in the prostate gland and the CP/CPPS symptoms (26).
This clinical trial was not randomized because most men with CP/CPPS had psychological problems. Indeed, some scholars believe that psychological problems are a component of CP/CPPS (27). Blinding of patients/assessors to the study protocol was not possible because DATD had to be applied to participants and measurements taken. Thus this study was not a randomized. Having a “placebo” or “sham” group as controls could have provided more statistical rigor with regard to outcomes. However, in men with CP/CPPS largely unresponsive to medical interventions, greater pain is associated with diminished QoL (28). Therefore, proposing that men with CP/CPPS should wear a “placebo belt” for 6 months that does not alleviate symptoms would be very difficult. Usually, patients with CP felt symptom relief within weeks of wearing DATD, and used the device as required.
Physicians currently prescribe a wide range of medications, some of which have studied, and numerous of them have not been studied yet in randomized controlled trials (RCTs), however, none of them has shown high efficacy (29). Many new drugs for CP/CPPS treatment were found to be valueless (30, 31), and most commonly used drugs have adverse effects, especially when used in long-term (32). Zhang with colleagues investigated associations between lifestyle factors and CP/CPPS on a large number of men. However, no associations were observed between major lifestyle factors (obesity, smoking, and hypertension) and CP/CPPS (8). There is poor evidence supporting the efficacy of physical treatment options for CP/CPPS that include repetitive prostate massage or methods to apply energy to the prostate, so they remain controversial (33). Some researches reveal effectiveness of acupuncture for CP/CPPS and recommend applying it for managing pains of CP/CPPS with standard treatment options (34). However, there is no evidence for how long the effect after acupuncture lasts.
It should be noted that, contrary to conventional and alternative treatment options for CP/CPPS, TT stimulates the processes in prostate for prolong period of time, providing the treatment of its cause (35). The use of TT using DATD does not impede men’s day-to-day activity. Importantly, none of the patients who received TT suffered side effects and the cost of DATD compares favourably with the cost of conventional treatment. The present study shows effectiveness of new natural therapy for CP/CPPS which can be recommended as a new independent treatment for this chronic condition.
5.1. Conclusions
Six-month clinical study confirmed the ability of TT with DATD as a montherapy to reduce PV and pain, and improve QoL in men with CP/CPPS, therefore, this natural therapy should be recommended as an independent and traditional treatment option for these patients. The effectiveness of this therapy is in its capacity to influence the etiology of CP/CPPS.