1. Background
Percutaneous nephrolithotomy (PCNL) has become the mainstay of large renal stones (> 2 cm) treatment due to the remarkable rate of stone removal (1). Nonetheless, nowadays, minimal procedures, especially mini-PCNL and retrograde intrarenal surgery (RIRS), are at the center of stone management, which exhibits lower complications than previous methods (2, 3).
With several improvements in endoscopy technology, RIRS can be utilized as the choice in situations where PCNL is contraindicated or inferior to RIRS (4, 5). According to the recommendation of the European Association of Urology, RIRS can be considered the standard treatment for patients with small to medium size stones (6), and recently, satisfactory outcomes have been reached regarding applying RIRS in patients with larger stones (> 2 cm) (7). However, a low stone-free rate (SFR) and a high chance of stone recurrence limit the broad usage of RIRS in managing large renal stones (8, 9). In addition, it is essential to note that RIRS poses a tremendous financial burden on the healthcare system, especially in developing countries (10-12).
There is an ongoing challenge in managing renal stones in patients with overweight and obese. In these patients with large kidney stones, even though the safety of PCNL has been demonstrated, it has been shown that this procedure is accompanied by a longer duration of operation and length of hospital stay, a more poor SFR, and higher odds of necessitating retreatment (13, 14).
2. Objectives
Given the current trend toward more minor invasive procedures, exclusively RIRS in the management of renal stones, and the paucity of information concerning the outcomes of this procedure in obese patients, we designed a study to compare a different aspect of RIRS and PCNL in obese patients who had stones larger than 2 cm and smaller than 4 cm and treated at Sina Hospital during 2015 - 2018.
3. Methods
Eighty-two patients, who underwent PCNL and RIRS between June 2015 and December 2018 at the Department of Urology of Sina Hospital, were enrolled in our retrospective cohort study. The Ethics Committee of the Tehran University of Medical Sciences assessed and confirmed this study (IR.TUMS.SINAHOSPITAL.REC.1399.013) and the Iranian Registry of Clinical Trials (IRCTID: IRCT20190624043991N9). The patients with stones larger than 4 cm and smaller than 2 cm, age lower than 18 and higher than 75 years old, body mass index (BMI) lower than 30 and higher than 40 kg/m2, prior history of the renal stone procedure, and renal anatomic abnormalities were excluded from the study. All procedures were performed electively by the same surgeon. The obese patients were stratified into 2 groups based on the procedure: Group 1: Patients (n = 40) treated by PCNL; group 2: Patients (n = 42) whom RIRS treated. The choice of treatment modality was determined based on the surgeon and patient preferences.
The data of patients characteristics (age and gender), the kidney stones features (the size and the location), and operative and postoperative outcomes, including the length of surgery, the length of stay, SFR, need for retreatment, the dosage of painkiller consumption, and complications rate were gathered and compared between 2 groups. Stone-free rate was calculated based on outcomes of immediate and 3-month postoperative imaging, including kidney, ureter, and bladder (KUB) or computed tomography (CT) scan. The period between puncturing for access to the track and the nephrostomy insertion was considered operation time. Although a KUB X-ray was done on all the patients, the size and location of patients’ stones were assessed using a CT scan performed on the first post-operation day and 3-months follow-up. Stone-free was defined as the absence of residual fragments on postoperative imaging. The maximum stone diameter on the CT scan was considered the stone size. All the patients who had positive urine culture results underwent suitable antibiotic therapy before the surgery, and after negative urine culture results, the surgery was done for them.
