1. Background
Infertility is described as the unsuccessful attempt to conceive after at least 12 months of sexual intercourse without using contraception (1). Infertility leads to significant psychological, economic, and medical problems, particularly in societies that have a high emphasis on fertilization (2). Based on recent epidemiological findings, the lifetime prevalence of infertility is 17.5% (3). The results of a worldwide analysis published in 2022 show that men residing in the Middle East and North Africa have experienced a rising trend in primary and secondary infertility prevalence rates during the last decades (4). According to a meta-analysis published in 2023, the prevalence of primary infertility was 18.3% among Iranian couples; furthermore, 2.5% of the population was estimated to be struggling with secondary infertility (5).
Infertility is divided into two types: Primary if the couple has never had a child and secondary if they have experienced conception before. Two-thirds of cases are estimated to be primary fertility, with an average period of infertility reported as 5.6 years (1). Infertility can occur due to female, male, or combined causes. In some cases, no particular cause is determined for infertility (6). Female factors, including tubal pathology, polycystic ovarian syndrome, uterine malformations, and endocrine abnormalities, account for 42.8% to 46.6% of infertility causes (6, 7). Male factor is the only cause of infertility in 10% to 35.5% of couples (6, 7). Additionally, 10.8% to 18.4% of cases have a combined reason (6, 7). In 3.4% to 32.5% of couples, the cause of infertility was not identified (6, 7).
Various factors are known to be associated with male infertility. Hypogonadism, genetic defects of the Y chromosome, neoplasms, cryptorchidism, varicocele, and infections are some known factors (8). Sperm concentration, motility, and morphology play an essential role in male fertility; as a result, semen analysis is considered a valuable test for evaluating male fertility (2). Several studies have reported a decline in semen concentration and morphology during the past years. A significant decrease of 32.2% in sperm concentration was observed between 1989 to 2005 (9). Some infertile men can show normal semen parameters, which suggests the need for further investigations. Furthermore, with the emerging modern assisted reproductive technology, new methods are required to meet the needs of reproductive practice (10).
The DNA fragmentation index (DFI) is considered a remarkable indicator for assessing male fertility. It reflects the integrity of sperm DNA, thereby identifying sperm damage (10-12). Couples with no known infertility problem and a male DFI of < 30% are estimated to have a 7.0-time chance of pregnancy (13). Different factors, including cigarette smoking, increasing age, elevated body mass index (BMI), and mobile phone radiation, have been hypothesized to be correlated with sperm DNA integrity (11). Many researchers have investigated the association between these environmental and lifestyle factors and semen parameters, including the DFI (14, 15). Nevertheless, data are scarce on the role of lifestyle factors in infertility in Khorramabad, Iran.
2. Objectives
This study aimed to evaluate the association between demographic characteristics and sperm DFI in 222 infertile men admitted to two urology clinics in Khorramabad, Iran.
3. Methods
3.1. Study Design and Participants
This cross-sectional descriptive study was performed on 222 infertile men referred to the Urology Clinic of Shohada-ye Ashayer and Shahid Rahimi hospitals of Khorramabad from 2021 to 2022. The inclusion criteria were male infertility and consent to participation in the study. The exclusion criteria were andrological disorders with confirmed effects on sperm quality, including genetic diseases of the sex chromosome, a previous history of mumps orchitis, undescended testis, high-grade varicocele, history of testicular torsion or scrotal damage, congenital bilateral absence of vas deferens, taking medications with known effects on semen, drug abuse, history of malignancy, and mental disorders.
3.2. Data Collection
After obtaining informed consent from the subjects and ensuring that their personal information would be confidential, sperm DFI was measured in all patients. The sperm sample was collected after 5 days of non-ejaculation and combined with chemicals, such as acridine orange. Damaged single-stranded DNA emits red fluorescent in combination with this substance, and healthy DNA emits green fluorescent. At least five thousand sperm are counted, and the number of sperm that emits red rays is determined, thereby obtaining the DFI (16). Based on sperm DFI levels, the subjects were divided into three groups: (1) patients with a DFI < 15%; (2) patients with a DFI level of 15 - 30%; and (3) patients with a DFI > 30%. Then, the potential risk factors, including alcohol consumption, smoking, BMI, and age, were studied in each group.
3.3. Data Analysis
The data collected were analyzed using SPSS software (version 22). To achieve the descriptive objectives of the study, the calculation of frequency, mean, standard deviation, and contingency tables were used considering the variable type. To achieve the analytical objectives, the chi-square test was used to assess the association between smoking and alcohol consumption with the DFI, and the one-way analysis of variance (ANOVA) test was used to compare the mean age and BMI in the three studied groups. The significance level was considered less than 0.05.
3.4. Ethical Considerations
This study was conducted with the permission of the Research Ethics Committee of Lorestan University of Medical Sciences, Khorramabad, Iran, with the ethical code IR.LUMS.REC.1400.265. Written consent was obtained from all the patients. The checklists were designed anonymously to observe the principle of confidentiality.