The RIRS was done after inducing general anesthesia; the procedure was carried out on patients in group 2 in the dorsal lithotomy position. First of all, a cystoscopy was performed, and after that, under C-arm fluoroscopic guidance, a hydrophilic guidewire was placed within the ureteral orifice into the renal pelvis with full precaution to prevent mucosa injury. Meanwhile, the dilation of the ureter was maintained by ureteroscopy. Then, the surgeon placed a ureteral access sheath (9.5 - 11.5 Fr) over the mentioned guidewire at the level of the ureteropelvic junction. Once a flexible ureteroscope was passed through the access sheath, stones were fragmented by utilizing a YAG laser called holmium, and finally, double-J stents were inserted in all the patients. A 273 μm laser fiber was used, Holmium machine energy was set at 0.6 to 1.5 J, and frequency was set at 8 - 10 Hz. Although a ureteral access sheath could not be inserted in 2 of our cases, we successfully proceeded with the process without a ureteral access sheath. In one of our patients, we could not pass the flexible ureteroscope into the renal pelvis; we inserted a double-J stent and postponed the surgery for 2 weeks.
Percutaneous nephrolithotomy procedure was performed on patients of group 1 initially after anesthesiologist-induced general anesthesia. Access was obtained through C-arm fluoroscopy using an 18 gauge needle prone, similar to the standardized method described in a previous study (15). After inducing dilation of the tract with a high-pressure balloon dilator (NephromaxTM Microvasive, Boston Scientific, Natick, MA, USA), stone fragmentation was performed using pneumatic/ultrasonic lithotrite (Swiss LithoClast Ultra®, Boston Scientific). When the procedure was accomplished, a 24 F nephrostomy tube was inserted into the collecting system for drainage.
3.1. Statistical Analysis
The continuous variables are reported using the mean ± standard deviation, and the t-test compares these variables between the groups. Moreover, the discrete variables are reported as numbers (%) using the chi-squared test, and their distribution is reached between the 2 groups. The logistic and linear regression models are fitted to binary and continuous response variables. The analyses were performed using the statistical software Stata (ver. 13), and the significance level was set to 0.05.
4. Results
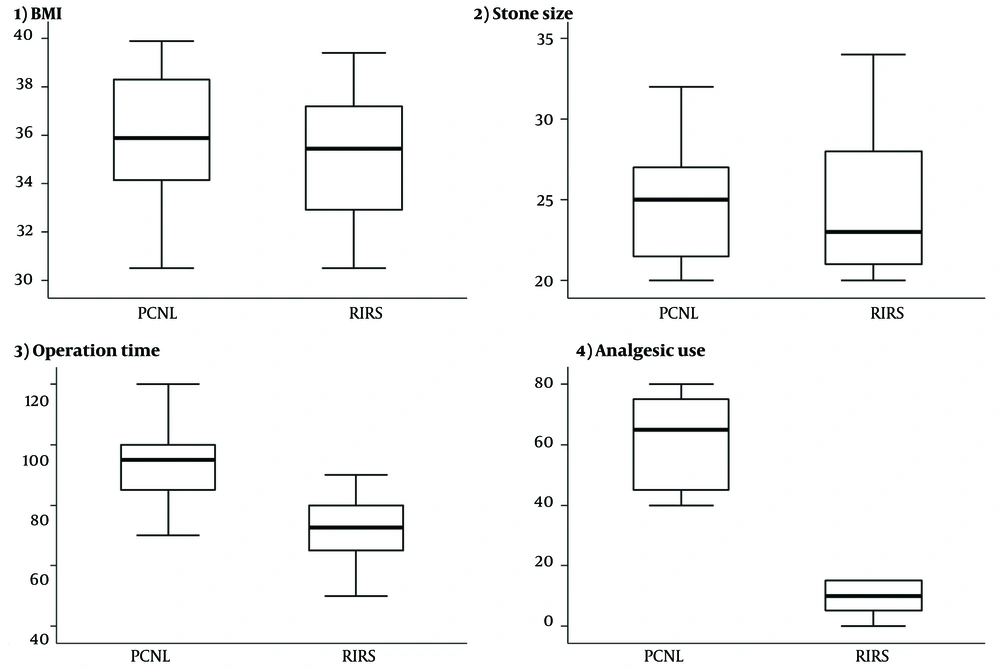
The baseline characteristics in terms of age, sex, BMI, stone size, stone location, and stone composition were compared in Table 1 between the treatment groups. Stone analysis was performed on 36 patients of the PCNL and 38 patients of the RIRS group (Figure 1).