4. Results
In this study, 222 men with infertility were included. The mean age of the patients was 37.45 ± 5.99 years, with a minimum and maximum age of 27 and 60 years, respectively. Regarding age, 163 individuals (73.4%) were ≤ 35 years. Moreover, 94 patients (42.3%) were smokers, and 52 cases (23.4%) mentioned alcohol consumption. In terms of BMI, 115 subjects (51.8%) were within the range of 18.6 - 24.9 kg/m2 (Table 1).
| Variables | Frequency (%) |
|---|---|
| Age (y) | |
| ≤ 35 | 163 (73.4) |
| > 35 | 59 (26.6) |
| Smoking | |
| Yes | 94 (42.3) |
| No | 128 (57.7) |
| Alcohol consumption | |
| Yes | 52 (23.4) |
| No | 170 (76.6) |
| BMI (kg/m2) | |
| ≤ 18.5 | 1 (0.5) |
| 18.6 - 24.9 | 115 (51.8) |
| 25 - 29.9 | 90 (40.5) |
| ≥ 30 | 16 (7.2) |
Abbreviation: BMI, body mass index.
The DFI was < 15%, 15 - 30%, and 30% < in 119 (53.6%), 69 (31.1%), and 34 (15.3%) individuals, respectively. The data on the association of smoking and alcohol consumption with DFI are listed in Table 2.
Abbreviation: DFI, DNA fragmentation index.
a Chi-square test.
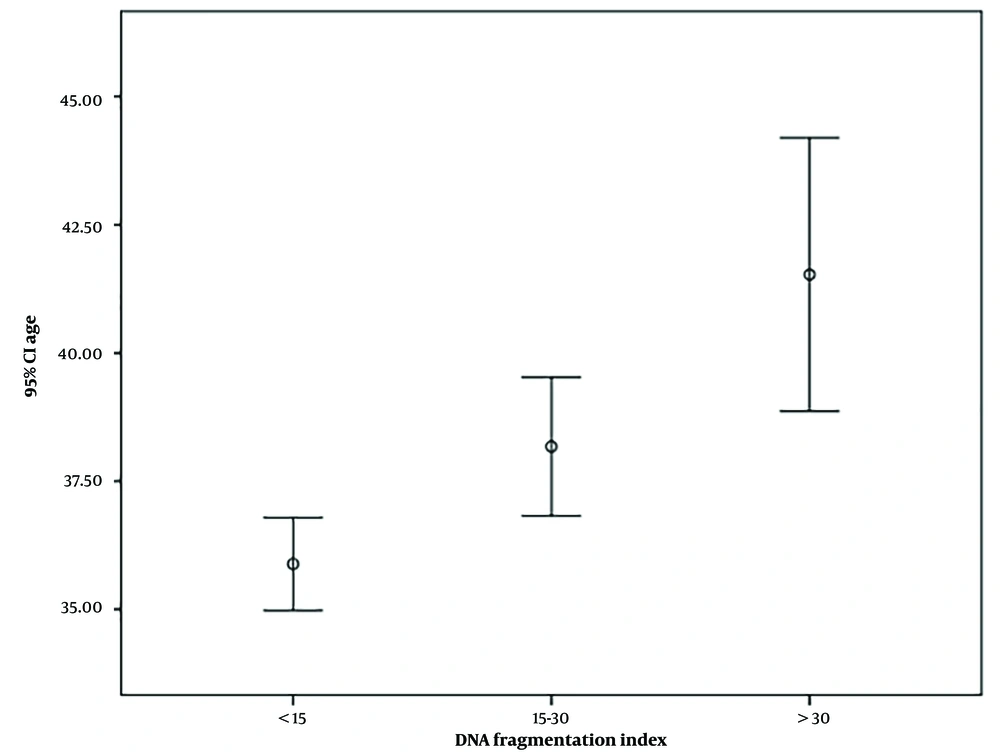
There was no statistically significant relationship between smoking and alcohol consumption with the DFI (P > 0.05). The mean age in the three DFI groups of less than 15%, 15 - 30%, and more than 30% was 35.88, 38.17, and 41.52 years, respectively, indicating a statistically significant difference (P < 0.05) (Table 3). However, there was no statistically significant relationship between BMI and DFI (P > 0.05) (Table 4).
| DFI | No | Mean ± SD | F | df | P-Value |
|---|---|---|---|---|---|
| < 15% | 119 | 35.88 ± 5.00 | 13.906 | 2 | 0.001 a |
| 15 - 30% | 69 | 38.17 ± 5.63 | |||
| > 30% | 34 | 41.52 ± 7.64 | |||
| Total | 222 | 37.45 ± 5.99 |
Abbreviations: DFI, DNA fragmentation index; SD, standard deviation; ANOVA, analysis of variance.
a One-way ANOVA.
| DFI | No | Mean ± SD | F | df | P-Value |
|---|---|---|---|---|---|
| < 15% | 119 | 24.84 ± 3.89 | 1.291 | 2 | 0.277 a |
| 15 - 30% | 69 | 25.57 ± 2.87 | |||
| > 30% | 34 | 24.61 ± 2.54 | |||
| Total | 222 | 25.03 ± 3.42 |
Abbreviations: DFI, DNA fragmentation index; SD, standard deviation; ANOVA, analysis of variance.
a One-way ANOVA.