| Variables | Group | P-Value | |
|---|---|---|---|
| Percutaneous Nephrolithotomy | Retrograde Intrarenal Surgery | ||
| Gender (male) | 19 (47.5) | 20 (47.6) | 0.991 b |
| Age (y) | 52.5 ± 15.9 | 53.3 ± 15.8 | 0.818 c |
| Body mass index (kg/m2) | 36.0 ± 2.7 | 35.2 ± 2.6 | 0.142 c |
| Stone size (cm) | 25.2 ± 3.8 | 24.4 ± 4.0 | 0.348 * |
| Stone location | 0.877 b | ||
| Upper | 10 (25.0) | 13 (31.7) | |
| Middle calyx | 11 (27.5) | 9 (22.0) | |
| Lower calcium | 5 (12.5) | 4 (9.8) | |
| Pelvic | 14 (35.0) | 15 (36.6) | |
| Stone composition | 0.702 b | ||
| Calcium oxalate monohydrate | 25 (73.5) | 27 (71.1) | |
| Calcium oxalate dihydrate | 7 (20.6) | 5 (13.2) | |
| Cystine | 0 (0.0) | 2 (5.3) | |
| Struvite | 1 (2.9) | 2 (5.3) | |
| Uric acid | 1 (2.3) | 2 (5.3) | |
A Description of the Measured Variables a
Stone-free rate, preoperative and postoperative data between the 2 groups are compared in Table 2. The hospitalization stays for the majority of the RIRS group (78.6%) was 1 day and for the rest of them (21.4%) was more than 1 day which in patients of the PCNL group was more than 1 day, and this difference between 2 groups was significant (P < 0.001). The mean operation time for the RIRS and PCNL groups was 71.6 ± 11 and 93.3 ± 12.2, respectively, which was statically significant between the 2 groups (P < 0.001). The mean of analgesic use in the PCNL group was significantly greater than in the RIRS group (P < 0.001). Regarding post-operation complications, differences were detected between the 2 groups, but none were statically significant. Two of 40 patients of the PCNL group and 8 of 42 patients of the RIRS group had a postoperative fever. Of those, 4 patients in the RIRS group and 1 in the PCNL group had sepsis. For patients who presented with only fever, antibiotics were given instantly, and for patients with urosepsis after admission to the intensive care unit, intravenous antibiotics were given immediately. No mortality was observed. No acute re-admissions took place. No creatinine rise was seen in patients of both groups. Two patients in the PCNL group needed a blood transfusion during surgery. However, none in the RIRS group needed it. Angio infarction has occurred only in 1 patient in the PCNL group. Creatinine levels were not rising in either the RIRS or PCNL groups. There was no ureteric injury during the surgery, and there were no cases of hydronephrosis or stricture at the 3-month follow-up.
| Variables | Group | P-Value | |
|---|---|---|---|
| Percutaneous Nephrolithotomy | Retrograde Intrarenal Surgery | ||
| Stone-free rate (yes) | 38 (95.0) | 39 (92.9) | 0.523 b |
| Hospital stay (days) | < 0.001 | ||
| 1 | 0 (0.0) | 33 (78.6) | |
| > 1 | 40 (100.0) | 9 (21.4) | |
| Operation time (min) | 93.0 ± 12.2 | 71.6 ± 11.0 | < 0.001c |
| Analgesic use (g) | 61.8 ± 13.6 | 9.0 ± 5.5 | < 0.001c |
| Transfusion (yes) | 2 (5.0) | 0 (0.0) | 0.235 b |
| Fever (yes) | 2 (5.0) | 8 (19.1) | 0.089 b |
| Sepsis (yes) | 1 (2.5) | 4 (9.5) | 0.360 b |
| Angio-infarction (yes) | 1 (2.5) | 0 (0.0) | 0.488 b |
| Resurgery (yes) | 2 (5.0) | 1 (2.4) | 0.611 b |
Comparison of Stone-free Rate, Preoperative and Postoperative Data of Retrograde Intrarenal Surgery and Percutaneous Nephrolithotomy Group
After a single procedure session, the SFR for the PCNL group was 95% and for the RIRS group was 92.9%. One patient in the RIRS group and 2 patients in the PCNL group needed a second surgery, and at last, after 3 months of follow-up, SFR improved to 97.5% for the PCNL group and 95.2% for the RIRS group.