Figure 1 illustrates the mean age of the study population based on the DFI. As can be seen, higher DFIs are accompanied by a higher mean (95% confidence interval) age.
5. Discussion
It is suggested to perform a sperm DFI assay in addition to routine tests in evaluating male fertility (17). The association between lifestyle factors and the DFI has been widely reported (14). The authors of the present study believed that if a strong link was confirmed between these factors and sperm DFI, public health strategies could be made to prevent and eliminate these habits among the general population; therefore, this study was conducted to evaluate these potential risk factors.
In the current study, the mean age of patients was 37.45 ± 5.99 years, and 73.4% of patients were younger than 35 years. Previous studies have shown a mean age ranging from 27.83 to 46.6 years among male partners of couples suffering from infertility (18, 19). The discrepancy observed in the mean age of infertile men from different regions can be justified by differences in genetic and environmental factors between populations. In some areas, low health insurance coverage can also play a role as it might make it financially infeasible for some individuals, particularly younger couples, to seek fertility care. Traditionally, aging is believed to play a principal role in diminishing sperm quality. Different factors, such as the degeneration of the urogenital tract, a decrease in the number of Leydig cells, and more exposure to exogenous toxicants, can contribute to lower semen quality in older men (20).
In the current study, 15.3% of the subjects had a DFI of more than 30%. Al Omrani et al. reported that 13.83% of infertile men had high DFI in the Saudi population (21). The present study demonstrated a significant difference between the mean age in the three studied groups. The group with a higher mean age had a higher DFI. Radwan et al. showed that the age category of older than 40 years was correlated with a higher DFI (11). The underlying causes of sperm DNA impairment in older men are unclear. However, some mechanisms, such as oxidative stress and impaired sperm chromatin packaging, have been suggested (22). Oxidative stress associated with paternal aging results in inflammation and endocrine dysfunction and subsequently hinders spermatogenesis (20).
In the present study, 51.8% of the patients had a normal BMI. The mean BMI was 27.01 in an analysis performed by Ajayi et al. Additionally, they reported lower semen volume, sperm count, and motility in obese men than those with normal weight (23). The current study’s results showed no significant relationship between BMI and DFI in the studied population. Bandel et al. performed a cross-sectional study on 1503 men in the general population. They did not confirm a positive relationship between high BMI and sperm DNA damage (14). On the other hand, Kort et al. showed a positive relationship between BMI and DFI; as the subjects’ BMI increased beyond 25 kg/m2, the DFI also rose (24).
In the present study, no noticeable relationship was observed between smoking and DFI. Sepaniak et al. showed that smokers had a significantly higher DFI than non-smokers (32% versus 25.9%) (25). This finding is inconsistent with the findings of the current study and a study performed by Radwan et al., where they showed no association between smoking and sperm DNA damage (11).
In the current study, there was no considerable correlation between alcohol consumption and DFI. Similarly, Rios et al. demonstrated no relationship between increased sperm DFI and alcohol use in a study on 147 infertile men (26). In addition, Shi et al. showed that the alcohol drinking index was not significantly correlated with any of the evaluated sperm parameters in their study (15). The aforementioned results differ from the results of Komiya et al.’s study. They concluded that in those with chronic alcohol use, sperm DFI is higher than in nondrinkers (27).
Based on the present study’s results, age is the only demographic variable that affects male fertility, and lifestyle factors might not have an influential role in the occurrence of infertility. Therefore, theoretically, lifestyle modification might not be effective in the prevention or treatment of male infertility. At the clinical level, the findings of the present study insinuate the potential benefits of the DFI measurement in the evaluation of infertile men aged over 35 years.
5.1. Limitations
This study has specific strengths, including evaluating both unmodifiable factors (i.e., age) and modifiable factors (i.e., BMI, smoking, and alcohol consumption) in a relatively large sample size. At the same time, most similar studies studied fewer variables or had smaller sample sizes. However, there were also some limitations to this study. The first one is the couples’ reluctance to participate, particularly men denying infertility due to cultural misconceptions. Furthermore, as many infertile couples had been referred to various practitioners before participating in this study, it was challenging to convince them to give a detailed history over again.
5.2. Conclusions
There was no significant relationship between lifestyle factors and DFI. However, large-scale studies are required to evaluate the role of these factors, as if their role in infertility is proven, lifestyle modification might be a potential method for managing infertility.