The logistic regression model was applied to the binary outcome, SFR, comparing the 2 groups. Age, gender, and BMI were adjusted in this model, and none was significant. No difference was found between the 2 groups, taking the PCNL as the reference group (OR = 0.35, P-value = 0.237). Moreover, regarding the continuous outcome operation time, the linear regression model was fitted. Adjusted for age, gender, and BMI, the RIRS group’s operation times were, on average, 21.5 minutes less than the PCNL group’s (P-value < 0.001). As a minor point, age was the only significant covariate; each 10-year increase in age increased the operation time by 1.8 minutes (P-value = 0.033). Similarly, none of the covariates were significant, fitting the linear model on the amount of analgesic use. In contrast, on average, the RIRS group’s analgesic use was 52.6 grams less than the PCNL group’s (P-value < 0.001).
5. Discussion
To the best of our knowledge, this is the first study that evaluated the differences between PCNL and RIRS in terms of patients and kidney stones characteristics and operative and postoperative outcomes in obese patients (BMI between 30 and 40 kg/m2) whose kidney stones with the size between 2 cm and 4 cm. Our results demonstrated no significant differences between the 2 groups other than the dosage of painkillers, the length of stay, and the length of surgery that RIRS had superiority over PCNL.
Albeit, the standard treatment for managing many kidney stones larger than 2 cm and complex stones is PCNL (15, 16), which has an association with detrimental complications and hampered wide usage of that. The notable advancements in the new flexible ureteroscope both increase the efficacy of these tools and lower complication rates (17, 18). Although several studies have been dedicated to comparing the effectiveness of PCNL and shock wave lithotripsy concerning kidney stones management (19-21), there is a lack of studies comparing the outcomes of PCNL and RIRS in this regard (22, 23).
Promising successful rates regarding applying RIRS in patients with stones larger than 2 cm have been reported in former studies (5, 24-27). For instance, El-Anany et al. performed RIRS on 30 patients with stones > 2 cm, and 23 (77%) of 30 patients were free of stones after surgery (26). A study on 51 patients with 161 intrarenal stones (July 2000 to April 2006) in the USA showed that overall SFR after the first and second RIRS was about 64.7% and 92.2%, respectively. The overall SFR for stones less than and more significant than 2 cm was 100% and 85.1%, respectively (25). Riley et al. sought to show the efficacy of RIRS in 22 patients with stones larger than 2.5 cm (27). In their study, 5 patients after 1, 14 patients after 2, and 1 patient after 3 procedures were free of renal stones, and 2 patients failed to respond to RIRS, so they underwent PCNL (27). As we can see, after the second session of RIRS, RIRS -SFRs are comparable with PCNL-SFRs, and the success rates of RIRS are approximately similar to PCNL.
Only a few studies have compared the efficacy of RIRS and PCNL regarding renal stones management. Chung et al. designed a study to compare the outcome of PCNL and RIRS in 27 patients with 1 - 2 cm renal stones (22). 15 of 27 underwent PCNL, and 12 of 27 experienced RIRS without additional sessions in 8 months. Last, SFR for PCNL and RIRS were 87% and 67%, respectively, but this difference was not statistically significant (22). Akman et al. showed that the SFR of PNCL and RIRS were significantly different (91.2% and 73.5%, respectively) in non-obese patients with 2 - 4 cm renal stones of different compositions (4). The successful PCNL and RIRS in the Paul et al.’s study were 84.8% and 88.6%, respectively (28). In the current study, after a single procedure, the SFR for PCNL was about 95% and for RIRS was 92%, which was higher than in recent studies.
Treatments of patients with obesity have been challenging for doctors, especially urologists. The role of obesity in increasing the rate of renal stone formation, mainly in high-income countries, has been well-validated (29). It has been postulated that patients with obesity, compared to patients with non-obesity, are more prone to surgical complications following the procedure and show a higher mortality rate (30). Heterogeneous findings have appeared in studies that evaluated the influence of BMI on the outcome of different methods of renal stone management (13, 14, 31). Torrecilla Ortiz et al. designed a study to evaluate the efficacy and complications of PCNL in obese patients compared to non-obese patients (31). They showed that statistically, there is no difference between the group’s increase in complications and SFR (31). In the study of Fuller et al., PCNL in obese patients resulted in lower SFR and higher operation time (13). On the contrary, in Olbert et al., patients with higher BMI were more susceptible to being stone-free than non-obese patients (14).
Our study’s mean operation times for the PCNL and RIRS groups were approximately 93.0 ± 12.2 and 71.6 ± 11.0, respectively. The mean operation time of PCNL and RIRS for patients with 2 - 4 cm renal stones was 58.2 ± 13.4 and 38.7 ± 11.6 min, respectively (4). Several studies have investigated the association between the complications of PCNL and the mean operation time. Akman et al. pointed out that if the operation time last more than 58 minutes in patients who are treated with PCNL, the chance of blood transfusion increases 2.82 times during surgery (32) and also, and Keoghae et al. illustrated that increase in operation time of PCNL raises the odds of blood transfusion (33). In contrast to PCNL, as far as we know, the need for blood transfusion during the RIRS procedure has not been reported in former studies (34), and similarly, in our study, no patient in the RIRS group needed a blood transfusion. However, 2 of the PCNL group required that.
Hospital stay in the PCNL group was significantly higher than in the RIRS group. This difference can be explained by some reasons, including necessitating catheter insertion for drainage and following patients following blood transfusion in patients of the PCNL group (28). Recent studies show that performing PCNL procedures without a tube significantly decreases hospital duration (35, 36). In the present study, hospital stay in the RIRS group were significantly shorter than in the PCNL group, similar to the outcomes of relevant studies (34, 35).
In our study, urosepsis occurred in 9.5% of the RIRS group and 2.5% of the PCNL group. This procedure complication happened at a higher rate in our study compared to previous studies (4, 37). It has been shown that operating time is one of the leading independent risk factors of infection in patients who undergo RIRS, and precaution should be exercised in surgeries that last more than 1 hour (38). Hence, our patients’ higher incidence of urosepsis can be attributed to longer operation times. The main reason for longer operation time is obesity, which can be a risk factor for longer operation duration (13).
We acknowledge that our study had some limitations. First, it was a single-center, retrospective study with a limited number of patients and a short follow-up (3 months). Therefore, a multicentric investigation with large sample sizes is warranted. Second, the patient’s pain score was not assessed, mainly due to the nephrostomy tube in the patients in the PCNL group. Despite those, the first study compares the efficacy and complications of RIRS and PCNL in obese patients with 2 - 4 cm renal stones.
5.1. Conclusions
To treat renal stones with CT diameter between 2 - 4 cm in patients with BMI between 30 and 40, in terms of SFR, post-operation complications, need for blood transfusion, and surgery, there was no difference between PCNL and RIRS. However, the RIRS group had significantly lower operation time, analgesic use, and hospitalization duration than the PCNL group. Moreover, according to the high rates of SFR in both groups, it can be concluded that the outcomes of RIRS and PCNL would be satisfactory.